Abstract
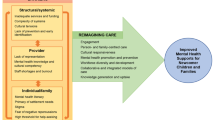
This chapter provides a brief overview of barriers that mental health practitioners face when working with refugee children and families and the importance of engaging with refugee communities in equitable partnerships in order to improve engagement in, and effectiveness of, family strengthening interventions. Challenges include stigma around mental health as well as formal mental healthcare systems not well adapted to meet the needs of refugee families. Practical barriers include the challenge of prioritizing addressing mental health problems, while refugee families are in the midst of dealing with competing stressors related to displacement or third country resettlement. Other issues arise within the clinical encounter, such as dependence on outside interpreters for communication between practitioners and clients, which make engaging in treatment challenging and undesirable. Authors draw upon their own experiences as refugee community leaders, healthcare professionals, and researchers engaged in community-based refugee mental health work to provide practical recommendations and strategies to overcome these barriers and work with refugee children and families.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Adolescent Health Initiative. Creating and sustaining a thriving youth advisory council. 2nd ed. Ann Arbor: The Adolescent Health Initiative at Michigan Medicine; 2019.
Beardslee WR. Prevention and the clinical encounter. Am J Orthopsychiatry. 1998;68(4):521–33. https://doi.org/10.1037/h0080361.
Beardslee WR, Gladstone TR, Wright EJ, Cooper AB. A family-based approach to the prevention of depressive symptoms in children at risk: evidence of parental and child change. Pediatrics. 2003;112(2):e119–31.
Beardslee WR, Wright EJ, Gladstone TR, Forbes P. Long-term effects from a randomized trial of two public health preventive interventions for parental depression. J Fam Psychol. 2007;21(4):703–13. https://doi.org/10.1037/0893-3200.21.4.703.
Betancourt TS, Berent JM, Freeman J, Frounfelker RL, Brennan RT, Abdi S, Maalim A, Abdi A, Mishra T, Gautam B, Creswell JW, Beardslee W. Family-based mental health promotion for Somali bantu and Bhutanese refugees: feasibility and acceptability trial. J Adolesc Health. 2020;66:336.
Betancourt TS, Frounfelker RL, Mishra T, Hussein A, Falzarano R. Addressing health disparities in the mental health of refugee children and adolescents through community-based participatory research: a study in two communities. Am J Public Health. 2015;105(S3):S475–82. https://doi.org/10.2105/AJPH.2014.302504.
Betancourt TS, Ng LC, Kirk CM, Munyanah M, Mushashi C, Ingabire C, Teta S, Beardslee WR, Brennan RT, Zahn I, Stulac S, Cyamatare FR, Sezibera V. Family-based prevention of mental health problems in children affected by HIV and AIDS: an open trial. AIDS. 2014;28(3):S359–68. https://doi.org/10.1097/2FQAD.0000000000000336.
Colucci E, Minas H, Szwarc J, Guerra C, Paxton G. In or out ? Barriers and facilitators to refugee-background young people accessing mental health services. Transcult Psychiatry. 2015;52(6):766–90. https://doi.org/10.1177/1363461515571624.
Colucci E, Valibhoy M, Szwarc J, Kaplan I, Minas H. Improving access to and engagement with mental health services among young people from refugee backgrounds: service user and provider perspectives. Int J Cult Mental Health. 2017;10(2):185–96. https://doi.org/10.1080/17542863.2017.1279674.
Ellis HB, Miller AB, Baldwin H, Abdi S. New directions in refugee youth mental health services: overcoming barriers to engagement. J Child Adolesc Trauma. 2011;4(1):69–85. https://doi.org/10.1080/19361521.2011.545047.
Fazel M, Garcia J, Stein A. The right location? Experiences of refugee adolescents seen by school-based mental health services. Clin Child Psychol Psychiatry. 2016;21(3):368–80. https://doi.org/10.1177/1359104516631606.
Fazel M, Betancourt TS. Preventive mental health interventions for refugee children and adolescents in high-income settings. Lancet Child Adolesc Health. 2017;2(2):121–32. https://doi.org/10.1016/S2352-4642(17)30147-5.
Inter-Agency Standing Committee (IASC). IASC guidelines on mental health and psychosocial support in emergency settings. Geneva: IASC; 2007. Retrieved from: https://www.who.int/mental_health/emergencies/guidelines_iasc_mental_health_psychosocial_june_2007.pdf
Israel BA, Schulz AJ, Parker EA, Becker AB. Review of community-based research: assessing partnership approaches to improve public health. Annu Rev Public Health. 1998;19(1):173–202. https://doi.org/10.1146/annurev.publhealth.19.1.173.
Karageorge A, Rodes P, Gray R, Papadopoulos R. Refugee and staff experiences of psychotherapeutic services: a qualitative systematic review. Intervention. 2017;15(1):51–69. https://doi.org/10.1097/WTF.0000000000000137.
Kohrt BA, Maharjan SM, Timsina D, Griffith JL. Applying Nepali ethnopsychology to psychotherapy for the treatment of mental illness and prevention of suicide among Bhutanese refugees. Ann Anthropological Pract. 2012;36(1):88–112. https://doi.org/10.1111/j.2153-9588.2012.01094.x.
LoIacono Merves M, Rodgers CR, Silver EJ, Sclafane JH, Bauman LJ. Engaging and sustaining adolescents in community-based participatory research: structuring a youth-friendly community-based participatory research environment. Family Commun Health. 2015;38(1):22–32.
Majumder P, O’Reilly M, Khalid K, Vostanis P. ‘This doctor, I do not trust him, I’m not safe’: the perceptions of mental health and services by unaccompanied refugee adolescents. Int J Soc Psychiatry. 2015;61(2):129–36. https://doi.org/10.1177/0020764014537236.
Miller KE. Rethinking a familiar model: psychotherapy and the mental health of refugees. J Contemp Psychother. 1999;29(4):283–306. https://doi.org/10.1023/A:1022926721458.
Minkler M. Linking science and policy through community-based participatory research to study and address health disparities. Am J Public Health. 2010;100(S1):S81–7. https://doi.org/10.2105/AJPH.2009.165720.
Murray KE, Davidson GR, Schweitzer RD. Review of refugee mental health interventions following resettlement: best practices and recommendations. Am J Orthopsychiatry. 2010;80(4):576–85. https://doi.org/10.1111/j.1939-0025.2010.01062.x.
Pejic V, Alvarado AE, Hess RS, Groark S. Community-based interventions with refugee families using a family systems approach. Fam J. 2017;25(1):101–8. https://doi.org/10.1177/1066480716680189.
Pejic V, Hess RS, Miller GE, Wille A. Family first: community-based supports for refugees. Am J Orthopsychiatry. 2016;86(4):409–14. https://doi.org/10.10337/ort0000189.
Priebe S, Giacco D, El-Nagib R. Public health aspects of mental health among migrants and refugees: a review of the evidence on mental health care for refugees, asylum seekers and irregular migrants in the WHO European Region. Copenhagen: WHO Regional Office for Europe; 2016.
Saechao F, Sharrock S, Reicherter D, Livingston JD, Aylward A, Whisnant J, Koopman C, Kohli S. Stressors and barriers to using mental health services among diverse groups of first-generation immigrants to the United States. Community Ment Health J. 2012;48(1):98–106. https://doi.org/10.1007/s10597-011-9419-4.
Scuglik DL, Alacoon RD, Lapeyre AC, Williams MD, Logan KM. When the poetry no longer rhymes: mental health issues among Somali immigrants in the USA. Transcult Psychiatry. 2007;44(4):581–95. https://doi.org/10.1177/1363461507083899.
Shannon PJ. Refugees’ advice to physicians: how to ask about mental health. Fam Pract. 2014;31(4):462–6. https://doi.org/10.1093/fampra/cmu017.
Shannon PJ, Wieling E, Simmelink-McCleary J, Becher E. Beyond stigma: barriers to discussing mental health in refugee populations. J Loss Trauma. 2015;20(3):281–96. https://doi.org/10.1080/15325024.2014.934629.
Singh NN, McKay JD, Singh AN. The need for cultural brokers in mental health services. J Child Fam Stud. 1999;8(1):1–10. https://doi.org/10.1023/A:1022949225965.
Svenberg K, Skott C, Lepp M. Ambiguous expectations and reduced confidence: experience of Somali refugees encountering Swedish health care. J Refug Stud. 2011;24(4):690–705. https://doi.org/10.1093/jrs/fer026.
UNHCR. A community-based approach in UNHCR operations. Geneva. 2008. Retrieved from: https://www.refworld.org/pdfid/47da54722.pdf.
UNHCR. Understanding community-based protection. Protection Policy Paper. Geneva. 2013. Retrieved from: https://www.refworld.org/pdfid/5209f0b64.pdf.
UNHCR. Community-based protection and mental health & psychosocial support. Geneva. 2017. Retrieved from: https://www.refworld.org/docid/593ab6add.html.
Valibhoy MC, Kaplan I, Szwarc J. “It comes down to just how human someone can be”: a qualitative study with young people from refugee backgrounds about their experiences of Australian mental health services. Transcult Psychiatry. 2017;54(1):23–45. https://doi.org/10.1177/1363461516662810.
Valibhoy MC, Szwarc J, Kaplain I. Young services users from refugee backgrounds: their perspectives on barriers to access Australian mental health services. Int J Human Rights in Healthc. 2017;10(1):68–80. https://doi.org/10.1108/IJHRH-07-20160010.
Wallace NM, Berent JM, McCarthy TG, Senn TE, Carey M. Recruitment and retention of low-income, urban participants in a longitudinal study: recognizing and strengthening participants’ motivations. Behav Ther. 2014;37(8):226–30.
Wallerstein NB, Duran B. Using community-based participatory research to address health disparities. Health Promot Pract. 2006;7(3):312–23. https://doi.org/10.1177/1524839906289376.
Weine SM. Family roles in refugee youth resettlement from a prevention perspective. Child Adolesc Psychiatr Clin N Am. 2008;17(3):515–32. https://doi.org/10.1016/j.chc.2008.02.006.
Weine SM. Developing preventive mental health interventions for refugee families in resettlement. Fam Process. 2011;50(3):410–30. https://doi.org/10.1111/j.1545-5300.2011.01366.x.
Weissbecker I, Hanna F, El Shazly M, Gao J, Ventevogel P. Integrative mental health and psychosocial support interventions for refugees in humanitarian crisis settings. In: Wenzel T, Drozdek B, editors. Uncertain safety: understanding and assisting the 21st century refugees. Cham: Springer; 2019. p. 117–53.
Wong EC, Marshall GN, Schell TL, Elliot MN, Hambarsoomians K, Chung CA, Berthold SM. Barriers to mental health care utilization for U.S. Cambodian refugees. J Consult Clin Psychol. 2006;74(6):1116–20. https://doi.org/10.1037/0022-006X.74.6.1116.
Young M, Chan KJ. School-based interventions for refugee children and youth: Canadian and international perspectives. In: Brewer CA, McCabe M, editors. Immigrant and refugee students in Canada. Edmonton: Brush Education; 2014. p. 31–53.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Frounfelker, R.L., Mishra, T., Gautam, B., Berent, J.M., Abdi, A., Betancourt, T.S. (2020). Engaging Refugee Families in a Family-Strengthening Intervention to Promote Child Mental Health and Family Functioning. In: Song, S., Ventevogel, P. (eds) Child, Adolescent and Family Refugee Mental Health. Springer, Cham. https://doi.org/10.1007/978-3-030-45278-0_16
Download citation
DOI: https://doi.org/10.1007/978-3-030-45278-0_16
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-45277-3
Online ISBN: 978-3-030-45278-0
eBook Packages: MedicineMedicine (R0)