Abstract
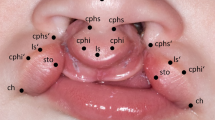
Cleft palate surgery is technically challenging to perform. There is delicate tissue handling required within the confines of the infant oral cavity workspace. A surgical robot provides improved visualization, access, and precision. Therefore, cleft palate surgery is a suitable environment for robotic application. A highly realistic cleft palate simulator was developed for testing existing and newly developed robotic systems to determine feasibility and efficacy of robotic cleft palate surgery. The cleft palate simulator has been validated as a realistic simulation environment as well as an effective and valuable training tool. Pre-clinical and clinical studies have determined that robotic cleft palate surgery is feasible and offers specific advantages such as improved visualization, access, precision, and ergonomics. However, existing robotic systems require design optimization for the unique requirements of performing cleft palate surgery within the confines of the infant oral cavity workspace. A newly developed robotic instrument that couples to the da Vinci surgical system has been developed that is more readily miniaturized and provides more compact articulation within the infant oral cavity workspace compared to existing robotic instruments. As smaller and more capable robotic surgical systems become available in the future, robotic cleft palate surgery may evolve to provide a more precise repair that ultimately may lead to improved patient outcomes.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
Abbreviations
- DOF:
-
Degrees-of-freedom
- PSM:
-
Patient side manipulator
- RCM:
-
Remote center of motion
- TORS:
-
Trans-oral robotic surgery
References
Mossey PA, Little J, Munger RG, Dixon MJ, Shaw WC. Cleft lip and palate. Lancet. 2009;374(9703):1773–85.
Burg ML, Chai Y, Yao CA, Magee W, Figueiredo JC. Epidemiology, etiology, and treatment of isolated cleft palate. Front Physiol. 2016;6(67):1–16.
Woo AS. Evidence-based medicine: cleft palate. Plast Reconstr Surg. 2017;139(1):191e–203e.
Hopper RA, Tse R, Smartt J, Swanson J, Kinter S. Cleft palate repair and velopharyngeal dysfunction. Plast Reconstr Surg. 2014;133(6):852e–64e.
Vadodaria S, Watkin N, Thiessen F, Ponniah A. The first cleft palate simulator. Plast Reconstr Surg. 2007;120(1):259–61.
Sommerlad BC. A technique for cleft palate repair. Plastic Reconstr Surg. 2003;112(6):1542–8.
Cutting CB, Rosenbaum J, Rovati L. The technique of muscle repair in the cleft soft palate. Oper Tech Plast Reconstr Surg. 1995;2(4):215–22.
Sommerlad BC. Surgery of the cleft palate: repair using the operating microscope with radical muscle retropositioning–the GostA approach. B-ENT. 2006;2(Suppl 4):32–4.
Sommerlad BC. The use of the operating microscope for cleft palate repair and pharyngoplasty. Plast Reconstr Surg. 2003;112(6):1540–1.
Witt PD, Wahlen JC, Marsh JL, Grames LM, Pilgram TK. The effect of surgeon experience on velopharyngeal functional outcome following palatoplasty: is there a learning curve? Plast Reconstr Surg. 1998;102(5):1375–84.
Rintala AE, Haapanen ML. The correlation between training and skill of the surgeon and reoperation rate for persistent cleft palate speech. Br J Oral Maxillofac Surg. 1995;33:295–8.
Khan K, Dobbs T, Swan MC, Weinstein GS, Goodacre TE. Trans-oral robotic cleft surgery (TORCS) for palate and posterior pharyngeal wall reconstruction: a feasibility study. J Plast Reconstr Aesthet Surg. 2016;69(1):97–100.
Selber JC, Sarhane KA, Ibrahim AE, Holsinger FC. Transoral robotic reconstructive surgery. Semin Plast Surg. 2014;28(1):35–8.
Selber JC, Alrasheed T. Robotic microsurgical training and evaluation. Semin Plast Surg. 2014;28(1):5–10.
Willis RE, Gomez PP, Ivatury SJ, Mitra HS, Van Sickle KR. Virtual reality simulators: valuable surgical skills trainers or video games? J Surg Educ. 2014;71(3):426–33.
Kazan R, Cyr S, Hemmerling TM, Lin SJ, Gilardino MS. The evolution of surgical simulation: The current state and future avenues for plastic surgery education. Plast Reconstr Surg. 2017;139(2):533e–43e.
da Cruz JA, Dos Reis ST, Cunha Frati RM, Duarte RJ, Nguyen H, Srougi M, et al. Does warm-up training in a virtual reality simulator improve surgical performance? A prospective randomized analysis. J Surg Educ. 2016;73(6):974–8.
Cosman P, Hemli JM, Ellis AM, Hugh TJ. Learning the surgical craft: a review of skills training options. ANZ J Surg. 2007;77(10):838–45.
Senturk S. The simplest cleft palate simulator. J Craniofac Surg. 2013;24(3):1056.
Nagy K, Mommaerts MY. Advanced s(t)imulator for cleft palate repair techniques. Cleft Palate Craniofac J. 2009;46(1):1–5.
Matthews MS. A teaching device for Furlow palatoplasty. Cleft Palate Craniofac J. 1999;36(1):64–6.
Devinck F, Riot S, Qassemyar A, Belkhou A, Wolber A, Martinot Duquennoy V, et al. Suture simulator - Cleft palate surgery. Ann Chir Plast Esthet. 2017;62(2):167–70.
Podolsky DJ, Fisher DM, Wong Riff KW, Looi T, Drake JM, Forrest CR. Infant robotic cleft palate surgery: a feasibility assessment using a realistic cleft palate simulator. Plast Reconstr Surg. 2017;139(2):455e–65e.
Podolsky DJ, Fisher DM, Wong Riff KW, Szasz P, Looi T, Drake JM, Forrest CR. Assessing technical performance and determining the learning curve in cleft palate surgery using a high fidelity cleft palate simulator. Plast Reconstr Surg. 2018;141(6):1485–500.
Podolsky DJ, Fisher DM, Wong KW, Looi T, Drake JM, Forrest CR. Evaluation and implementation of a high-fidelity cleft palate simulator. Plast Reconstr Surg. 2017;139(1):85e–96e.
Cheng H, Podolsky DP, Fisher DM, Wong Riff KW, Lorenz PH, Khosla RK, Drake JM, Forrest CR. Teaching palatoplasty using a high-fidelity cleft palate simulator. Plast Reconstr Surg. 2018;141(1):91e–8e.
Xiao D, Jakimowicz JJ, Albayrak A, Buzink SN, Botden SM, Goossens RH. Face, content, and construct validity of a novel portable ergonomic simulator for basic laparoscopic skills. J Surg Educ. 2014;71(1):65–72.
Ghaderi I, Manji F, Park YS, Juul D, Ott M, Harris I, et al. Technical skills assessment toolbox: a review using the unitary framework of validity. Ann Surg. 2015;261(2):251–62.
Arezzo A, Ulmer F, Weiss O, Schurr MO, Hamad M, Buess GF. Experimental trial on solo surgery for minimally invasive therapy: comparison of different systems in a phantom model. Surg Endosc. 2000;14(10):955–9.
Niccolini M, Castelli V, Diversi C, Kang B, Mussa F, Sinibaldi E. Development and preliminary assessment of a robotic platform for neuroendoscopy based on a lightweight robot. Int J Med Robot. 2016;12(1):4–17.
Strauss G, Koulechov K, Hofer M, Dittrich E, Grunert R, Moeckel H, et al. The navigation-controlled drill in temporal bone surgery: a feasibility study. Laryngoscope. 2007;117(3):434–41.
Ghezzi TL, Corleta OC. 30 years of robotic surgery. World J Surg. 2016;40(10):2550–7.
Selber JC. Transoral robotic reconstruction of oropharyngeal defects: a case series. Plast Reconstr Surg. 2010;126(6):1978–87.
Pugin F, Bucher P, Morel P. History of robotic surgery: from AESOP(R) and ZEUS(R) to da Vinci(R). J Visc Surg. 2011;148(5 Suppl):e3–8.
Hussain A, Malik A, Halim MU, Ali AM. The use of robotics in surgery: a review. Int J Clin Pract. 2014;68(11):1376–82.
Marcus HJ, Hughes-Hallett A, Cundy TP, Yang G, Darzi A, Nandi D. da Vinci robot-assisted keyhole neurosurgery: a cadaver study on feasibility and safety. Neurosurg Rev. 2015;38:367–71.
Li Z, Glozman D, Milutinovic D, Rosen J. Maximizing dexterous workspace and optimal port placement of a multi-arm surgical robot. IEEE International Conference on Robotics and Automation; 2011; Shanghai, China. p. 3394–9.
Sun LW, Yeung CK. Port placement and pose selection of the da Vinci surgical system for collision-free intervention based on performance optimization. Proceedings of the 2007 IEEE/RSJ International Conference on Intelligent Robots and Systems; 2007; San Diego, CA, USA. p. 1951–6.
Li G, Wu D, Ma R, Huang K, Du Z. Pose planning for robotically assisted minimally invasive surgery. 3rd International Conference on Biomedical Engineering and Informatics; 2010; Yantai, China. p. 1769–74.
Nadjmi N. Transoral robotic cleft palate surgery. Cleft Palate Craniofac J. 2016;53(3):326–31.
Carroll DJ, Byrd JK, Harris GF. The feasibility of pediatric TORS for lingual thyroglossal duct cyst. Int J Pediatr Otorhinolaryngol. 2016;88:109–12.
Wine TM, Duvvuri U, Maurer SH, Mehta DK. Pediatric transoral robotic surgery for oropharyngeal malignancy: a case report. Int J Pediatr Otorhinolaryngol. 2013;77(7):1222–6.
Mahida JB, Cooper JN, Herz D, Diefenbach KA, Deans KJ, Minneci PC, et al. Utilization and costs associated with robotic surgery in children. J Surg Res. 2015;199(1):169–76.
Cheon B, Gezgin E, Ji DK, Tomikawa M, Hashizume M, Kim HJ, et al. A single port laparoscopic surgery robot with high force transmission and a large workspace. Surg Endosc. 2014;28(9):2719–29.
Choi H, Kwak HS, Lim YA, Kim HJ. Surgical robot for single-incision laparoscopic surgery. IEEE Trans Biomed Eng. 2014;61(9):2458–66.
Xu K, Goldman RE, Ding J, Allen PK, Fowler DL, Simaan N. System design of an insertable robotic effector platform for single port access (SPA) surgery. IEEE/RSJ International Conference on Intelligent Robots and Systems; 2009; St. Louis, USA. p. 5546–52.
Lee H, Choi Y, Yi B. Stackable 4-BAR manipulator for single port access surgery. IEEE/ASME Trans Mechatron. 2012;17(1):157–65.
Quaglia C, Petroni G, Niccolini M, Caccavaro S, Dario P, Menciassi A. Design of a compact robotic manipulator for single-port laparoscopy. ASME J Mech Des. 2014;136(10): 105001.
Piccigallo M, Scarfogliero U, Quaglia C, Petroni G, Valdastri P, Menciassi A, Dario P. Design of a novel bimanual robotic system for single-port laparoscopy. IEEE/ASME Trans Mechatron. 2010;15(6):871–8.
Abbott DJ, Becke C, Rothstein R, Peine W. Design of an Endoluminal NOTES Robotic System. IEEE/RSJ International Conference on Intelligent Robots and Systems; 2007; San Diego, CA, USA. p. 410–16.
Rivera-Serrano CM, Johnson P, Zubiate B, Kuenzler R, Choset H, Zenati M, et al. A transoral highly flexible robot: novel technology and application. Laryngoscope. 2012;122(5):1067–71.
Jelinek F, Arkenbout EA, Henselmans PW, Pessers R, Breedveld P. Classification of joints used in steerable instruments for minimally invasive surgery-a review of the state of the art. J Med Devices. 2015;9(1)
Catherine J, Christine RL, Micaelli A. Comparative review of endoscopic devices articulations technologies developed for minimally invasive medical procedures. Appl Bionics Biomech. 2011;8:151–71.
Podolsky DJ, Diller E, Fisher DM, Wong Riff KW, Looi T, Drake J, Forrest C. Utilization of cable guide channels for compact articulation within a dexterous three degrees-of-freedom surgical wrist design. J Med Devices. 2019;13(1)
Wu G, Podolsky D, Looi T, Kahrs L, Drake J, Forrest C. A 3 mm wristed instrument for the da Vinci robot: setup, characterization, and phantom tests for cleft palate repair. IEEE Trans Med Robot Bionics. 2020;2(2):130–9.
Pessaux P, Diana M, Soler L, Piardi T, Mutter D, Marescaux J. Towards cybernetic surgery: robotic and augmented reality-assisted liver segmentectomy. Langenbeck’s Arch Surg. 2015;400(3):381–5.
Hellan M, Spinoglio G, Pigazzi A, Lagares-Garcia JA. The influence of fluorescence imaging on the location of bowel transection during robotic left-sided colorectal surgery. Surg Endosc. 2014;28(5):1695–702.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Podolsky, D.J., Fisher, D.M., Wong Riff, K.W., Looi, T., Drake, J.M., Forrest, C.R. (2021). Robotic Cleft Palate Surgery and Simulation. In: Selber, J.C. (eds) Robotics in Plastic and Reconstructive Surgery. Springer, Cham. https://doi.org/10.1007/978-3-030-74244-7_7
Download citation
DOI: https://doi.org/10.1007/978-3-030-74244-7_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-74243-0
Online ISBN: 978-3-030-74244-7
eBook Packages: MedicineMedicine (R0)