Abstract
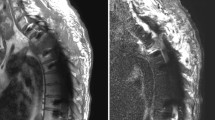
The spine is the most common site for skeletal metastasis. As improved treatment for primary cancer affords longer life expectancy, the incidence of spinal metastasis is increasing. Patients generally present with neck or back pain with or without neurological symptoms such as radicular pain, numbness, weakness, or myelopathy. Surgical treatment is palliative and is often used in conjunction with radiation and/or chemotherapy. The goals of surgery include mechanical stabilization, decompression of the neural elements, and optimization of the radiation target. The number of metastatic tumor patients undergoing surgery is growing. In spite of increased rates of surgical treatment, improved hardware and refined technique, the rate of surgery-related complications remains high. The most common complications are dural injury, wound infection and dehiscence, and hardware failure. The extent and severity of these complications can be mitigated by preoperative risk assessment with appropriate goal identification, intraoperative technique, and early recognition of postoperative deterioration.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Kakhki VR, et al. Pattern and distribution of bone metastases in common malignant tumors. Nucl Med Rev Cent East Eur. 2013;16(2):66–9.
Campbell PG, et al. Patient comorbidity score predicting the incidence of perioperative complications: assessing the impact of comorbidities on complications in spine surgery. J Neurosurg Spine. 2012;16(1):37–43.
Reis RC, et al. Risk of complications in spine surgery: a prospective study. Open Orthop J. 2015;9:20–5.
Nair S, et al. Preoperative embolization of hypervascular thoracic, lumbar, and sacral spinal column tumors: technique and outcomes from a single center. Interv Neuroradiol. 2013;19(3):377–85.
Robial N, et al. Is preoperative embolization a prerequisite for spinal metastases surgical management? Orthop Traumatol Surg Res. 2012;98(5):536–42.
Prince EA, Ahn SH. Interventional management of vertebral body metastases. Semin Intervent Radiol. 2013;30(3):278–81.
Wilson MA, et al. Retrospective analysis of preoperative embolization of spinal tumors. AJNR Am J Neuroradiol. 2010;31(4):656–60.
Hong CG, et al. Preoperative embolization in patients with metastatic spinal cord compression: mandatory or optional? World J Surg Oncol. 2017;15(1):45.
Wise JJ, et al. Complication, survival rates, and risk factors of surgery for metastatic disease of the spine. Spine (Phila Pa 1976). 1999;24(18):1943–51.
Omeis IA, et al. Postoperative surgical site infections in patients undergoing spinal tumor surgery: incidence and risk factors. Spine (Phila Pa 1976). 2011;36(17):1410–9.
Demura S, et al. Surgical site infection in spinal metastasis: risk factors and countermeasures. Spine (Phila Pa 1976). 2009;34(6):635–9.
Kumar N, et al. Blood loss and transfusion requirements in metastatic spinal tumor surgery: evaluation of influencing factors. Ann Surg Oncol. 2016;23(6):2079–86.
Kumar S, et al. Risk factors for wound infection in surgery for spinal metastasis. Eur Spine J. 2015;24(3):528–32.
Sebaaly A, et al. Surgical site infection in spinal metastasis: incidence and risk factors. Spine J. 2018;18(8):1382–7.
Sampedro MF, et al. A biofilm approach to detect bacteria on removed spinal implants. Spine (Phila Pa 1976). 2010;35(12):1218–24.
Levi AD, Dickman CA, Sonntag VK. Management of postoperative infections after spinal instrumentation. J Neurosurg. 1997;86(6):975–80.
Weinstein MA, McCabe JP, Cammisa FP Jr. Postoperative spinal wound infection: a review of 2,391 consecutive index procedures. J Spinal Disord. 2000;13(5):422–6.
O’Neill KR, et al. Reduced surgical site infections in patients undergoing posterior spinal stabilization of traumatic injuries using vancomycin powder. Spine J. 2011;11(7):641–6.
Okafor R, et al. Intrawound vancomycin powder for spine tumor surgery. Global Spine J. 2016;6(3):207–11.
Hey HW, et al. Is intraoperative local vancomycin powder the answer to surgical site infections in spine surgery? Spine (Phila Pa 1976). 2017;42(4):267–74.
Sweet FA, Roh M, Sliva C. Intrawound application of vancomycin for prophylaxis in instrumented thoracolumbar fusions: efficacy, drug levels, and patient outcomes. Spine (Phila Pa 1976). 2011;36(24):2084–8.
Pahys JM, et al. Methods to decrease postoperative infections following posterior cervical spine surgery. J Bone Joint Surg Am. 2013;95(6):549–54.
Godil SS, et al. Comparative effectiveness and cost-benefit analysis of local application of vancomycin powder in posterior spinal fusion for spine trauma: clinical article. J Neurosurg Spine. 2013;19(3):331–5.
Chang DW, Friel MT, Youssef AA. Reconstructive strategies in soft tissue reconstruction after resection of spinal neoplasms. Spine (Phila Pa 1976). 2007;32(10):1101–6.
Garvey PB, et al. Immediate soft-tissue reconstruction for complex defects of the spine following surgery for spinal neoplasms. Plast Reconstr Surg. 2010;125(5):1460–6.
Chahoud J, Kanafani Z, Kanj SS. Surgical site infections following spine surgery: eliminating the controversies in the diagnosis. Front Med (Lausanne). 2014;1:7.
Mesfin A, et al. Changing the adverse event profile in metastatic spine surgery: an evidence-based approach to target wound complications and instrumentation failure. Spine (Phila Pa 1976). 2016;41 Suppl 20:S262–s270.
Janssen DMC, et al. A retrospective analysis of deep surgical site infection treatment after instrumented spinal fusion with the use of supplementary local antibiotic carriers. J Bone Joint Infect. 2018;3(2):94–103.
Vitaz TW, et al. Rotational and transpositional flaps for the treatment of spinal wound dehiscence and infections in patient populations with degenerative and oncological disease. J Neurosurg. 2004;100(1 Suppl Spine):46–51.
Chieng LO, et al. Reconstruction of open wounds as a complication of spinal surgery with flaps: a systematic review. Neurosurg Focus. 2015;39(4):E17.
Menon SK, Onyia CU. A short review on a complication of lumbar spine surgery: CSF leak. Clin Neurol Neurosurg. 2015;139:248–51.
Ghobrial GM, et al. Iatrogenic neurologic deficit after lumbar spine surgery: a review. Clin Neurol Neurosurg. 2015;139:76–80.
Weber C, Piek J, Gunawan D. Health care costs of incidental durotomies and postoperative cerebrospinal fluid leaks after elective spinal surgery. Eur Spine J. 2015;24(9):2065–8.
Guerin P, et al. Incidental durotomy during spine surgery: incidence, management and complications. A retrospective review. Injury. 2012;43(4):397–401.
Tafazal SI, Sell PJ. Incidental durotomy in lumbar spine surgery: incidence and management. Eur Spine J. 2005;14(3):287–90.
Niu T, et al. Postoperative cerebrospinal fluid leak rates with subfascial epidural drain placement after intentional durotomy in spine surgery. Global Spine J. 2016;6(8):780–5.
Pannullo SC, et al. MRI changes in intracranial hypotension. Neurology. 1993;43(5):919–26.
Tosun B, et al. Management of persistent cerebrospinal fluid leakage following thoraco-lumbar surgery. Asian Spine J. 2012;6(3):157–62.
Gautschi OP, et al. Incidental durotomy in lumbar spine surgery – is there still a role for flat bed rest? Spine J. 2014;14(10):2522–3.
Gautschi OP, et al. Incidental durotomy in lumbar spine surgery–a three-nation survey to evaluate its management. Acta Neurochir. 2014;156(9):1813–20.
Hu P, et al. A circumferential decompression-based surgical strategy for multilevel ossification of thoracic posterior longitudinal ligament. Spine J. 2015;15(12):2484–92.
Hu PP, Liu XG, Yu M. Cerebrospinal fluid leakage after thoracic decompression. Chin Med J. 2016;129(16):1994–2000.
Mazur M, et al. Management of cerebrospinal fluid leaks after anterior decompression for ossification of the posterior longitudinal ligament: a review of the literature. Neurosurg Focus. 2011;30(3):E13.
Cho JY, et al. Management of cerebrospinal fluid leakage after anterior decompression for ossification of posterior longitudinal ligament in the thoracic spine: the utilization of a volume-controlled pseudomeningocele. J Spinal Disord Tech. 2012;25(4):E93–102.
Fang Z, et al. Subfascial drainage for management of cerebrospinal fluid leakage after posterior spine surgery–a prospective study based on Poiseuille’s law. Chin J Traumatol. 2016;19(1):35–8.
Quraishi NA, et al. Reoperation rates in the surgical treatment of spinal metastases. Spine J. 2015;15(3 Suppl):S37–43.
Pedreira R, et al. Hardware failure in patients with metastatic cancer to the spine. J Clin Neurosci. 2017;45:166–71.
Amankulor NM, et al. The incidence and patterns of hardware failure after separation surgery in patients with spinal metastatic tumors. Spine J. 2014;14(9):1850–9.
Moon BJ, et al. Polymethylmethacrylate-augmented screw fixation for stabilization of the osteoporotic spine : a three-year follow-up of 37 patients. J Korean Neurosurg Soc. 2009;46(4):305–11.
Frankel BM, Jones T, Wang C. Segmental polymethylmethacrylate-augmented pedicle screw fixation in patients with bone softening caused by osteoporosis and metastatic tumor involvement: a clinical evaluation. Neurosurgery. 2007;61(3):531–7; discussion 537–8.
Jang JS, et al. Polymethylmethacrylate-augmented screw fixation for stabilization in metastatic spinal tumors. Technical note. J Neurosurg. 2002;96(1 Suppl):131–4.
Amendola L, et al. Fenestrated pedicle screws for cement-augmented purchase in patients with bone softening: a review of 21 cases. J Orthop Traumatol. 2011;12(4):193–9.
Fransen P. Increasing pedicle screw anchoring in the osteoporotic spine by cement injection through the implant. Technical note and report of three cases. J Neurosurg Spine. 2007;7(3):366–9.
Yoshioka K, et al. Prevalence and risk factors for development of venous thromboembolism after degenerative spinal surgery. Spine (Phila Pa 1976). 2015;40(5):E301–6.
Zacharia BE, et al. Incidence and risk factors for preoperative deep venous thrombosis in 314 consecutive patients undergoing surgery for spinal metastasis. J Neurosurg Spine. 2017;27(2):189–97.
Ferree BA, Wright AM. Deep venous thrombosis following posterior lumbar spinal surgery. Spine (Phila Pa 1976). 1993;18(8):1079–82.
Gerlach R, et al. Postoperative nadroparin administration for prophylaxis of thromboembolic events is not associated with an increased risk of hemorrhage after spinal surgery. Eur Spine J. 2004;13(1):9–13.
Fukuda W, et al. Management of pulmonary thromboembolism based on severity and vulnerability to thrombolysis. Ann Vasc Dis. 2017;10(4):371–7.
Luksanapruksa P, et al. Perioperative complications of spinal metastases surgery. Clin Spine Surg. 2017;30(1):4–13.
Scavarda D, et al. [Postoperative spinal extradural hematomas. 14 cases]. Neurochirurgie. 1997;43(4):220–7.
Ziewacz JE, et al. The design, development, and implementation of a checklist for intraoperative neuromonitoring changes. Neurosurg Focus. 2012;33(5):E11.
Ryken TC, et al. The acute cardiopulmonary management of patients with cervical spinal cord injuries. Neurosurgery. 2013;72(Suppl 2):84–92.
Yue JK, et al. Update on critical care for acute spinal cord injury in the setting of polytrauma. Neurosurg Focus. 2017;43(5):E19.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Yasin, B., Virk, M.S. (2020). Postoperative Complications and Spinal Metastases. In: Ramakrishna, R., Magge, R., Baaj, A., Knisely, J. (eds) Central Nervous System Metastases. Springer, Cham. https://doi.org/10.1007/978-3-030-42958-4_45
Download citation
DOI: https://doi.org/10.1007/978-3-030-42958-4_45
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-42957-7
Online ISBN: 978-3-030-42958-4
eBook Packages: MedicineMedicine (R0)