Abstract
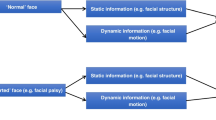
The most important goals for facial palsy patients receiving treatment is to be perceived as “normal” by society, and subsequently this is the most important goal for the reconstructive surgeon. The literature is abundant in descriptions of dynamic reanimation techniques, but less detailed on addressing asymmetry at rest. Facial palsy treatment should therefore not solely focus on restoring facial motion but also tone to obtain an optimal result. The exact chosen surgical approach depends on several variables as patient presentation (flaccid vs. partial vs. synkinesis), palsy duration (acute vs. subacute, vs. longstanding) and etiology (cancer vs. benign vs. infectious), nerve continuity (residual vs. reconstructed nerve continuity vs. no nerve continuity), and more. These factors and their influence on facial palsy treatment, more specifically the use of static support in combination with free muscle transfer will be elaborated on in this chapter. The most important message of this chapter is that, to achieve an optimal outcome, all available reconstructive and aesthetic surgical tools and the combination thereof must be considered despite of their perceived “classification.”
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Bradbury ET, Simons W, Sanders R. Psychological and social factors in reconstructive surgery for hemi-facial palsy. J Plast Reconstr Aesthet Surg. 2006;59(3):272–8.
Rozen SM. Discussion: symmetry restoration at rest after masseter-to-facial nerve transfer: is it as efficient as smile reanimation? Plast Reconstr Surg. 2017;140(4):802–4.
Dartt DA. Neural regulation of lacrimal gland secretory processes: relevance in dry eye diseases. Prog Retin Eye Res. 2009;28(3):155–77.
Husseman J, Mehta RP. Management of synkinesis. Facial Plast Surg. 2008;24(2):242–9.
Placheta E, Tzou CH, Hold A, Pona I, Frey M. Facial synkinesia before and after surgical reanimation of the paralyzed face. Plast Reconstr Surg. 2014;133(6):842e–51e.
Hembd A, Harrison B, Rocha CSM, Rocha FS, Chamseddin K, Labbe D, Cardenas-Mejia A, Rozen SM. Facial reanimation in the seventh and eighth decades of life. Plast Reconstr Surg. 2018;141(5):1239–51.
Hayashi A, Yoshizawa H, Natori Y, Suda S, Mochizuki M, Nishimuta Y, Tanaka R, Mizuno H. Assessment of T-shape double fascia graft for lower lip deformity from facial paralysis: a questionnaire survey. J Plast Reconstr Aesthet Surg. 2016;69(3):427–35.
Rozen S, Harrison B. Involuntary movement during mastication in patients with long-term facial paralysis reanimated with a partial gracilis free neuromuscular flap innervated by the masseteric nerve. Plast Reconstr Surg. 2013;132(1):110e–6e.
Garcia RM, Hadlock TA, Klebuc MJ, Simpson RL, Zenn MR, Marcus JR. Contemporary solutions for the treatment of facial nerve paralysis. Plast Reconstr Surg. 2015;135(6):1025e–46e.
Labbe D, Bussu F, Iodice A. A comprehensive approach to long-standing facial paralysis based on lengthening temporalis myoplasty. Acta Otorhinolaryngol Ital. 2012;32(3):145–53.
Rozen S, Lehrman C. Upper eyelid postseptal weight placement for treatment of paralytic lagophthalmos. Plast Reconstr Surg. 2013;131(6):1253–65.
Marten TJ. High SMAS facelift: combined single flap lifting of the jawline, cheek, and midface. Clin Plast Surg. 2008;35(4):569–603, vi–vii.
Trussler AP, Hatef D, Broussard GB, Brown S, Barton FE. The viscoelastic properties of the SMAS and its clinical translation: firm support for the high-SMAS rhytidectomy. Plast Reconstr Surg. 2011;128(3):757–64.
Terzis JK, Bruno W. Outcomes with eye reanimation microsurgery. Facial Plast Surg. 2002;18(2):101–12.
Chuang DC, Chang TN, Lu JC. Postparalysis facial synkinesis: clinical classification and surgical strategies. Plast Reconstr Surg Glob Open. 2015;3(3):e320.
Paletz JL, Manktelow RT, Chaban R. The shape of a normal smile: implications for facial paralysis reconstruction. Plast Reconstr Surg. 1994;93(4):784–9; discussion 790–781.
Labbe D, Benichou L, Iodice A, Giot JP. [Depressor anguli oris sign (DAO) in facial paresis. How to search it and release the smile (technical note)]. Ann Chir Plast Esthet. 2012;57(3):281–5.
Gur E, Zuker RM, Zaretski A, Leshem D, Barnea Y, Arad E, Yanko R, Meilik B, Kedar DJ, Fliss E. Incomplete facial paralysis - the use of the ipsilateral residual facial nerve as a donor nerve for facial reanimation. Plast Reconstr Surg. 2018;142:202.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Cornelissen, A.J.M., Rozen, S.M. (2021). Simultaneous Use of Static Support and Free Muscle Transfer. In: Tzou, CH.J., Rodríguez-Lorenzo, A. (eds) Facial Palsy. Springer, Cham. https://doi.org/10.1007/978-3-030-50784-8_20
Download citation
DOI: https://doi.org/10.1007/978-3-030-50784-8_20
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-50783-1
Online ISBN: 978-3-030-50784-8
eBook Packages: MedicineMedicine (R0)