Abstract
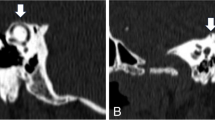
Superior semicircular canal dehiscence (SSCD) is an example of a “third mobile window” (TMW) condition resulting from dehiscence of middle fossa bone over the superior semicircular canal [1]. While not as well characterized as SSCD, other foci of otic capsule dehiscence have also been described, including the posterior semicircular canal, vestibular aqueduct, internal auditory canal, carotid canal, and fallopian canal [2–7]. TMWs allow aberrant sound and energy transfer through the inner ear, leading to classic findings of mixed hearing loss, autophony and vestibular dysfunction. Less specific symptoms, including pulsatile tinnitus, headache, hyperacusis and visual disturbance, may also be present, resulting in difficulty distinguishing TMW conditions from other entities, including migraine variants and idiopathic intracranial hypertension (IIH) [8].
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Minor LB, Solomon D, Zinreich JS, Zee DS. Sound- and/or pressure-induced vertigo due to bone dehiscence of the superior semicircular canal. Arch Otolaryngol Neck Surg. 1998;124(3):249. https://doi.org/10.1001/archotol.124.3.249.
Merchant SN, Nakajima HH, Halpin C, et al. Clinical investigation and mechanism of air-bone gaps in large vestibular aqueduct syndrome. Ann Otol Rhinol Laryngol. 2007;116(7):532–41. https://doi.org/10.1177/000348940711600709.
Blake DM, Tomovic S, Vazquez A, Lee HJ, Jyung RW. Cochlear-facial dehiscence—a newly described entity. Laryngoscope. 2014;124(1):283–9. https://doi.org/10.1002/lary.24223.
Karlberg M, Annertz M, Magnusson M. Mondini-like malformation mimicking otosclerosis and superior semicircular canal dehiscence. J Laryngol Otol. 2006;120(5):419–22. https://doi.org/10.1017/S0022215106000934.
Kim HHS, Wilson DF. A third mobile window at the cochlear apex. Otolaryngol Head Neck Surg. 2006;135(6):965–6. https://doi.org/10.1016/j.otohns.2005.04.006.
Lund AD, Palacios SD. Carotid artery-cochlear dehiscence: a review. Laryngoscope. 2011;121(12):2658–60. https://doi.org/10.1002/lary.22391.
Reynard P, Idriss S, Ltaief-Boudrigua A, et al. Proposal for a unitary anatomo-clinical and radiological classification of third mobile window abnormalities. Front Neurol. 2022;12:792545. https://doi.org/10.3389/fneur.2021.792545.
Naert L, Berg R, Heyning P, et al. Aggregating the symptoms of superior semicircular canal dehiscence syndrome. Laryngoscope. 2018;128(8):1932–8. https://doi.org/10.1002/lary.27062.
Takahashi N, Tsunoda A, Shirakura S, Kitamura K. Anatomical feature of the middle cranial fossa in fetal periods: possible etiology of superior canal dehiscence syndrome. Acta Otolaryngol (Stockh). 2012;132(4):385–90. https://doi.org/10.3109/00016489.2011.637234.
Crovetto M, Whyte J, Rodriguez OM, Lecumberri I, Martinez C, Eléxpuru J. Anatomo-radiological study of the superior semicircular canal dehiscence. Eur J Radiol. 2010;76(2):167–72. https://doi.org/10.1016/j.ejrad.2009.05.038.
Carey JP, Minor LB, Nager GT. Dehiscence or thinning of bone overlying the superior semicircular canal in a temporal bone survey. Arch Otolaryngol Neck Surg. 2000;126(2):137. https://doi.org/10.1001/archotol.126.2.137.
Tóth M, Helling K, Baksa G, Mann W. Localization of congenital Tegmen Tympani defects. Otol Neurotol. 2007;28(8):1120–3. https://doi.org/10.1097/MAO.0b013e31815aee0c.
Zhou G, Gopen Q, Poe DS. Clinical and diagnostic characterization of canal dehiscence syndrome: a great otologic mimicker. Otol Neurotol. 2007;28(7):920–6. https://doi.org/10.1097/MAO.0b013e31814b25f2.
Davey S, Kelly-Morland C, Phillips JS, Nunney I, Pawaroo D. Assessment of superior semicircular canal thickness with advancing age: SSC thickness and age. Laryngoscope. 2015;125(8):1940–5. https://doi.org/10.1002/lary.25243.
Berkiten G, Gürbüz D, Akan O, et al. Dehiscence or thinning of bone overlying the superior semicircular canal in idiopathic intracranial hypertension. Eur Arch Otorhinolaryngol. 2022;279:2899. https://doi.org/10.1007/s00405-021-07020-z.
Handzel O, Brenner-Ullman A, Niry D, et al. Tegmen attenuation in patients with idiopathic intracranial hypertension is progressive. Laryngoscope. 2020;130(12):E904. https://doi.org/10.1002/lary.28490.
Watters KF, Rosowski JJ, Sauter T, Lee DJ. Superior semicircular canal dehiscence presenting as postpartum vertigo. Otol Neurotol. 2006;27(6):756–68. https://doi.org/10.1097/01.mao.0000227894.27291.9f.
Kuo P, Bagwell KA, Mongelluzzo G, et al. Semicircular canal dehiscence among idiopathic intracranial hypertension patients: SSCD among IIH patients. Laryngoscope. 2018;128(5):1196–9. https://doi.org/10.1002/lary.26795.
Schutt CA, Neubauer P, Samy RN, et al. The correlation between obesity, obstructive sleep apnea, and superior semicircular canal dehiscence: a new explanation for an increasingly common problem. Otol Neurotol. 2015;36(3):551.
Nadgir RN, Ozonoff A, Devaiah AK, Halderman AA, Sakai O. Superior semicircular canal dehiscence: congenital or acquired condition? Am J Neuroradiol. 2011;32(5):947–9. https://doi.org/10.3174/ajnr.A2437.
McCluskey G, Mulholland DA, McCarron P, McCarron MO. Idiopathic intracranial hypertension in the northwest of northern Ireland: epidemiology and clinical management. Neuroepidemiology. 2015;45(1):34–9. https://doi.org/10.1159/000435919.
Miah L, Strafford H, Fonferko-Shadrach B, et al. Incidence, prevalence, and health care outcomes in idiopathic intracranial hypertension: a population study. Neurology. 2021;96(8):e1251–61. https://doi.org/10.1212/WNL.0000000000011463.
Radhakrishnan K, Ahlskog JE, Cross SA, Kurland LT, O’Fallon WM. Idiopathic intracranial hypertension (Pseudotumor cerebri). Descriptive epidemiology in Rochester, Minn, 1976 to 1990. Arch Neurol. 1993;50(1):78–80. https://doi.org/10.1001/archneur.1993.00540010072020.
Durcan FJ, Corbett JJ, Wall M. The incidence of pseudotumor cerebri. Population studies in Iowa and Louisiana. Arch Neurol. 1988;45(8):875–7. https://doi.org/10.1001/archneur.1988.00520320065016.
Wall M. Idiopathic intracranial hypertension (pseudotumor cerebri). Curr Neurol Neurosci Rep. 2008;8(2):87–93.
Jindal M, Hiam L, Raman A, Rejali D. Idiopathic intracranial hypertension in otolaryngology. Eur Arch Otorhinolaryngol. 2009;266(6):803–6. https://doi.org/10.1007/s00405-009-0973-0.
De Simone R, Ranieri A, Bonavita V. Advancement in idiopathic intracranial hypertension pathogenesis: focus on sinus venous stenosis. Neurol Sci. 2010;31(Suppl 1):S33–9. https://doi.org/10.1007/s10072-010-0271-z.
Kim SW, Choi JH. Cerebrospinal fluid otorrhea caused by arachnoid granulation. Korean J Audiol. 2012;16(3):152–5. https://doi.org/10.7874/kja.2012.16.3.152.
Gacek RR. Arachnoid granulation cerebrospinal fluid otorrhea. Ann Otol Rhinol Laryngol. 1990;99(11):854–62. https://doi.org/10.1177/000348949009901102.
Yew M, Dubbs B, Tong O, et al. Arachnoid granulations of the temporal bone: a histologic study of dural and osseous penetration. Otol Neurotol. 2011;32(4):602–9. https://doi.org/10.1097/MAO.0b013e3182129026.
Bruce BB, Kedar S, Van Stavern GP, et al. Idiopathic intracranial hypertension in men. Neurology. 2009;72(4):304–9. https://doi.org/10.1212/01.wnl.0000333254.84120.f5.
Sugerman HJ, Felton WL, Salvant JB, Sismanis A, Kellum JM. Effects of surgically induced weight loss on idiopathic intracranial hypertension in morbid obesity. Neurology. 1995;45(9):1655–9. https://doi.org/10.1212/wnl.45.9.1655.
Hannerz J, Greitz D, Ericson K. Is there a relationship between obesity and intracranial hypertension? Int J Obes Relat Metab Disord. 1995;19(4):240–4.
Kupersmith MJ, Gamell L, Turbin R, Peck V, Spiegel P, Wall M. Effects of weight loss on the course of idiopathic intracranial hypertension in women. Neurology. 1998;50(4):1094–8. https://doi.org/10.1212/wnl.50.4.1094.
Hannerz J, Ericson K. The relationship between idiopathic intracranial hypertension and obesity. Headache. 2009;49(2):178–84. https://doi.org/10.1111/j.1526-4610.2008.01240.x.
Nedelmann M, Kaps M, Mueller-Forell W. Venous obstruction and jugular valve insufficiency in idiopathic intracranial hypertension. J Neurol. 2009;256(6):964–9. https://doi.org/10.1007/s00415-009-5056-z.
Friedman DI. The pseudotumor cerebri syndrome. Neurol Clin. 2014;32(2):363–96. https://doi.org/10.1016/j.ncl.2014.01.001.
Bloomfield GL, Ridings PC, Blocher CR, Marmarou A, Sugerman HJ. A proposed relationship between increased intra-abdominal, intrathoracic, and intracranial pressure. Crit Care Med. 1997;25(3):496–503. https://doi.org/10.1097/00003246-199703000-00020.
Michaelides EM, Sismanis A, Sugerman HJ, Felton WL. Pulsatile tinnitus in patients with morbid obesity: the effectiveness of weight reduction surgery. Am J Otol. 2000;21(5):682–5.
Kesler A, Kliper E, Assayag EB, et al. Thrombophilic factors in idiopathic intracranial hypertension: a report of 51 patients and a meta-analysis. Blood Coagul Fibrinolysis Int J Haemost Thromb. 2010;21(4):328–33. https://doi.org/10.1097/MBC.0b013e328338ce12.
Markey KA, Uldall M, Botfield H, et al. Idiopathic intracranial hypertension, hormones, and 11β-hydroxysteroid dehydrogenases. J Pain Res. 2016;9:223–32. https://doi.org/10.2147/JPR.S80824.
Botfield HF, Uldall MS, Westgate CSJ, et al. A glucagon-like peptide-1 receptor agonist reduces intracranial pressure in a rat model of hydrocephalus. Sci Transl Med. 2017;9(404):eaan0972. https://doi.org/10.1126/scitranslmed.aan0972.
Higgins JNP, Pickard JD. Lateral sinus stenoses in idiopathic intracranial hypertension resolving after CSF diversion. Neurology. 2004;62(10):1907–8. https://doi.org/10.1212/01.wnl.0000125285.44539.d7.
Ahmed RM, Wilkinson M, Parker GD, et al. Transverse sinus stenting for idiopathic intracranial hypertension: a review of 52 patients and of model predictions. AJNR Am J Neuroradiol. 2011;32(8):1408–14. https://doi.org/10.3174/ajnr.A2575.
Eisenman DJ. Sinus wall reconstruction for sigmoid sinus diverticulum and dehiscence: a standardized surgical procedure for a range of radiographic findings. Otol Neurotol. 2011;32(7):1116–9. https://doi.org/10.1097/MAO.0b013e31822a1c7d.
Goodwin CR, Elder BD, Ward A, et al. Risk factors for failed transverse sinus stenting in Pseudotumor cerebri patients. Clin Neurol Neurosurg. 2014;127:75–8. https://doi.org/10.1016/j.clineuro.2014.09.015.
Thurtell MJ, Wall M. Idiopathic intracranial hypertension (pseudotumor cerebri): recognition, treatment, and ongoing management. Curr Treat Options Neurol. 2013;15(1):1–12. https://doi.org/10.1007/s11940-012-0207-4.
Acheson JF. Idiopathic intracranial hypertension and visual function. Br Med Bull. 2006;79-80:233–44. https://doi.org/10.1093/bmb/ldl019.
Radhakrishnan K, Thacker AK, Bohlaga NH, Maloo JC, Gerryo SE. Epidemiology of idiopathic intracranial hypertension: a prospective and case-control study. J Neurol Sci. 1993;116(1):18–28. https://doi.org/10.1016/0022-510x(93)90084-c.
Olesen J. The international classification of headache disorders. 2nd edition (ICHD-II). Rev Neurol (Paris). 2005;161(6-7):689–91. https://doi.org/10.1016/s0035-3787(05)85119-7.
Kosmorsky GS. Idiopathic intracranial hypertension: pseudotumor cerebri. Headache. 2014;54(2):389–93. https://doi.org/10.1111/head.12284.
Aaron G, Doyle J, Vaphiades MS, Riley KO, Woodworth BA. Increased intracranial pressure in spontaneous CSF leak patients is not associated with papilledema. Otolaryngol Head Neck Surg. 2014;151(6):1061–6. https://doi.org/10.1177/0194599814551122.
Bidot S, Clough L, Saindane AM, Newman NJ, Biousse V, Bruce BB. The optic canal size is associated with the severity of papilledema and poor visual function in idiopathic intracranial hypertension. J Neuroophthalmol. 2016;36(2):120–5. https://doi.org/10.1097/WNO.0000000000000318.
Johnson LN, Krohel GB, Madsen RW, March GA. The role of weight loss and acetazolamide in the treatment of idiopathic intracranial hypertension (Pseudotumor cerebri). Ophthalmology. 1998;105(12):2313–7. https://doi.org/10.1016/S0161-6420(98)91234-9.
Lee AG, Golnik K, Kardon R, Wall M, Eggenberger E, Yedavally S. Sleep apnea and intracranial hypertension in men. Ophthalmology. 2002;109(3):482–5. https://doi.org/10.1016/s0161-6420(01)00987-3.
Fridley J, Foroozan R, Sherman V, Brandt ML, Yoshor D. Bariatric surgery for the treatment of idiopathic intracranial hypertension. J Neurosurg. 2011;114(1):34–9. https://doi.org/10.3171/2009.12.JNS09953.
Satti SR, Leishangthem L, Chaudry MI. Meta-analysis of CSF diversion procedures and dural venous sinus stenting in the setting of medically refractory idiopathic intracranial hypertension. AJNR Am J Neuroradiol. 2015;36(10):1899–904. https://doi.org/10.3174/ajnr.A4377.
Sismanis A, Butts FM, Hughes GB. Objective tinnitus in benign intracranial hypertension: an update. Laryngoscope. 1990;100(1):33–6. https://doi.org/10.1288/00005537-199001000-00008.
Murphy TP. Otologic manifestations of pseudotumor cerebri. J Otolaryngol. 1991;20(4):258–61.
Shim T, Chillakuru Y, Moncada P, et al. Sensorineural hearing loss and tinnitus characteristics in patients with idiopathic intracranial hypertension. Otol Neurotol. 2021;42(9):1323–8. https://doi.org/10.1097/MAO.0000000000003213.
Vivas EX, Mccall A, Raz Y, Fernandez-Miranda JC, Gardner P, Hirsch BE. ICP, BMI, surgical repair, and CSF diversion in patients presenting with spontaneous CSF otorrhea. Otol Neurotol. 2014;35(2):344–7. https://doi.org/10.1097/MAO.0b013e3182a473cf.
Nelson RF, Gantz BJ, Hansen MR. The rising incidence of spontaneous cerebrospinal fluid leaks in the United States and the association with obesity and obstructive sleep apnea. Otol Neurotol. 2015;36(3):476–80. https://doi.org/10.1097/MAO.0000000000000535.
Stevens SM, Lambert PR, Rizk H, McIlwain WR, Nguyen SA, Meyer TA. Novel radiographic measurement algorithm demonstrating a link between obesity and lateral skull base attenuation. Otolaryngol Head Neck Surg. 2015;152(1):172–9. https://doi.org/10.1177/0194599814557470.
Prichard CN, Isaacson B, Oghalai JS, Coker NJ, Vrabec JT. Adult spontaneous CSF otorrhea: correlation with radiographic empty sella. Otolaryngol Head Neck Surg. 2006;134(5):767–71. https://doi.org/10.1016/j.otohns.2006.01.002.
Goddard JC, Meyer T, Nguyen S, Lambert PR. New considerations in the cause of spontaneous cerebrospinal fluid otorrhea. Otol Neurotol. 2010;31(6):940–5. https://doi.org/10.1097/mao.0b013e3181e8f36c.
Rosenfeld E, Dotan G, Kimchi TJ, Kesler A. Spontaneous cerebrospinal fluid otorrhea and rhinorrhea in idiopathic intracranial hypertension patients. J Neuroophthalmol. 2013;33(2):113–6. https://doi.org/10.1097/WNO.0b013e18274b870.
Kenning TJ, Willcox TO, Artz GJ, Schiffmacher P, Farrell CJ, Evans JJ. Surgical management of temporal meningoencephaloceles, cerebrospinal fluid leaks, and intracranial hypertension: treatment paradigm and outcomes. Neurosurg Focus. 2012;32(6):E6. https://doi.org/10.3171/2012.4.FOCUS1265.
Stucken EZ, Selesnick SH, Brown KD. The role of obesity in spontaneous temporal bone encephaloceles and CSF leak. Otol Neurotol. 2012;33(8):1412–7. https://doi.org/10.1097/MAO.0b013e318268d350.
Schlosser RJ, Bolger WE. Significance of empty sella in cerebrospinal fluid leaks. Otolaryngol Head Neck Surg. 2003;128(1):32–8. https://doi.org/10.1067/mhn.2003.43.
O’Connell BP, Stevens SM, Xiao CC, Meyer TA, Schlosser RJ. Lateral skull base attenuation in patients with anterior cranial fossa spontaneous cerebrospinal fluid leaks. Otolaryngol Head Neck Surg. 2016;154(6):1138–44. https://doi.org/10.1177/0194599816630738.
Psaltis AJ, Overton LJ, Thomas WW, Fox NF, Banks CA, Schlosser RJ. Differences in skull base thickness in patients with spontaneous cerebrospinal fluid leaks. Am J Rhinol Allergy. 2014;28(1):e73–9. https://doi.org/10.2500/ajra.2014.28.4002.
Stevens SM, Rizk HG, McIlwain WR, Lambert PR, Meyer TA. Association between lateral skull base thickness and surgical outcomes in spontaneous CSF Otorrhea. Otolaryngol Head Neck Surg. 2016;154(4):707–14. https://doi.org/10.1177/0194599816628528.
Liu Z, Dong C, Wang X, et al. Association between idiopathic intracranial hypertension and sigmoid sinus dehiscence/diverticulum with pulsatile tinnitus: a retrospective imaging study. Neuroradiology. 2015;57(7):747–53. https://doi.org/10.1007/s00234-015-1517-5.
Harvey RS, Hertzano R, Kelman SE, Eisenman DJ. Pulse-synchronous tinnitus and sigmoid sinus wall anomalies: descriptive epidemiology and the idiopathic intracranial hypertension patient population. Otol Neurotol. 2014;35(1):7–15. https://doi.org/10.1097/MAO.0b013e3182a4756c.
Schlosser RJ, Wilensky EM, Grady MS, Bolger WE. Elevated intracranial pressures in spontaneous cerebrospinal fluid leaks. Am J Rhinol. 2003;17(4):191–5.
Wang EW, Vandergrift WA, Schlosser RJ. Spontaneous CSF leaks. Otolaryngol Clin North Am. 2011;44(4):845–56, vii. https://doi.org/10.1016/j.otc.2011.06.018.
Rizk HG, Hatch JL, Stevens SM, Lambert PR, Meyer TA. Lateral skull base attenuation in superior semicircular canal dehiscence and spontaneous cerebrospinal fluid otorrhea. Otolaryngol Head Neck Surg. 2016;155(4):641–8. https://doi.org/10.1177/0194599816651261.
El Hadi T, Sorrentino T, Calmels MN, Fraysse B, Deguine O, Marx M. Spontaneous tegmen defect and semicircular canal dehiscence: same etiopathogenic entity? Otol Neurotol. 2012;33(4):591–5. https://doi.org/10.1097/MAO.0b013e31824bae10.
Georgalas C, Oostra A, Ahmed S, et al. International consensus statement: spontaneous cerebrospinal fluid rhinorrhea. Int Forum Allergy Rhinol. 2021;11(4):794–803. https://doi.org/10.1002/alr.22704.
Oh MS, Vivas EX, Hudgins PA, Mattox DE. The prevalence of superior semicircular canal dehiscence in patients with mastoid encephalocele or cerebrospinal fluid otorrhea. Otol Neurotol. 2019;40(4):485–90. https://doi.org/10.1097/MAO.0000000000002155.
Jan TA, Cheng YS, Landegger LD, et al. Relationship between surgically treated superior canal dehiscence syndrome and body mass index. Otolaryngol Head Neck Surg. 2017;156(4):722–7. https://doi.org/10.1177/0194599816686563.
Erdogan N, Songu M, Akay E, et al. Posterior semicircular canal dehiscence in asymptomatic ears. Acta Otolaryngol (Stockh). 2011;131(1):4–8. https://doi.org/10.3109/00016489.2010.502184.
Verrecchia L, Edholm K, Pekkari M. Asymptomatic superior semicircular canal dehiscence. J Laryngol Otol. 2022;136(1):87–90. https://doi.org/10.1017/S0022215121003273.
Minor LB, Cremer PD, Carey JP, Della Santina CC, Streubel SO, Weg N. Symptoms and signs in superior canal dehiscence syndrome. Ann N Y Acad Sci. 2001;942:259–73. https://doi.org/10.1111/j.1749-6632.2001.tb03751.x.
Zhang L, Creighton FX, Carey JP. A cohort study comparing importance of clinical factors in determining diagnosis and treatment for superior semicircular canal dehiscence syndrome. Otol Neurotol. 2021;42(9):1429–33. https://doi.org/10.1097/MAO.0000000000003274.
Zuniga MG, Janky KL, Nguyen KD, Welgampola MS, Carey JP. Ocular versus cervical VEMPs in the diagnosis of superior semicircular canal dehiscence syndrome. Otol Neurotol. 2013;34(1):121–6. https://doi.org/10.1097/MAO.0b013e31827136b0.
Janky KL, Nguyen KD, Welgampola M, Zuniga MG, Carey JP. Air-conducted oVEMPs provide the best separation between intact and superior canal dehiscent labyrinths. Otol Neurotol. 2013;34(1):127–34. https://doi.org/10.1097/MAO.0b013e318271c32a.
Gioacchini FM, Alicandri-Ciufelli M, Kaleci S, Scarpa A, Cassandro E, Re M. Outcomes and complications in superior semicircular canal dehiscence surgery: a systematic review. Laryngoscope. 2016;126(5):1218–24. https://doi.org/10.1002/lary.25662.
Lee JA, Liu YF, Nguyen SA, McRackan TR, Meyer TA, Rizk HG. Posterior semicircular canal dehiscence: case series and systematic review. Otol Neurotol. 2020;41(4):511–21. https://doi.org/10.1097/MAO.0000000000002576.
Succar EF, Manickam PV, Wing S, Walter J, Greene JS, Azeredo WJ. Round window plugging in the treatment of superior semicircular canal dehiscence. Laryngoscope. 2018;128(6):1445–52. https://doi.org/10.1002/lary.26899.
Friedman DI, Jacobson DM. Diagnostic criteria for idiopathic intracranial hypertension. Neurology. 2002;59(10):1492–5. https://doi.org/10.1212/01.wnl.0000029570.69134.1b.
Friedman DI, Liu GT, Digre KB. Revised diagnostic criteria for the pseudotumor cerebri syndrome in adults and children. Neurology. 2013;81(13):1159–65. https://doi.org/10.1212/WNL.0b013e3182a55f17.
De Simone R, Ranieri A, Montella S, et al. Intracranial pressure in unresponsive chronic migraine. J Neurol. 2014;261(7):1365–73. https://doi.org/10.1007/s00415-014-7355-2.
Wang F, Lesser ER, Cutsforth-Gregory JK, et al. Population-based evaluation of lumbar puncture opening pressures. Front Neurol. 2019;10:899. https://doi.org/10.3389/fneur.2019.00899.
Celebisoy N, Gökçay F, Sirin H, Akyürekli O. Treatment of idiopathic intracranial hypertension: topiramate vs acetazolamide, an open-label study. Acta Neurol Scand. 2007;116(5):322–7. https://doi.org/10.1111/j.1600-0404.2007.00905.x.
Sugita Y, Iijima S, Teshima Y, et al. Marked episodic elevation of cerebrospinal fluid pressure during nocturnal sleep in patients with sleep apnea hypersomnia syndrome. Electroencephalogr Clin Neurophysiol. 1985;60(3):214–9. https://doi.org/10.1016/0013-4694(85)90033-1.
Jennum P, Børgesen SE. Intracranial pressure and obstructive sleep apnea. Chest. 1989;95(2):279–83. https://doi.org/10.1378/chest.95.2.279.
Purvin VA, Kawasaki A, Yee RD. Papilledema and obstructive sleep apnea syndrome. Arch Ophthalmol. 2000;118(12):1626–30. https://doi.org/10.1001/archopht.118.12.1626.
Poletti-Muringaseril SC, Rufibach K, Ruef C, Holzmann D, Soyka MB. Low meningitis-incidence in primary spontaneous compared to secondary cerebrospinal fluid rhinorrhoea. Rhinology. 2012;50(1):73–9. https://doi.org/10.4193/Rhino11.124.
Eljamel MS, Foy PM. Acute traumatic CSF fistulae: the risk of intracranial infection. Br J Neurosurg. 1990;4(5):381–5. https://doi.org/10.3109/02688699008992759.
McGirt MJ, Woodworth G, Thomas G, Miller N, Williams M, Rigamonti D. Cerebrospinal fluid shunt placement for pseudotumor cerebri-associated intractable headache: predictors of treatment response and an analysis of long-term outcomes. J Neurosurg. 2004;101(4):627–32. https://doi.org/10.3171/jns.2004.101.4.0627.
Abubaker K, Ali Z, Raza K, Bolger C, Rawluk D, O’Brien D. Idiopathic intracranial hypertension: lumboperitoneal shunts versus ventriculoperitoneal shunts—case series and literature review. Br J Neurosurg. 2011;25(1):94–9. https://doi.org/10.3109/02688697.2010.544781.
Kanagalingam S, Subramanian PS. Cerebral venous sinus stenting for pseudotumor cerebri: a review. Saudi J Ophthalmol. 2015;29(1):3–8. https://doi.org/10.1016/j.sjopt.2014.09.007.
Carter SR, Seiff SR. Macular changes in pseudotumor cerebri before and after optic nerve sheath fenestration. Ophthalmology. 1995;102(6):937–41. https://doi.org/10.1016/s0161-6420(95)30931-1.
Chandrasekaran S, McCluskey P, Minassian D, Assaad N. Visual outcomes for optic nerve sheath fenestration in pseudotumour cerebri and related conditions. Clin Experiment Ophthalmol. 2006;34(7):661–5. https://doi.org/10.1111/j.1442-9071.2006.01301.x.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Doerfer, K.W., Schutt, C.A., Dwyer, S., Kado, K. (2022). Increased Intracranial Pressure. In: Gianoli, G.J., Thomson, P. (eds) Third Mobile Window Syndrome of the Inner Ear. Springer, Cham. https://doi.org/10.1007/978-3-031-16586-3_19
Download citation
DOI: https://doi.org/10.1007/978-3-031-16586-3_19
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-16585-6
Online ISBN: 978-3-031-16586-3
eBook Packages: MedicineMedicine (R0)