Abstract
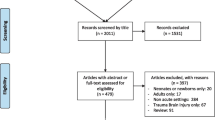
Transcranial Doppler (TCD) ultrasonography has an established clinical role in reducing a first ever stroke in children with sickle cell disease (SCD) by identifying those at high risk who benefit from blood transfusion. In this chapter, we will review the literature related to this topic. Beyond SCD, other potential roles for TCD in pediatrics include as a point of care ultrasound (POCUS) or as a neuromonitoring strategy in the pediatric intensive care unit (PICU). We will therefore also review the literature for the applications of TCD in critically ill children with traumatic brain injury (TBI), cerebral vasospasm, brain death, and those undergoing support with extracorporeal membrane oxygenation (ECMO). Based on the limited available evidence for these topics, TCD data in these populations should be treated as hypothesis-generating. TCD may serve as a precursor or adjunct to definitive imaging or invasive techniques. In order to put TCD into routine practice in the pediatric intensive care unit (PICU), collaboration and research is needed to determine the appropriate clinical indications and quantify the impact of use on clinical care and outcomes.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Adams R, McKie V, Nichols F, Carl E, Zhang DL, McKie K, et al. The use of transcranial ultrasonography to predict stroke in sickle cell disease. N Engl J Med. 1992;326(9):605–10.
Adams RJ, McKie VC, Hsu L, Files B, Vichinsky E, Pegelow C, et al. Prevention of a first stroke by transfusions in children with sickle cell anemia and abnormal results on transcranial doppler ultrasonography. N Engl J Med. 1998;339(1):5–11.
Adams RJ, McKie VC, Brambilla D, Carl E, Gallagher D, Nichols FT, et al. Stroke prevention trial in sickle cell anemia. Control Clin Trials. 1998;19(1):110–29.
Adams RJ, Brambilla DJ, Granger S, Gallagher D, Vichinsky E, Abboud MR, et al. Stroke and conversion to high risk in children screened with transcranial doppler ultrasound during the STOP study. Blood. 2004;103(10):3689–94.
Adams RJ, Brambilla D. Optimizing primary stroke prevention in sickle cell anemia trial I: discontinuing prophylactic transfusions used to prevent stroke in sickle cell disease. N Engl J Med. 2005;353(26):2769–78.
LaRovere KL, Tasker RC, Wainwright M, Reuter-Rice K, Appavu B, Miles D, et al. Transcranial doppler ultrasound during critical illness in children: survey of practices in pediatric neurocritical care centers. PCCM. 2020;21(1):67–74.
Tegeler CH, Crutchfield K, Katsnelson M, Kim J, Tang R, Passmore Griffin L, et al. Transcranial doppler velocities in a large, healthy population. J Neuroimaging. 2013;23(3):466–72.
O’Brien NF. Reference values for cerebral blood flow velocities in critically ill sedated children. Childs Nerv Syst. 2015;31(12):2269–76.
Bode H, Wais U. Age dependence of flow velocities in basal cerebral arteries. Arch Dis Child. 1988;63(6):606–11.
Quinn CT, Rogers ZR, Buchanan GR. Survival of children with sickle cell disease. Blood. 2004;103(11):4023–7.
Rothman SM, Fulling KH, Nelson JS. Sickle cell anemia and central nervous system infarction: a neuropathological study. Ann Neurol. 1986;20(6):684–90.
Kaul DK, Fabry ME, Nagel RL. Microvascular sites and characteristics of sickle cell adhesion to vascular endothelium in shear flow conditions: pathophysiological implications. Proc Natl Acad Sci U S A. 1989;86(9):3356–60.
Merkel KH, Ginsberg PL, Parker JC Jr, Post MJ. Cerebrovascular disease in sickle cell anemia: a clinical, pathological and radiological correlation. Stroke. 1978;9(1):45–52.
Thust SC, Burke C, Siddiqui A. Neuroimaging findings in sickle cell disease. Br J Radiol. 2014;87(1040):20130699.
Stockman JA, Nigro MA, Mishkin MM, Oski FA. Occlusion of large cerebral vessels in sickle-cell anemia. NEJM. 1972;287(17):846–9.
Powars D, Wilson B, Imbus C, Pegelow C, Allen J. The natural history of stroke in sickle cell disease. Am J Med. 1978;65(3):461–71.
Russell MO, Goldberg HI, Hodson A, Kim HC, Halus J, Reivich M, et al. Effect of transfusion therapy on arteriographic abnormalities and on recurrence of stroke in sickle cell disease. Blood. 1984;63(1):162–9.
Brass LM, Pavlakis SG, DeVivo D, Piomelli S, Mohr JP. Transcranial doppler measurements of the middle cerebral artery. Effect of hematocrit. Stroke. 1988;19(12):1466–9.
Adams RJ, Nichols FT, Figueroa R, McKie V, Lott T. Transcranial doppler correlation with cerebral angiography in sickle cell disease. Stroke. 1992;23(8):1073–7.
Adams RJ, McKie VC, Carl EM, Nichols FT, Perry R, Brock K, et al. Long-term stroke risk in children with sickle cell disease screened with transcranial doppler. Ann Neurol. 1997;42(5):699–704.
Nichols FT, Jones AM, Adams RJ. Stroke prevention in sickle cell disease (STOP) study guidelines for transcranial doppler testing. J Neuroimaging. 2001;11(4):354–62.
Lee YS, Jung KH, Roh JK. Diagnosis of moyamoya disease with transcranial doppler sonography: correlation study with magnetic resonance angiography. J Neuroimaging. 2004;14(4):319–23.
Fullerton HJ, Elkind MS, Barkovich AJ, Glaser C, Glidden D, Hills NK, et al. The vascular effects of infection in pediatric stroke (VIPS) study. J Child Neurol. 2011;26(9):1101–10.
Wintermark M, Hills NK, deVeber GA, Barkovich AJ, Elkind MS, Sear K, et al. Arteriopathy diagnosis in childhood arterial ischemic stroke: results of the vascular effects of infection in pediatric stroke study. Stroke. 2014;45(12):3597–605.
Elkind MS, Hills NK, Glaser CA, Lo WD, Amlie-Lefond C, Dlamini N, et al. Herpesvirus infections and childhood arterial ischemic stroke: results of the VIPS study. Circulation. 2016;133(8):732–41.
van Santbrink H, Schouten JW, Steyerberg EW, Avezaat CJ, Maas AI. Serial transcranial doppler measurements in traumatic brain injury with special focus on the early posttraumatic period. Acta Neurochir. 2002;144(11):1141–9.
Ract C, Le Moigno S, Bruder N, Vigue B. Transcranial doppler ultrasound goal-directed therapy for the early management of severe traumatic brain injury. Int Care Med. 2007;33(4):645–51.
Trabold F, Meyer PG, Blanot S, Carli PA, Orliaguet GA. The prognostic value of transcranial doppler studies in children with moderate and severe head injury. Int Care Med. 2004;30(1):108–12.
Chaiwat O, Sharma D, Udomphorn Y, Armstead WM, Vavilala MS. Cerebral hemodynamic predictors of poor 6-month Glasgow outcome score in severe pediatric traumatic brain injury. J Neurotrauma. 2009;26(5):657–63.
Visocchi M, Chiaretti A, Genovese O, Di Rocco F. Haemodynamic patterns in children with posttraumatic diffuse brain swelling. A preliminary study in 6 cases with neuroradiological features consistent with diffuse axonal injury. Acta Neurochir. 2007;149(4):347–56.
O’Brien NF, Maa T, Moore-Clingenpeel M, Rosenberg N, Yeates KO. Relationships between cerebral flow velocities and neurodevelopmental outcomes in children with moderate to severe traumatic brain injury. Childs Nerv Syst. 2018;34(4):663–72.
Kochanek PM, Tasker RC, Carney N, Totten AM, Adelson PD, Selden NR, et al. Guidelines for the management of pediatric severe traumatic brain injury, third edition: update of the brain trauma foundation guidelines. PCCM. 2019;20(3S Suppl 1):S1–S82.
Kochanek PM, Tasker RC, Carney N, Totten AM, Adelson PD, Selden NR, et al. Guidelines for the management of pediatric severe traumatic brain injury, third edition: update of the brain trauma foundation guidelines, executive summary. Neurosurgery. 2019;84(6):1169–78.
Alkhoury F, Kyriakides TC. Intracranial pressure monitoring in children with severe traumatic brain injury: National Trauma Data Bank-Based Review of outcomes. JAMA Surg. 2014, Jun;149(6):544–8.
Alali AS, Gomez D, Sathya C, Burd RS, Mainprize TG, Moulton R, et al. Intracranial pressure monitoring among children with severe traumatic brain injury. J Neurosurg Pediatr. 2015;16(5):523–32.
Morris KP, Forsyth RJ, Parslow RC, Tasker RC, Hawley CA, Group UKPTBIS, Paediatric Intensive Care Society Study G. Intracranial pressure complicating severe traumatic brain injury in children: monitoring and management. Int Care Med. 2006;32(10):1606–12.
Bennett TD, Riva-Cambrin J, Keenan HT, Korgenski EK, Bratton SL. Variation in intracranial pressure monitoring and outcomes in pediatric traumatic brain injury. Arch Pediatr Adolesc Med. 2012;166(7):641–7.
Dixon RR, Nocera M, Zolotor AJ, Keenan HT. Intracranial pressure monitoring in infants and young children with traumatic brain injury. PCCM. 2016;17(11):1064–72.
Van Cleve W, Kernic MA, Ellenbogen RG, Wang J, Zatzick DF, Bell MJ, et al. National variability in intracranial pressure monitoring and craniotomy for children with moderate to severe traumatic brain injury. Neurosurgery. 2013;73(5):746–52.
Figaji AA, Zwane E, Fieggen AG, Siesjo P, Peter JC. Transcranial doppler pulsatility index is not a reliable indicator of intracranial pressure in children with severe traumatic brain injury. Surg Neurol. 2009;72(4):389–94.
Melo JR, Di Rocco F, Blanot S, Cuttaree H, Sainte-Rose C, Oliveira-Filho J, et al. Transcranial doppler can predict intracranial hypertension in children with severe traumatic brain injuries. Childs Nerv Syst. 2011;27(6):979–84.
O’Brien NF, Maa T, Reuter-Rice K. Noninvasive screening for intracranial hypertension in children with acute, severe traumatic brain injury. J Neurosurg Pediatr. 2015;16(4):420–5.
Fanelli A, Vonberg FW, LaRovere KL, Walsh BK, Smith ER, Robinson S, et al. Fully automated, real-time, calibration-free, continuous noninvasive estimation of intracranial pressure in children. J Neurosurg Pediatr. 2019;24(5):509–19.
O’Brien NF, Lovett ME, Chung M, Maa T. Non-invasive estimation of cerebral perfusion pressure using transcranial doppler ultrasonography in children with severe traumatic brain injury. Childs Nerv Syst. 2020;36(9):2063–71.
Rao VK, Haridas A, Nguyen TT, Lulla R, Wainwright MS, Goldstein JL. Symptomatic cerebral vasospasm following resection of a medulloblastoma in a child. Neurocrit Care. 2013;18(1):84–8.
Pendharkar AV, Guzman R, Dodd R, Cornfield D, Edwards MS. Successful treatment of severe cerebral vasospasm following hemorrhage of an arteriovenous malformation. Case report. J Neurosurg Pediatr. 2009;4(3):266–9.
O’Brien NF, Reuter-Rice KE, Khanna S, Peterson BM, Quinto KB. Vasospasm in children with traumatic brain injury. Int Care Med. 2010;36(4):680–7.
O’Brien NF, Maa T, Yeates KO. The epidemiology of vasospasm in children with moderate-to-severe traumatic brain injury. CCM. 2014;43(3):674–85.
Philip S, Chaiwat O, Udomphorn Y, Moore A, Zimmerman JJ, Armstead W, et al. Variation in cerebral blood flow velocity with cerebral perfusion pressure >40 mm Hg in 42 children with severe traumatic brain injury. CCM. 2009;37(11):2973–8.
O’Brien NF, Mutatshi Taty T, Moore-Clingenpeel M, Bodi Mabiala J, Mbaka Pongo J, Ambitapio Musungufu D, et al. Transcranial doppler ultrasonography provides insights into neurovascular changes in children with cerebral malaria. Pediatrics. 2018;203(116–24):e113.
Garg K, Singh PK, Sharma BS, Chandra PS, Suri A, Singh M, et al. Pediatric intracranial aneurysms--our experience and review of literature. Childs Nerv Syst. 2014;30(5):873–83.
Moftakhar P, Cooke DL, Fullerton HJ, Ko NU, Amans MR, Narvid JA, et al. Extent of collateralization predicting symptomatic cerebral vasospasm among pediatric patients: correlations among angiography, transcranial doppler ultrasonography, and clinical findings. J Neurosurg Pediatr. 2015;15(3):282–90.
Udomphorn Y, Armstead WM, Vavilala MS. Cerebral blood flow and autoregulation after pediatric traumatic brain injury. Pediatr Neurol. 2008;38(4):225–34.
O’Brien NF, Buttram SDW, Maa T, Lovett ME, Reuter-Rice K, LaRovere KL. Cerebrovascular physiology during pediatric extracorporeal membrane oxygenation: a multicenter study using transcranial doppler ultrasonography. PCCM. 2019;20(2):178–86.
Rilinger JF, Smith CM, deRegnier RAO, Goldstein JL, Mills MG, Reynolds M, et al. Transcranial doppler identification of neurologic injury during pediatric extracorporeal membrane oxygenation therapy. J Stroke Cerebrovasc Dis. 2017;26(10):2336–45.
Thiagarajan RR, Barbaro RP, Rycus PT, McMullan DM, Conrad SA, Fortenberry JD, et al. Extracorporeal life support organization registry international report 2016. ASAIO. 2017;63(1):60–7.
Bembea MM, Felling RJ, Caprarola SD, Ng DK, Tekes A, Boyle K, et al. Neurologic outcomes in a two-center cohort of neonatal and pediatric patients supported on extracorporeal membrane oxygenation. ASAIO. 2020;66(1):79–88.
Barrett CS, Bratton SL, Salvin JW, Laussen PC, Rycus PT, Thiagarajan RR. Neurological injury after extracorporeal membrane oxygenation use to aid pediatric cardiopulmonary resuscitation. PCCM. 2009;10(4):445–51.
Waitzer E, Riley SP, Perreault T, Shevell MI. Neurologic outcome at school entry for newborns treated with extracorporeal membrane oxygenation for noncardiac indications. J Child Neurol. 2009;24(7):801–6.
Schiller RM, Madderom MJ, Reuser JJ, Steiner K, Gischler SJ, Tibboel D, et al. Neuropsychological follow-up after neonatal ECMO. Pediatrics. 2016;138(5):e20161313.
Bembea MM, Felling R, Anton B, Salorio CF, Johnston MV. Neuromonitoring during extracorporeal membrane oxygenation: a systematic review of the literature. PCCM. 2015;16(6):558–64.
Kwon HM, Park JH, Kim JM, Yoon BW. Mild left ventricular dysfunction is associated with thrombogenicity in cardioembolic stroke. Eur Neurol. 2006;56(4):217–21.
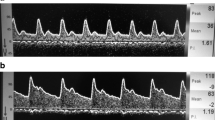
Yang Y, Grosset DG, Li Q, Lees KR. Identification of echocardiographic “smoke” in a bench model with transcranial doppler ultrasound. Stroke. 2000;31(4):907–14.
Asinger RW, Koehler J, Pearce LA, Zabalgoitia M, Blackshear JL, Fenster PE, et al. Pathophysiologic correlates of thromboembolism in nonvalvular atrial fibrillation: II. Dense spontaneous echocardiographic contrast (The Stroke Prevention in Atrial Fibrillation [SPAF-III] study). J A Soc Echocardiogr. 1999;12(12):1088–96.
Ringelstein EB, Droste DW, Babikian VL, Evans DH, Grosset DG, Kaps M, et al. Consensus on microembolus detection by TCD. International consensus group on microembolus detection. Stroke. 1998;29(3):725–9.
Imaduddin SM, LaRovere KL, Kussman BD, Heldt T. A time-frequency approach for cerebral embolic load monitoring. IEEE Trans Biomed Eng. 2019;67(4):1007–18.
LaRovere KL, Kapur K, McElhinney DB, Razumovsky A, Kussman BD. Cerebral high-intensity transient signals during pediatric cardiac catheterization: a pilot study using transcranial doppler ultrasonography. J Neuroimaging. 2017;27(4):381–7.
Sanker P, Roth B, Frowein RA, Firsching R. Cerebral reperfusion in brain death of a newborn. Case report. Neurosurg Rev. 1992;15(4):315–7.
Glasier CM, Seibert JJ, Chadduck WM, Williamson SL, Leithiser RE Jr. Brain death in infants: evaluation with doppler US. Radiology. 1989;172(2):377–80.
Bode H, Sauer M, Pringsheim W. Diagnosis of brain death by transcranial doppler sonography. Arch Dis Child. 1988;63(12):1474–8.
World malaria report 2018. Geneva: World Health Organization; 2018.
Okiro EA, Al-Taiar A, Reyburn H, Idro R, Berkley JA, Snow RW. Age patterns of severe paediatric malaria and their relationship to plasmodium falciparum transmission intensity. Malar J. 2009;8(4):1–11.
Taylor TE. Caring for children with cerebral malaria: insights gleaned from 20 years on a research ward in Malawi. Trans R Soc Trop Med Hyg. 2009;103(Suppl 1):S6–10.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this chapter
Cite this chapter
LaRovere, K.L., O’Brien, N.F. (2022). Applications of Transcranial Doppler Ultrasonography in Sickle Cell Disease, Stroke, and Critical Illness in Children. In: Ziai, W.C., Cornwell, C.L. (eds) Neurovascular Sonography . Springer, Cham. https://doi.org/10.1007/978-3-030-96893-9_19
Download citation
DOI: https://doi.org/10.1007/978-3-030-96893-9_19
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-96892-2
Online ISBN: 978-3-030-96893-9
eBook Packages: MedicineMedicine (R0)