Abstract
Aims: To report the endovascular treatment and complications of intracranial and spinal dural arteriovenous (AV) fistulas. Methods: A retrospective analysis of 863 cases with dural AV fistulas was completed in the nationwide registry study of the Japanese Society of Neuroendovascular Therapy. Results: Treatments included transarterial/transvenous embolization (TAE/TVE), open surgery, stereotactic radiation, and their combinations. Modified Rankin Scale 0 (mRS-0) of the patients before and after treatment were 21% and 68%, and mRS 0-1were 69% and 86%, respectively. Mortality rate after treatment was 0.6%. Major complications of TAE and TVE were cranial nerve palsy and cerebral infarction. Conclusions: Major complications resulted from occlusion of vasa nervosum and material migration via dangerous intracranial and extracranial arterial anastomosis.
You have full access to this open access chapter, Download conference paper PDF
Similar content being viewed by others
Keywords
Dural arteriovenous fistulas (dAVF) are acquired lesions whose incidence is reported to be 0.3 per 100,000 per year [1]. The locations of the fistula include the cavernous sinus, transverse-sigmoid sinus, superior sagittal sinus, inferior and superior petrosal sinuses, anterior condylar confluence, tentorium, anterior skull base, craniocervical junction, convexity, and spinal cord. These lesions are divided into sinus type (the former six lesions) and non-sinus type (the latter five lesions).
The principle of dAVF therapy had been endovascular treatment for the sinus type and surgical treatment for the non-sinus type until Onyx was introduced as an embolic material. Nowadays the majority of non-sinus type dAVFs can be successfully treated with use of Onyx [2]. Current endovascular therapy includes transvenous coil embolization of the sinus type and transarterial glue or Onyx embolization of the non-sinus type. The aim of this study is to report complications that resulted from endovascular treatment of this disease.
Complication of Transarterial Embolization (TAE)
Migration Via the Arterial Anastomosis
One of the most important and critical complications is cerebral ischemia resulting from the migration of embolic materials via so-called dangerous anastomosis or the network between dural and pial arteries. Usually the dural branches of the external carotid artery have rich anastomosis with the dural and pial branches of the internal and vertebral arteries. Liquid embolic materials like NBCA (n-butyl cyanoacrylate) and Onyx, as well as particulate materials smaller than 200 μm, are easily migrating to the pial arteries via the network. One must care about another dangerous behavior of the liquid materials; it tends to come back to the parent feeding pedicle via the arterial network arising from the feeding artery itself (Fig. 1).
A case with dAVF in the craniocervical junction showing NBCA migration. (a) Preoperative vertebral angiogram indicating dAVF fed by C2 segmental artery of the vertebral artery and drained into the cerebral vein in the brain stem. (b) Microangiogram from the feeding artery. (c) Postoperative CT scan indicating migration of the fragmented pieces of NBCA. (d) Schematic drawing of the mechanism of NBCA migration; injected NBCA came back to the distal parent vertebral artery via the other feeding pedicle
Migration to the Venous Side
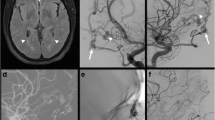
Onyx, particularly, tends to penetrate the arteriovenous fistula very easily and go to the venous side. This penetration is the essential phenomenon needed for the radical treatment and the most advantageous point of Onyx to the particulates. However, excessive penetration (migration) could occasionally result in the occlusion of the functioning cerebral veins (Fig. 2), causing potential venous infarction.
A case with Borden type-I dAVF involving the transverse-sigmoid sinus. The shunt was obliterated with Onyx injection from the distal occipital artery arising from the vertebral artery. A balloon catheter was inflated in the involved sinus to prevent Onyx migration to the sinus side. (a) Preoperative vertebral angiogram. (b) Postoperative vertebral angiogram indicating complete obliteration of the shunt. (c) Postoperative craniogram showing the Onyx cast. (d) Postoperative cone beam CT indicating Onyx migration to the tinny petrosal vein (arrow) via the superior petrosal sinus
NBCA tends to make fragmentation in the venous side when arterial blood flow comes from the other feeding arteries. If the block of fragment occludes the distal side of the draining vein, venous bleeding may occur because of the remaining arterial inflow.
Ischemia of the Vasa Nervosum
NBCA, Onyx, and small particulates (<200 μm) migrating into the vasa nervosum will cause cranial nerve palsy. Many external carotid branches like the middle meningeal, accessory meningeal, deep temporal artery, and the artery of foramen rotundum give rise to branches feeding the cranial nerves around the middle fossa. The middle meningeal, ascending pharyngeal, occipital artery, and posterior meningeal branch of the vertebral artery also feed the cranial nerves inside and outside the posterior fossa. The inferolateral and meningohypophyseal trunk of the internal carotid artery feed many cranial nerves and have a rich collateral anastomosis between external carotid artery.
Complication of Transvenous Embolization (TVE)
Mass Effect to the Cranial Nerves
Excessive transvenous coil packing of the cavernous sinus and anterior condylar confluence causes III, IV, V cranial nerve palsy and XII nerve palsy, respectively. Sometimes, the delayed ocular palsy will occur and never recover [3]. This mechanism still remains unknown but one should remind.
Venous Infarction and Bleeding
Normal cerebral veins sometimes drain into the involved sinus in an antegrade fashion. Venous infarction will occur after complete transvenous sinus packing by blocking the normal venous drainage (Fig. 3). Cortical venous drainage or retrograde leptomeningeal drainage in sinus type dAVFs is sometimes seen in Borden type II or III and Cognard type IIb. Transvenous sinus packing of these lesions have a potent complication of venous bleeding from excessive residual drainage to the cortical vein if the packing is incomplete (Fig. 4). One must obliterate, at first, the dangerous small draining veins like the uncal vein, petrosal vein, and bridging veins to the brain stem (Fig. 5).
A case with cavernous sinus dAVF treated with transvenous packing of the affected sinus. Left: Preoperative external carotid angiogram (lateral view) showing the shunt in the cavernous sinus. Center: Preoperative internal carotid angiogram (lateral view) showing the superficial middle cerebral veins are emptying into the affected cavernous sinus in an antegrade fashion. Right: Venous phase of the postoperative common carotid angiogram (lateral view). Note one of the superficial middle cerebral veins (arrow in the center figure) was missing
A case with cavernous sinus dAVF treated by transvenous coil embolization. Left: Preoperative common carotid angiogram. Center: Postoperative common carotid angiogram showing incomplete obliteration of the affected cavernous sinus. Note the cavernous sinus was packed with coils but the inferior petrosal sinus was still opacified (arrow). Right: MRI (FLAIR) examined in the next day showing (venous) infarction of the entire brain stem, suggesting the postoperative change of the draining route into the brain stem by incomplete transvenous occlusion of the cavernous sinus
Examples of the dangerous draining veins. Left: Cavernous sinus injection opacified the uncal vein (arrow) connecting with deep cerebral veins (vein of Rosenthal and vein of Galen). Center: Cavernous sinus injection opacified the petrosal vein (arrow). Right: Carotid angiogram showing the cavernous sinus dAVF draining only into the tinny vein of the brain stem (double arrows) via the bridging vein (arrow)
References
Kuwayama N (2016) Epidemiologic survey of dural arteriovenous fistulas in Japan: clinical frequency and present status of treatment. Acta Neurochir Suppl 123:185–188
Kim B, Jeon P, Kim K, Kim S, Kim H, Byun HS, Jo KI (2016) Predictive factors for response of intracranial dural arteriovenous fistulas to transarterial onyx embolization: angiographic subgroup analysis of treatment outcomes. World Neurosurg 88:609–618
Kashiwazaki D, Kuwayama N, Akioka N, Kuroda S (2014) Delayed abducens nerve palsy after transvenous coil embolization for cavernous sinus dural arteriovenous fistulae. Acta Neurochir 156:97–101
Conflict of Interest
The authors do not have a financial relationship with any organization.
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2021 The Author(s)
About this paper
Cite this paper
Kuwayama, N., Akioka, N. (2021). Complications of Endovascular Treatment of Intracranial Dural Arteriovenous Fistulas. In: Esposito, G., Regli, L., Cenzato, M., Kaku, Y., Tanaka, M., Tsukahara, T. (eds) Trends in Cerebrovascular Surgery and Interventions. Acta Neurochirurgica Supplement, vol 132. Springer, Cham. https://doi.org/10.1007/978-3-030-63453-7_18
Download citation
DOI: https://doi.org/10.1007/978-3-030-63453-7_18
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-63452-0
Online ISBN: 978-3-030-63453-7
eBook Packages: MedicineMedicine (R0)