Abstract
Achieving and maintaining skeletal health throughout the life trajectory is essential for the prevention of bone diseases such as rickets, osteomalacia and osteoporosis. Rickets and osteomalacia are usually a result of calcium and/or vitamin D deficiency, causing softening of bones and bone pain, and both conditions are treatable with calcium and vitamin D supplementation. Osteoporosis is a multifaceted disease mainly affecting older people, and its pathogenesis (and hence treatment) is more complex. Untreated osteoporosis results in fragility fractures causing morbidity and increased mortality.
Nutrition is one of many factors that influence bone mass and risk of bone disease. Developing a nutritional sciences approach is a feasible option for improving bone health.
The importance of adequate calcium and vitamin D in ensuring skeletal integrity throughout the life course has a sound evidence base. Poor vitamin D status in population groups of all ages is widespread across many countries (including affluent and non-affluent areas). Public health approaches are required to correct this given the fact that vitamin D is not just required for musculoskeletal health but also for other health outcomes.
Dietary protein may be beneficial for bone due to its effect of increasing insulin-like growth-factor-1 (IGF-1). Recent meta-analyses show that dietary protein has a beneficial role to play in bone health at all ages.
Other nutritional factors and nutrients (such as potassium, magnesium, vitamin K and acid-base balance) are also likely to have an important role in bone health, though the literature is less clear in terms of the association/relationship and more research is required.
This chapter is a component of Part I: Nutritional Care in Old Age.
For an explanation of the grouping of chapters in this book, please see Chap. 1: ‘Overview of Nutrition Care in Geriatrics and Orthogeriatrics’.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
FormalPara Learning OutcomesBy the end of this chapter, you will be able to:
-
Explain the role of key nutrients and other factors that influence bone mass and risk of bone disease.
-
Apply knowledge learned and tools to identify older adults with or at risk of musculoskeletal frailty and fractures.
-
Apply multicomponent strategies to prevent and manage frailty, fragility, fractures and osteoporosis.
1 Introduction
1.1 Bone
Bone is a complex living tissue. It provides structure, support and protection for the body. It is formed from collagen reinforced by minerals. There are two types of bone in the skeleton: cortical and trabecular. Cortical bone is smooth, dense and strong and is found at the surface of bone. Trabecular bone has a honeycomb structure and is found inside the bones, making bone strong, light and slightly flexible. Bone is built and develops its strength through the early years.
1.2 Normal Bone Metabolism
Bone metabolism is a continual cycle of bone formation and bone resorption undertaken by cells called osteoclasts and osteoblasts [1]. The bone matrix created requires mineralisation with calcium phosphate. Bone metabolism is influenced by hormones and other regulatory factors.
Think of the bones like an enormous house, constantly in need of maintenance and updating. Bone cells are like groups of workmen, ones that pull down the old walls (cells called osteoclasts) and ones that build up new walls (cells called osteoblasts). This process continues constantly, and slowly, over time, and the house (or the skeleton) is renewed. Ageing causes the groups of workmen building up new walls (the osteoblasts) to get slower and slower and fall behind their destructive colleagues. This leads to crumbling walls in the house making it more likely to fall down or the bone to fracture.
1.3 Peak Bone Mass (PBM)
The skeleton usually reaches maximum growth between the late second and early third decades and mineralises during this time as well. During this time, bone is being laid down faster than it is being absorbed, gradually increasing in density. Peak bone mass is achieved in the early fourth decade when bone is at its most robust. Genetic factors play a key role in the population variation of PBM, with estimates around 70–75% [2]. However, this still leaves plenty of room for key modifiable exogenous factors such as the effects of diet (including calcium, vitamin D, protein and other essential minerals) hormones and physical activity. After the fourth decade, bone mass declines, more gradually in men than women as a result of the menopause [3, 4].
2 Nutrients and Bone Health
2.1 Calcium
Calcium is an important component of the skeleton and is one of the predominant minerals found in bone. Over 99% of the body’s total calcium is found in bones and teeth in the form of hydroxyapatite. The remaining 1% of calcium circulates in the blood. Phosphorus and magnesium also make up a large percentage of the bone matrix, with over 88% and 60% of the body’s content of these minerals deposited in bone. There is no functional marker for calcium nutritional status, since serum/plasma calcium levels are homeostatically controlled by the body [5].
Inadequate calcium intake is a worldwide problem, having been reported in children, adolescents and adults across Europe, North America, Asia and Oceania [6]. In older adults, calcium intake varies between countries [6]. In the UK, preschool children [7] and adolescents aged 11–18 years [8] have been reported to have dietary calcium intakes below the relative UK Department of Health reference nutrient intake (RNI), whereas younger and older adults are meeting the UK RNI [8, 9].
The evidence that calcium supplementation improves attainment of bone density in childhood and prevents fractures in older age is weak and inconsistent [10, 11]. Thus, calcium supplementation is not recommended for fracture prevention at a population level.
There is however good data to show that calcium supplements are effective in reducing bone loss in late menopausal women (>5 years postmenopause), particularly in those with low habitual calcium intake (<400 mg/day) [12]. In the key study by [13], late postmenopausal women were found to have a significant reduction in lumbar spine and femoral neck bone loss following supplementation with 500 mg calcium per day, but no such effect was seen in early postmenopausal women (<5 years postmenopause). Reviews of over 20 studies have shown that calcium supplementation can decrease bone loss by approximately 1% per year. There are some data to suggest that the effect of calcium supplementation may be greater at skeletal sites with more cortical bone. There are also data to suggest that calcium supplementation improves the efficacy of antiresorptive therapy on bone mass [14].
2.2 Vitamin D
Vitamin D is the generic term for two molecules: ergocalciferol and cholecalciferol. Ergocalciferol (vitamin D2) is derived by ultraviolet (UV) irradiation of ergosterol, which is found in fungi and plants [15]. Cholecalciferol (vitamin D3) is formed from the effect of UV irradiation on the skin. The action of sunlight on the skin converts 7-dehydrocholesterol to previtamin D, which is metabolised to vitamin D by a temperature-dependent isomerisation. Vitamin D is then transported via the general circulation to the liver, where the enzyme 25-hydroxylase converts it to 25-hydroxy-vitamin D (25-OHD). This is the key circulating vitamin D metabolite and the best indicator of clinical status [15]. The kidney is the site for further conversion to calcitriol or 1,25(OH)2D3.
Calcitriol (1,25(OH)2D3), the active form of vitamin D, helps to maintain normal blood levels of calcium and phosphate. It promotes calcium absorption and bone mineralisation. It also enhances osteoclastic activity (bone turnover). Together with parathyroid hormone (PTH), it regulates calcium and phosphorus metabolism by promoting calcium absorption from the gut and kidney tubules [15].
25-Hydroxy-vitamin D (25-OHD) is the major circulating vitamin D metabolite and can be measured in the blood, considered the gold standard method for establishing vitamin D status [16]. However, there is a lack of consensus and definition regarding the suggested thresholds of 25-OHD used to define vitamin D deficiency or optimal levels, and the range of terminology and associated values used make comparisons of reported prevalence difficult.
The World Health Organization and the UK’s Scientific Advisory Committee on Nutrition (SACN) state that 25-OHD levels <25 nmol/L (10 mg/mL) is the deficiency threshold [16,17,19] with regard to the prevention of rickets and osteomalacia, and the WHO also defines vitamin D insufficiency as 25-OHD levels <50 nmol/L. However, the US Institute of Medicine (IOM) defines 25-OHD levels <30 nmol/L as deficiency, 30–50 nmol/L as inadequacy and >50 nmol/L as sufficient [20].
The UK National Osteoporosis Society has agreed with the IOM thresholds and proposed that the UK practitioners should also adopt these [21]. Commonly, vitamin D deficiency is defined by a 25-OHD threshold of <25–30 nmol/L, with insufficiency defined by 25-OHD levels in the range of 25–49 nmol/L [22]. Conversely, the Endocrine Society Task Force (USA/Canada) define deficiency as 25-OHD levels <50 nmol/L and advocate that 25-OHD levels should exceed 75 nmol/L [23].
Vitamin D deficiency has been associated with skeletal conditions and other musculoskeletal health outcomes. Low 25-OHD levels of <12 nmol/L in children often result in rickets [19]. In adults, 25-OHD levels ≤20 nmol/L result in osteomalacia [19].
In addition, epidemiological studies and randomised controlled trials have reported associations between vitamin D levels and muscle strength and function [24, 25], fracture risk [26, 27] and risk of falls [28]. Specifically, supplementation with vitamin D has been shown to have a positive effect on bone mineral density [26, 27, 29] with a recent meta-analysis of 23 studies showing a small benefit on femoral neck bone mineral density [30].
Our main source of vitamin D is the ultraviolet (UV) in sunlight. Much of the UV in sunlight is absorbed by clouds, ozone and other forms of atmospheric pollution. UV sunlight varies daily, seasonally and depending on latitude. In the UK, there is no UV radiation of the appropriate wavelength (280–310 mm) from the end of October to the end of March. For the remaining months of the year, the main percentage of the effective UV radiation occurs between 11.00 am and 3.00 pm [31].
A number of factors reduce the vitamin D production from UV exposure. Sunscreens absorb UVB radiation when applied to the skin, thereby reducing the production of previtamin D3. Glass absorbs all UVB photons, and hence sunlight that has passed through glass will not promote vitamin D3 synthesis in the skin. Clothing also absorbs UVB radiation; this is particularly relevant for women who cover up for cultural reasons.
There are few dietary sources of vitamin D. The major providers are fat spreads (which are often fortified with vitamin D), fish, eggs, pastry products, fortified breakfast cereals and meat [18].
2.3 Vitamin K
Vitamin K (‘koagulation vitamin’) was first described in Denmark by Dam (1935) as a dietary-derived coagulation factor [32]. He noted that a bleeding disorder in chickens was corrected by feeding a variety of vitamin K-rich foods. The fat-soluble vitamin was finally isolated in 1939. Vitamin K refers to a family of compounds with a common chemical structure, 2-methyl-1,4-naphthoquinone. Phylloquinone (vitamin K1) is present in plant-based foods, particularly green leafy vegetables. Menaquinones (vitamin K2) are derived from bacterial fermentation of foods such as cheese [33].
Vitamin K has an important function for the skeleton. There are data to show that low serum concentrations of vitamin K are associated with low bone mineral density and increased risk for osteoporotic fracture [34].
The results of randomised controlled trials looking at the effects of vitamin K supplementation and markers of bone health have been very disappointing, and the most recent vitamin K/fracture prevention meta-analysis did not demonstrate a beneficial effect of this nutrient on markers of bone health or prevention of osteoporotic fracture [35].
2.4 Protein
Historically there has been much debate as to whether dietary protein is good or bad for bone health. Insulin-like growth factor-1 (IGF-1) is a hormone which builds up the bone. IGF-1 is stimulated by dietary protein intake. In terms of epidemiology, many studies have found a positive association between dietary protein intake and bone health [36, 37], but some have found no association [38]. In particular there is conflicting evidence as to whether protein intake is associated with hip fracture risk, with a recent systematic reviews and meta-analyses finding a positive association between dietary protein intake and bone mass density, but not fracture risk [39, 40]. Therefore, dietary protein may have beneficial effects on bone density, but this may not necessarily translate into reduced risk of fracture.
2.5 Other Nutrients
There are numerous studies looking at other nutrients including potassium, vitamin C, vitamin E and vitamin A. It is difficult to draw clear conclusions from the evidence available, and none of these supplements are routinely recommended in promoting bone health [41].
3 Other Factors Influencing Bone Health
Hormones are extremely important in bone health. Normal testosterone and normal menstruation are required in order for bone to reach peak bone mass. Cigarette smoking and excessive alcohol intake may further accelerate the loss of bone in both women and men [1].
The skeleton also needs to be used appropriately. Bone density is achieved by putting weight through it. Over 100 years ago, a German scientist called Julius Wolff suggested the theory that bone would adapt to the load under which it is placed and would remodel to become stronger to resist that sort of loading, now known as Wolff’s law [42]. More recently, this concept has been refined to a general theory of bone mass regulation, known as the mechanostat model [43]. In the absence of weight-bearing exercise, bone loss will occur at both axial and appendicular skeletal sites. Early astronauts discovered that when they landed back on Earth, they had lost significant bone density and strength; it is the action of gravity through bones that gives them strength.
4 Osteoporosis
Osteoporosis is a term derived from osteo (bone) and porous (full of holes). This means that the bone is fragile and at increased risk of fracture. There are a pathological definition based on the appearance of bone under the microscope and a clinical definition where fracture type, mechanism of fracture and results of a bone density scan are used to define osteoporosis.
Osteoporosis is often diagnosed following a low trauma fracture typically affecting the wrist, a vertebral body in the spine or a hip (more specifically the neck of femur).
The most common and widely available bone density scan is the DEXA or dual-energy X-ray absorptiometry scan [44]. The result is described by a T-score and a Z-score. The T-score compares the result with that of a healthy 40-year-old. The Z-score compares the result to an age-matched average. The T-score is more widely used to diagnose osteoporosis. This score has been validated for use in different populations across the world. The measurements are ranked on a scale of normal distribution. Standard deviations of +1 or −1 are considered normal. This encompasses about 80% of the population. Scores from −1 to −2.5 are considered osteopenia (‘thin’ bone). A T-score of less than −2.5 is considered as osteoporotic. There are other ways to measure bone density including quantitative CT [45], but this is much less widely used.
Bone density is a strong predictor of fracture, yet many fragility fractures occur without osteoporosis as assessed by density criteria; this highlights the need to consider additional factors other than bone mineral density that may contribute to an older adult’s risk of fracture [46].
4.1 Risk Factors for Osteoporosis
There are a range of conditions and factors that accelerate bone density decline. These are termed risk factors and may be used in diagnosing and directing management of osteoporosis.
Osteoporosis increases with age and is more common in women, largely because of menopause and the loss of the hormonal access. Premature menopause and treatments that bring on menopause or reduce testosterone increase risk. Amenorrhoea associated with multiple pregnancies or often seen in eating disorders is strongly associated with reduced bone density [46, 47].
Osteoporosis is more common in Caucasian or Asian individuals and in those with a family history of maternal or paternal hip fracture. Body mass index is important with osteoporosis being more common in those who are underweight due to less basal bone mass and those with obesity. Both smoking and alcohol increase risk in a dose-dependent fashion [48].
Secondary osteoporosis occurs in those with other conditions associated with osteoporosis, e.g. rheumatoid arthritis, type 1 diabetes, untreated long-standing hyperthyroidism, hypogonadism or premature menopause (less than 45 years), chronic malnutrition (including eating disorders such as anorexia nervosa) or malabsorption, chronic liver disease and osteogenesis imperfecta in adults (Table 9.1) [50].
Medications associated with osteoporosis include steroids, low molecular weight heparin, proton pump inhibitors (e.g. omeprazole, lansoprazole), SSRIs (selective serotonin reuptake inhibitors; antidepressants), aromatase inhibitors for breast cancer and anti-epileptics. This list is by no means exhaustive. These are often dose-dependent, with longer exposure being more highly correlated with risk. In the context of steroids, a significant proportion of bone loss is thought to occur in the first 3 months of treatment. A clinically relevant dose is more than 3 months of at least 5 mg of prednisolone daily (Table 9.1) (Chap. 19) [51].
5 Fragility, Fractures and Falls
Fragility is defined as ‘the quality of being easily broken or damaged’ [52]. A fracture is a crack or break in a bone. Fragility fractures occur as a result of a fall from a standing height in someone with delicate or vulnerable bones. Fragility fractures are common and occur in one in three women and one in five men aged over 50 years. It is estimated that across the world a fragility fracture occurs every 3 s.
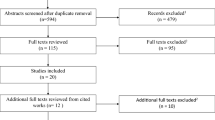
Falls are more common with age and one third of people over 65 years of age will fall each year. Falls are more likely to result in fractures, particularly in those with osteoporosis. A previous fracture is a strong predictor of future fractures [53]. This is often progressive with time; Fig. 9.1 highlights the progressive impact of osteoporosis, as commonly seen in ageing individuals.
The burden of osteoporosis [54]. (With permission of Kanis JA, Johnell O. The burden of osteoporosis. J Endocrinol Invest. 1999;22(8):583–8)
Wrist fractures often occur in early stages of osteoporosis in mobile individuals who fall forwards onto an outstretched hand. They usually result in a temporary disability but heal well with most individuals regaining most of their previous level of function. Vertebral fragility fractures may occur insidiously without significant trauma and be attributed to an exacerbation of chronic back pain. Progressive vertebral fractures can occur over many years resulting in loss of height with significant curvature of the spine (kyphosis) leading to progressive problems with balance, mobility and breathing. Hip fractures are considered the most significant fragility fracture associated with increased morbidity and mortality. They usually occur in older adults with intracapsular fractures resulting from a sideways fall onto the hip. There has been a focus on hip fracture management in the UK over the last 12 years with year-on-year reduction in mortality with the latest figure of 6.1% at 30 days [55]. However the 1-year mortality remains around 22% [56].
A significant proportion of older adults presenting with hip fracture have frailty. One study identified that 17% had no frailty, 39% had mild frailty [4, 5] and 44% had moderate to severe frailty [57]. Frailty is a widely used term in healthcare and is associated with functional decline and mortality. It is often associated with multimorbidity and ageing but is not synonymous with either. The word frailty often conjures up an image of an older person such as that described above, with poor muscle mass, a curved spine and arthritic joints struggling with mobility and function [58, 59].
Key causes of frailty, prevalence, associated outcomes and preventative and interventional management strategies have been previously detailed (Chap. 8). We highlight here the concept of musculoskeletal frailty, which often includes a loss of muscle (sarcopenia), loss of collagen (osteoarthritis) and loss of bone (osteoporosis) [60]. All elements of musculoskeletal frailty can be significantly reduced by a life-course approach to healthy ageing [61] (Chaps. 4 and 14). This is important as musculoskeletal frailty is a key predictor of fall-related fractures.
5.1 Frailty, Falls and Bone Health Assessment
5.1.1 Frailty Assessment
The description of frailty using a phenotypical approach was first described by Fried [58] and colleagues requiring the presence of three or more out of five indicators: weakness (reduced grip strength), slowness (gait speed), weight loss, low physical activity and exhaustion. Whilst global consensus is lacking, a useful broad definition encompasses a loss of physiological reserve so that systems fail with minor stressors. Frailty can be classified in many ways; a practical and widely used tool for frailty identification is the Rockwood Clinical Frailty Scale. This scale can be applied for those with frailty as a result of physical or cognitive decline (Fig. 9.2) [62].
The Rockwood Clinical Frailty Scale.
Source: (Canadian Study on Health & Aging, Revised 2008. 2. K. Rockwood et al. A global clinical measure of fitness and frailty in elderly people. CMAJ 2005;173:489–495. © 2007–2009. Version 1.2. All rights reserved. Geriatric Medicine Research, Dalhousie University, Halifax, Canada. Permission granted to copy for research and educational purposes only. Participating Sites: Cape Breton District HEALTH AUTHORITY Making Healthier Choices Together Sponsors: © 2007–2009. Version 1.2. All rights reserved. Geriatric Medicine Research, Dalhousie University, Halifax, Canada. Permission granted to copy for research and educational purposes only)
5.1.2 Falls Risk Assessment
In addition to advancing musculoskeletal frailty, other key factors influencing the incidence of falls include effects of polypharmacy, metabolic imbalances, cardiac events, related to alcohol intake, lack of a safe living environment, visual disturbances, reduced cognition (with poor safety awareness) and also reduced continence resulting in hurrying to the toilet or trying to manage incontinence [63]. A recent study has identified that malnourished inpatients were almost 8 times more likely to have a harmful fall than those not malnourished, independent of age and BMI [64].
Consequently, clinical care guidelines, for example, the UK’s NICE Guideline [65], recommend that older people are asked about their history of falls whenever coming into contact with health or social care practitioners. Where falls (or risk of falls) have been identified, older adults should be offered a multifactorial risk assessment and interventions to prevent further falls.
5.1.3 Bone Health Assessment
Given the complexities within and across sarcopenia, osteoarthritis, osteoporosis and frailty and the diversity of factors that contribute to fracture risk, bone health assessment requires an individualised, comprehensive approach. In a number of settings, bone health assessment applies a personalised fracture risk assessment tool such as FRAX® (https://www.sheffield.ac.uk/FRAX/). The FRAX® tool uses clinical risk factors to establish an individual’s fracture risk based on studying population-based cohorts from Europe, North America, Asia and Australia.
The FRAX® algorithms are freely available on the website and give the 10-year probability of fracture. The National Osteoporosis Guideline Group graphs provide a visual guide for clinicians and patients in recommending treatment, further assessment with DXA scan or lifestyle advice.
An initial fragility fracture is a strong predictor of second fracture; the importance of secondary fracture prevention cannot be overemphasised. As an example, Hip Fracture Care Clinical Care Standards require that hip fracture patients are assessed for future fall and fracture risk by suitably qualified orthogeriatric healthcare professionals, with documented plans for management including assessment for risk of falls, fall history and risk factors for falls, including a medication review, and formulation of a plan to prevent further falls. Despite such recommendations, falls risk assessment and secondary prevention strategies such as prescription of bone protection medication are often not undertaken following identification of initial fragility fracture. Audit data continues to highlight substantial variation and an ongoing, significant care gap that appears resistant to improvement and, consequently, missed opportunities to prevent consequent fractures [66].
6 Supporting Those with Frailty, Fragility, Fractures and Osteoporosis
Despite clearly articulated risk factors at the population level, for many individuals a fall and subsequent fracture is usually a significant and unexpected event. It can lead to a loss of confidence, isolation, reduced physical function, disability and in some cases a reliance on informal/formal care or even a change in living circumstances. Falls and fractures often also lead to a new diagnosis of osteoporosis, a disease which the older adult may have hitherto been unaware of. Individuals need access to the right treatment, support, education and encouragement to enable them to make the best possible recovery and to prevent further fractures occurring.
6.1 Lifestyle Advice to Improve Bone Health
Lifestyle advice includes nutritional guidance including sources of calcium, vitamin D and other essential nutrients and minerals as described above. Ceasing smoking, avoiding alcohol excess and encouraging a balanced diet rich in fruit and vegetables and ensuring at least sufficient or increased protein intakes (as recommended in older adults) may also contribute to the prevention of osteoporosis, improved bone health and/or reduced complications [1, 53, 67, 68].
For older adults with conditions that affect nutrition, a dietitian review is advised. Suggesting exercise as a prescription rather than a casual activity can influence uptake (Chap. 14). It is important to support the older adult through the initial trauma recovery to the post-injury rehabilitation and ultimately to a regular exercise schedule to maintain their mobility and balance.
Physical activity and exercise plays [1] a key role in improving bone health as well as improving balance. The work carried out by the Royal Osteoporosis Society (ROS) in the recent ‘strong, steady and straight campaign’ is a helpful consensus document providing the evidence to encourage older adults to exercise and provides the healthcare provider some clarity around the use of exercise in those with osteoporosis [69]. Strategies to reduce the risk of falls are also recommended as a key lifestyle management approach [49].
Older adults with osteoporosis often experience loss of confidence following a low-impact fall resulting in fracture. Thus their fear of falling results in restriction of movement and lifestyle. This in turn results in deconditioning and an increase in their risk of further falls and fracture. This consensus document indicates that increased activity and weight-bearing exercise is likely to provide greater lifestyle benefits and reduce fracture risk.
6.2 Supplementation and Medications
For most patients, calcium and vitamin D supplements are recommended. Medication for established osteoporosis has a good evidence base, for example, antiresorptive therapy (e.g. bisphosphonates, denosumab). Hormonal treatments may also be appropriate for some individuals [1]. Consideration must be given to potential side effects and adverse outcomes, duration of treatments and monitoring processes for prescribed supplements and/or medications [12].
Long-term medication adherence however remains a challenge [70] with less than 30% of patients continuing to take medication at 2 years. The asymptomatic nature of osteoporosis requires careful attention to emphasise the risk of complications from untreated disease. There are many factors which affect patients’ persistence [71].
These can be positively influenced by establishing a good relationship with the older adult, a medication regime to suit the individual and a clear understanding of the benefits. Negative influencers include the effect of negative press reports on long-term use of antiresorptive agents. As an example, the SCOOP trial in 2012 [72] identified that patients who underwent a DEXA scan and had the result explained to them were more likely to be adherent and persistent with medication.
Whether in relation to supplements or medications likely to adversely influence bone health and fracture risk, older adults should be supported to make an informed decision regarding medication by providing clear information about benefits and possible side effects. It is essential for older adults also to understand how to take medications to ensure they are effective and to minimise potential harm [49].
6.3 Education, Training and Sociopolitical Action
Valuable research by Yardley et al. [73] into designing and delivering advice about falls prevention indicated that if falls prevention education is given in a patronising way, where the individual is somehow seen to be negligent or they have done something ‘stupid’, they are less likely to engage in a falls prevention programme.
Listening to the older adult’s experience of falling and placing falls education within an exercise/balance initiative can make the older person more likely to actively engage in both falls prevention and exercise [63, 73].
Training to support the management of osteoporosis should be integrated into training processes across medical, nursing and allied health disciplines [49]. Programme and political level action is the recognised fourth pillar for orthogeriatric care; advocating for change in healthcare policy and priorities by engaging and mobilising healthcare leaders, policymakers and other sociopolitical influencers is a key factor to realising better bone health for individuals and populations [49, 72, 74].
Across acute, rehabilitation and secondary prevention settings, the importance of education and training for older adults, their carers, healthcare providers and services, organisations and professional bodies should be considered a fundamental priority. This is perhaps best highlighted by the Fragility Fracture Network call to action [75] which highlights the need for engaged, educated healthcare stakeholders to support coordinated care for those with or at risk of fragility fracture across acute, rehabilitation and secondary prevention settings. Perhaps most importantly, this needs to be underpinned sociopolitical action to overcome the failure for uptake of key opportunities for care improvement.
6.3.1 Coordinated Care Opportunities to Optimise Bone Health, Fragility and Fractures in Older Adults
6.3.1.1 Example 1: Orthogeriatric Services
Orthogeriatric services have been developed as a result of a focus on hip fracture care. Best practice for hip fractures involves early surgery and standardised peri-operative management with coordination between orthopaedic, anaesthetic and geriatric services [76].
A coordinated approach throughout the older adult’s journey is imperative to ensure that individuals are optimised before surgery to reduce post-operative complications and have access to appropriate interdisciplinary rehabilitation. Falls and bone health assessment are key to future fracture prevention.
6.3.1.2 Care Example 2: Fracture Liaison Services
The ‘Capture the Fracture’ campaign led by the International Osteoporosis Foundation is a global resource supporting the implementation of a post-fracture coordination programme such as a fracture liaison service. This coordinated, multidisciplinary approach has a strong evidence base in preventing further fractures also resulting in significant cost saving for healthcare systems and has also been demonstrated to reduce mortality [55, 77]. Globally there are almost 600 fracture liaison services registered with the ‘Capture the Fracture’ campaign over 48 countries (https://www.capturethefracture.org/).
6.3.1.3 Example 3: Fracture Liaison Nurses
Advancing older adult understanding through education is the key to self-management of bone health. The approach must be adjusted to the individual, their abilities and experience. For older adults living with frailty, engagement with their family and carers is often required. In many settings, fracture liaison nurse (FLN) roles have been established to advance knowledge of falls and bone health in addition to skills in health promotion. The overarching roles of the FLN (or similar positions) often include supporting an individual in coming to terms with their injury, working through the stages of the illness experience, encouraging older adults to actively participate in rehabilitation and educating older adults to manage their own bone health [78].
6.3.1.4 Example 4: Audit and Feedback
The role of audit and feedback to improve outcomes is well established. Implementation of the National Hip Fracture Database in the UK has been associated with improvements in care and survival of older people with hip fracture [79]. As a further example, the Fracture Liaison Service Database (FLS-DB) is a UK continuous audit, initiated to measure performance against standards of management of secondary prevention of fragility fractures set primarily by the National Institute for Clinical Excellence (NICE) and the Royal Osteoporosis Society. In 2017 there were 65 fracture liaison services operational in the UK who contributed data to the FLS-DB (https://www.fffap.org.uk/). Whilst the 2020 report demonstrates improvement in most key performance indicators, the audit highlights further opportunities to advance effective and efficient services.
6.3.2 End-of-Life Care
Lifestyle interventions, supplements and education to improve/maintain bone health are imperative to reducing population incidence of frailty, falls and fragility fractures. However, for those with severe frailty (CFS > 7) or end-stage disease, priorities are likely to be different and may require a refocus towards managing symptoms and comfort rather than disease prevention or cure (Chap. 21).
7 Summary
For all those working with older adults, it is important to have some insight into the complex interrelationship between bone health, fragility and fractures. Nutrition plays a key role in the promotion of bone health in the older population. The role of calcium and vitamin D is well established and dietary supplementation may be required. Less is known about the effects of dietary protein, acid-base balance and micronutrients.
Prevention of musculoskeletal frailty through a life-course approach focusing on a healthy diet, regular exercise and multi-component management of osteoporosis is recommended. Older adult and healthcare provider education is key to adherence to treatment strategies following fragility fractures; orthogeriatric services, fracture liaison services, fracture liaison nurses and feedback and audit processes should be considered a healthcare system priority.
Regardless of the age or stage of disease, individualised attention towards benefits versus burdens of potential interventions should be considered and where appropriate discussed with the older adult to guide patient-centred care. Actions to prevent initial disease onset and preventable complications must become the priority. Conversely, focus for management at the end of life is likely to be comfort, as at this stage it is unlikely that nutritional supplements, exercise or medication for bone health will be beneficial.
Take-Home Points
-
Nutrition plays a key role in the promotion of bone health in the older population.
-
There is a complex interrelationship between bone health, fragility and fractures.
-
Orthogeriatric services, fracture liaison services, fracture liaison nurses and feedback and audit processes should be routinely embedded in practice.
-
Engaging older adults, their carers, healthcare providers, organisations and professional bodies to prioritise a multi-component, life-course approach to preventing and managing bone health, fragility and fractures.
References
Barnsley J, Buckland G, Chan PE, Ong A, Ramos AS, Baxter M et al (2021) Pathophysiology and treatment of osteoporosis: challenges for clinical practice in older people. Aging Clin Exp Res 33:759
Maes HH, Neale MC, Eaves LJ (1997) Genetic and environmental factors in relative body weight and human adiposity. Behav Genet 27(4):325–351
Gordon CM, Zemel BS, Wren TA, Leonard MB, Bachrach LK, Rauch F et al (2017) The determinants of peak bone mass. J Pediatr 180:261–269
Lu J, Shin Y, Yen MS, Sun SS (2016) Peak bone mass and patterns of change in total bone mineral density and bone mineral contents from childhood into young adulthood. J Clin Densitom 19(2):180–191
Health NIo (2011) Dietary reference intakes for calcium and vitamin D. The national guidelines. Institute of Medicine (US), Washington, DC
Peterlik M, Cross HS (2009) Vitamin D and calcium insufficiency-related chronic diseases: molecular and cellular pathophysiology. Eur J Clin Nutr 63(12):1377–1386
Cribb VL, Northstone K, Hopkins D, Emmett PM (2015) Sources of vitamin D and calcium in the diets of preschool children in the UK and the theoretical effect of food fortification. J Hum Nutr Diet 28(6):583–592
Beverley Bates DC, Cox L, Nicholson S, Page P, Roberts C, Steer T, Swan G (2019) National diet and nutrition survey - years 1 to 9 of the rolling programme (2008/2009 – 2016/2017): time trend and income analyses. A survey carried out on behalf of Public Health England and the Food Standards Agency. Report No.: 2018756. Public Health England & Food Standards Agency, London
Derbyshire E (2018) Micronutrient intakes of British adults across mid-life: a secondary analysis of the UK National Diet and Nutrition Survey. Front Nutr 5:55
Winzenberg T, Shaw K, Fryer J, Jones G (2006) Effects of calcium supplementation on bone density in healthy children: meta-analysis of randomised controlled trials. BMJ 333(7572):775
Bolland MJ, Leung W, Tai V, Bastin S, Gamble GD, Grey A et al (2015) Calcium intake and risk of fracture: systematic review. BMJ 351:h4580
Sunyecz JA (2008) The use of calcium and vitamin D in the management of osteoporosis. Ther Clin Risk Manag 4(4):827–836
Dawson-Hughes B, Dallal GE, Krall EA, Sadowski L, Sahyoun N, Tannenbaum S (1990) A controlled trial of the effect of calcium supplementation on bone density in postmenopausal women. N Engl J Med 27;323(13):878–883
Lanham-New SA (2008) Importance of calcium, vitamin D and vitamin K for osteoporosis prevention and treatment: symposium on ‘Diet and bone health’. Proc Nutr Soc 67(2):163–176
Jäpelt RB, Jakobsen J (2013) Vitamin D in plants: a review of occurrence, analysis, and biosynthesis. Front Plant Sci 4:136
Seamans KM, Cashman KD (2009) Existing and potentially novel functional markers of vitamin D status: a systematic review. Am J Clin Nutr 89(6):1997S–2008S
WHO (2003) Global strategy on diet, physical activity and health - diet, nutrition and the prevention of chronic diseases. Contract No.: 916 (TRS 916). Surveillance and Population-based Prevention Unit, Department of Chronic Diseases and Health Promotion, Geneva
Kimball SM, Holick MF (2020) Official recommendations for vitamin D through the life stages in developed countries. Eur J Clin Nutr 74(11):1514–1518
D SACoNSWGoV (2016) Vitamin D and health report. SACN advises on nutrition and related health matters. It advises Public Health England (PHE) and other UK government organisations
Ross AC, Manson JE, Abrams SA, Aloia JF, Brannon PM, Clinton SK et al (2011) The 2011 report on dietary reference intakes for calcium and vitamin D from the Institute of Medicine: what clinicians need to know. J Clin Endocrinol Metab 96(1):53–58
Aspray TJ, Bowring C, Fraser W, Gittoes N, Javaid MK, Macdonald H et al (2014) National osteoporosis society vitamin D guideline summary. Age Ageing 43(5):592–595
Spiro A, Buttriss JL (2014) Vitamin D: an overview of vitamin D status and intake in Europe. Nutr Bull 39(4):322–350
Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP et al (2011) Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 96(7):1911–1930
Ward KA, Das G, Roberts SA, Berry JL, Adams JE, Rawer R et al (2010) A randomized, controlled trial of vitamin D supplementation upon musculoskeletal health in postmenarchal females. J Clin Endocrinol Metab 95(10):4643–4651
Tomlinson PB, Joseph C, Angioi M (2015) Effects of vitamin D supplementation on upper and lower body muscle strength levels in healthy individuals. A systematic review with meta-analysis. J Sci Med Sport 18(5):575–580
Chapuy MC, Arlot ME, Duboeuf F, Brun J, Crouzet B, Arnaud S et al (1992) Vitamin D3 and calcium to prevent hip fractures in elderly women. N Engl J Med 327(23):1637–1642
Dawson-Hughes B, Tosteson AN, Melton LJ III, Baim S, Favus MJ, Khosla S et al (2008) Implications of absolute fracture risk assessment for osteoporosis practice guidelines in the USA. Osteoporos Int 19(4):449–458
Stein MS, Wark JD, Scherer SC, Walton SL, Chick P, Di Carlantonio M et al (1999) Falls relate to vitamin D and parathyroid hormone in an Australian nursing home and hostel. J Am Geriatr Soc 47(10):1195–1201
Ooms ME, Lips P, Roos JC, van der Vijgh WJ, Popp-Snijders C, Bezemer PD et al (1995) Vitamin D status and sex hormone binding globulin: determinants of bone turnover and bone mineral density in elderly women. J Bone Miner Res 10(8):1177–1184
Reid IR, Bolland M, Grey A (2014) Effects of vitamin D supplements on bone mineral density: a systematic review and meta-analysis. Quality-assessed reviews. The University of York, 1995 - CfRaDU
Wacker M, Holick MF (2013) Sunlight and vitamin D: a global perspective for health. Dermatoendocrinology 5(1):51–108
Shampo MA, Kyle RA (1998) Henrik Dam-discoverer of vitamin K. Mayo Clin Proc 73:46
Gröber U, Reichrath J, Holick MF, Kisters K (2014) Vitamin K: an old vitamin in a new perspective. Dermatoendocrinology 6(1):e968490
Rodríguez-Olleros Rodríguez C, Díaz CM (2019) Vitamin K and bone health: a review on the effects of vitamin K deficiency and supplementation and the effect of non-vitamin K antagonist oral anticoagulants on different bone parameters. J Osteoporos 2019:2069176
Lewis R, Gómez Álvarez CB, Rayman M, Lanham-New S, Woolf A, Mobasheri A (2019) Strategies for optimising musculoskeletal health in the 21(st) century. BMC Musculoskelet Disord 20(1):164
Cooper C, Atkinson EJ, Hensrud DD, Wahner HW, O’Fallon WM, Riggs BL et al (1996) Dietary protein intake and bone mass in women. Calcif Tissue Int 58(5):320–325
Sahni S, Broe KE, Tucker KL, McLean RR, Kiel DP, Cupples LA et al (2014) Association of total protein intake with bone mineral density and bone loss in men and women from the Framingham Offspring Study. Public Health Nutr 17(11):2570–2576
Zhu K, Meng X, Kerr DA, Devine A, Solah V, Binns CW et al (2011) The effects of a two-year randomized, controlled trial of whey protein supplementation on bone structure, IGF-1, and urinary calcium excretion in older postmenopausal women. J Bone Miner Res 26(9):2298–2306
Darling AL, Manders RJF, Sahni S, Zhu K, Hewitt CE, Prince RL et al (2019) Dietary protein and bone health across the life-course: an updated systematic review and meta-analysis over 40 years. Osteoporos Int 30(4):741–761
Darling AL, Millward DJ, Torgerson DJ, Hewitt CE, Lanham-New SA (2009) Dietary protein and bone health: a systematic review and meta-analysis. Am J Clin Nutr 90(6):1674–1692
Palacios C (2006) The role of nutrients in bone health, from A to Z. Crit Rev Food Sci Nutr 46(8):621–628
Frost HM (1994) Wolff’s Law and bone’s structural adaptations to mechanical usage: an overview for clinicians. Angle Orthod 64(3):175–188
Wang L, You X, Lotinun S, Zhang L, Wu N, Zou W (2020) Mechanical sensing protein PIEZO1 regulates bone homeostasis via osteoblast-osteoclast crosstalk. Nat Commun 11(1):282
Blake GM, Fogelman I (2007) The role of DXA bone density scans in the diagnosis and treatment of osteoporosis. Postgrad Med J 83(982):509–517
Lorentzon M, Cummings SR (2015) Osteoporosis: the evolution of a diagnosis. J Intern Med 277(6):650–661
Unnanuntana A, Gladnick BP, Donnelly E, Lane JM (2010) The assessment of fracture risk. J Bone Joint Surg Am 92(3):743–753
Sözen T, Özışık L, Başaran NÇ (2017) An overview and management of osteoporosis. Eur J Rheumatol 4(1):46–56
Cauley JA (2011) Defining ethnic and racial differences in osteoporosis and fragility fractures. Clin Orthop Relat Res 469(7):1891–1899
Compston J, Cooper A, Cooper C, Gittoes N, Gregson C, Harvey N et al (2017) UK clinical guideline for the prevention and treatment of osteoporosis. Arch Osteoporos 12(1):43
Cosman F, de Beur SJ, LeBoff MS, Lewiecki EM, Tanner B, Randall S et al (2014) Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int 25(10):2359–2381
Mazziotti G, Canalis E, Giustina A (2010) Drug-induced osteoporosis: mechanisms and clinical implications. Am J Med 123(10):877–884
Oxford University (2010) Oxford dictionary of English, 3rd edn. Oxford University Press, Oxford
Berg KM, Kunins HV, Jackson JL, Nahvi S, Chaudhry A, Harris KA Jr et al (2008) Association between alcohol consumption and both osteoporotic fracture and bone density. Am J Med 121(5):406–418
Kanis JA, Johnell O (1999) The burden of osteoporosis. J Endocrinol Investig 22(8):583–588
Marsh D, Akesson K, Beaton DE, Bogoch ER, Boonen S, Brandi ML et al (2011) Coordinator-based systems for secondary prevention in fragility fracture patients. Osteoporos Int 22(7):2051–2065
Downey C, Kelly M, Quinlan JF (2019) Changing trends in the mortality rate at 1-year post hip fracture - a systematic review. World J Orthop 10(3):166–175
Chan S, Wong EKC, Ward SE, Kuan D, Wong CL (2019) The predictive value of the clinical frailty scale on discharge destination and complications in older hip fracture patients. J Orthop Trauma 33(10):497–502
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J et al (2001) Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 56(3):M146–M156
Rockwood K (2005) Frailty and its definition: a worthy challenge. J Am Geriatr Soc 53(6):1069–1070
Cooper C, Arden NK (2011) Excess mortality in osteoarthritis. BMJ 342:d1407
Hanson MA, Cooper C, Aihie Sayer A, Eendebak RJ, Clough GF, Beard JR (2016) Developmental aspects of a life course approach to healthy ageing. J Physiol 594(8):2147–2160
Rockwood K, Theou O (2020) Using the clinical frailty scale in allocating scarce health care resources. Can Geriatr J 23(3):210–215
England PH (2020) Falls: applying all our health: gov.uk. Updated 31 January 2020. https://www.gov.uk/government/publications/falls-applying-all-our-health/falls-applying-all-our-health
Lackoff AS, Hickling D, Collins PF, Stevenson KJ, Nowicki TA, Bell JJ (2020) The association of malnutrition with falls and harm from falls in hospital inpatients: findings from a 5-year observational study. J Clin Nurs 29(3–4):429–436
(NICE) NIfHaCE (2013) Falls in older people: assessing risk and prevention
Registry AaNZHF (2020) Annual report of hip fracture care. Annual report. Australian and New Zealand hip fracture registry, Registry AaNZHF, Sidney
Cheraghi Z, Doosti-Irani A, Almasi-Hashiani A, Baigi V, Mansournia N, Etminan M et al (2019) The effect of alcohol on osteoporosis: a systematic review and meta-analysis. Drug Alcohol Depend 197:197–202
Movassagh EZ, Vatanparast H (2017) Current evidence on the Association of Dietary Patterns and Bone Health: a scoping review. Adv Nutr 8(1):1–16
Royal Osteoporosis Society (2019) Strong, steady and straight: physical activity and exercise for osteoporosis quick guide: summary. https://theros.org.uk/media/0o5h1l53/ros-strong-steady-straight-quick-guide-february-2019.pdf
Fatoye F, Smith P, Gebrye T, Yeowell G (2019) Real-world persistence and adherence with oral bisphosphonates for osteoporosis: a systematic review. BMJ Open 9(4):e027049
Rampakakis E, Sampalis JS (2012) What can be done to maximize adherence of bisphosphonates in patients with osteoporosis? Int J Clin Rheumatol 7(4):361–364
Parsons CM, Harvey N, Shepstone L, Kanis JA, Lenaghan E, Clarke S et al (2020) Systematic screening using FRAX(®) leads to increased use of, and adherence to, anti-osteoporosis medications: an analysis of the UK SCOOP trial. Osteoporos Int 31(1):67–75
Yardley L, Donovan-Hall M, Francis K, Todd C (2006) Older people’s views of advice about falls prevention: a qualitative study. Health Educ Res 21(4):508–517
Marsh D, Mitchell P, Falaschi P, Beaupre L, Magaziner J, Seymour H et al (2021) The multidisciplinary approach to fragility fractures around the world: an overview. In: Falaschi P, Marsh D (eds) Orthogeriatrics: the management of older patients with fragility fractures. Springer International Publishing, Cham, pp 3–18
Dreinhöfer KE, Mitchell PJ, Bégué T, Cooper C, Costa ML, Falaschi P et al (2018) A global call to action to improve the care of people with fragility fractures. Injury 49(8):1393–1397
Riemen AHK, Hutchison JD (2016) The multidisciplinary management of hip fractures in older patients. Orthop Traumatol 30(2):117–122
Huntjens KM, van Geel TA, van den Bergh JP, van Helden S, Willems P, Winkens B et al (2014) Fracture liaison service: impact on subsequent nonvertebral fracture incidence and mortality. J Bone Joint Surg Am 96(4):e29
Jmmjyl J (1991) The illness experience: dimensions of suffering. Sage publications Inc., Thousand Oaks, CA
Neuburger J, Currie C, Wakeman R, Tsang C, Plant F, De Stavola B et al (2015) The impact of a national clinician-led audit initiative on care and mortality after hip fracture in England: an external evaluation using time trends in non-audit data. Med Care 53(8):686–691
Further Reading
Australian Commission on Safety and Quality in Health Care (2016) Hip fracture care clinical care standard. ACSQHC, Sydney safetyandquality.gov.au
Compston J, Cooper A, Cooper C et al (2017) UK clinical guideline for the prevention and treatment of osteoporosis. Arch Osteoporos 12:43
European Food Safety Authority (EFSA) (2016) Dietary reference values for vitamin D. EFSA panel on dietetic products, nutrition and allergies. https://doi.org/10.2903/j.efsa.2016.4547. https://efsa.onlinelibrary.wiley.com/
Scientific Advisory Committee on Nutrition (SACN) (2016) Vitamin D and health. https://www.gov.uk/government/groups/scientific-advisory-committee-on-nu
Royal College of Physicians. The Falls and Fragility Fracture Programme (FFFAP). https://www.fffap.org.uk/
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2021 The Author(s)
About this chapter
Cite this chapter
Wilson, H., Calcraft, D., Neville, C., Lanham-New, S., Durrant, L.R. (2021). Bone Health, Fragility and Fractures. In: Geirsdóttir, Ó.G., Bell, J.J. (eds) Interdisciplinary Nutritional Management and Care for Older Adults. Perspectives in Nursing Management and Care for Older Adults. Springer, Cham. https://doi.org/10.1007/978-3-030-63892-4_9
Download citation
DOI: https://doi.org/10.1007/978-3-030-63892-4_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-63891-7
Online ISBN: 978-3-030-63892-4
eBook Packages: MedicineMedicine (R0)