Summary
Anthropogenic emissions have transformed atmospheric composition to the extent that biogeochemical cycles, air quality, and climate have changed globally and profoundly. It is estimated that ambient (outdoor) air pollution causes an excess mortality rate of about 4.5 million per year, associated with 122 million years of life lost annually, mostly due to the detrimental health effects of fine particulate matter (PM2.5). Globally, the largest source of this pollution is residential energy use for heating and cooking, notably because of its importance in Asia. Agriculture, power production, and road traffic also contribute significantly. If residential energy emissions could be eliminated, up to 1.4 million deaths per year would be avoided. Agriculture, through the release of ammonia, contributes strongly to PM2.5. A study of health benefits achieved through European legislation since 1970 indicates that emission controls in the transport and energy sectors have prevented approximately 61,000 deaths per year in Europe and 163,000 per year worldwide, the latter through new technology that penetrated global markets. However, much stronger measures are needed to substantially lower the health burden from air pollution. Clean air is a human right, being fundamental to many sustainable development goals of the United Nations, such as good health, climate action, sustainable cities, clean energy, and protecting life on land and in the sea.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Although air pollution episodes have been documented since antiquity by the Greeks and Romans, public health concerns with smog emerged with urbanization and industrialization, such as in London after World War II. The burning of wood and coal for power generation, heating, and cooking releases sulfur dioxide (SO2), nitrogen oxides (NOx = NO + NO2), and carbon-containing compounds from which fine aerosol particles are formed through atmospheric chemistry. London’s smog is typically dominated by sulfur compounds, whereas photochemical smog in Los Angeles, for example, is characterized by high levels of ozone (O3), formed from hydrocarbons and NOx under the influence of sunlight. During the “great acceleration” of the Anthropocene in the middle of the twentieth century (Crutzen, 2002; Steffen, Grinevald, Crutzen, & McNeill, 2011), transboundary air pollution reached regional dimensions, accompanied by the degradation of ecosystems through the deposition of atmospheric sulfur and nitrogen compounds. In recent decades, widespread pollution emissions from traffic, industry, energy production, agriculture, and biomass burning across all continents have emerged into a global challenge.
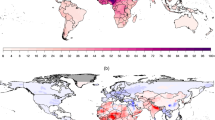
The chief pollutant that has been related to health outcomes is fine particulate matter, which are aerosols with diameters less than 2.5 μm (PM2.5), followed by O3, which is a strong oxidant. Depending on size, fine particles can penetrate deeply into the lungs, and the smallest ones even reach the bloodstream and affect other organs. Based on emission inventories, satellite observations, measurement data from monitoring networks, and model calculations, it has been unambiguously documented that air quality has degraded on regional and global scales (Akimoto, 2003; Anenberg, Horowitz, Tong, & West, 2010; Lelieveld & Dentener, 2000; Van Donkelaar et al., 2010; Wang & Mauzerall, 2006) (Fig. 9.1). In parallel, evidence that air pollutants adversely impact human health, based on epidemiological studies, has mounted (Burnett et al., 2014; Cohen et al., 2017; Dockery et al., 1993; Lim et al., 2012; Pope et al., 2002). The diseases incited by the long-term exposure to air pollution include acute lower respiratory infections, chronic obstructive pulmonary disease, cerebrovascular disease, ischemic heart disease, and lung cancer. This chapter uses a global model to estimate the health burden from air pollution, and especially how it can be avoided by reducing emissions.
Global mean PM2.5 in the period 2010–2012 derived from satellite observations (NASA). The World Health Organization (WHO) estimates that 90% of people on Earth are exposed to PM2.5 concentrations higher than the air quality guideline of 10 μg/m3 (see also Brauer et al., 2016)
Methods: Earth System Chemistry Model
We used the ECHAM/MESSy Atmospheric Chemistry (EMAC) computer model that comprehensively simulates meteorological and atmospheric chemical processes worldwide. It has been developed at the Max Planck Institute for Chemistry in Mainz, building on the climate model of the Max Planck Institute for Meteorology in Hamburg (Roeckner et al., 2006). EMAC couples atmosphere, ocean, and land processes to simulate biogeochemical cycles of reactive compounds. Therefore, it can be seen as an Earth system chemistry model, which can cover a wide range of space and time scales, typically up to decades or centuries (Pozzer, Jöckel, Kern, & Haak, 2011). Currently, the EMAC development is pursued by an international consortium (see http://www.messy-interface.org for details and references). The model can be applied at various horizontal resolutions (between about 50 and 250 km grid spacing), and covers the lower and middle atmosphere (Jöckel et al., 2006, 2010). Here, we use EMAC to investigate the global impact of growing air pollution emissions in recent years and also to determine possible chemical states of the atmosphere up to the middle of the twenty-first century, applying a grid spacing of ~100 km latitude/longitude. Air pollution emissions have been adopted from the Emission Database for Global Atmospheric Research (EDGAR) (http://edgar.jrc.ec.europa.eu/).
Model calculations have been extensively tested against measurement data of gases and particles from ground-based air quality networks and global observations from satellites (e.g., Karydis, Tsimpidi, Pozzer, Astitha, & Lelieveld, 2016; Karydis et al., 2017; Lelieveld, Gromov, Pozzer, & Taraborrelli, 2016; Pozzer et al., 2012a, 2012b; Tsimpidi, Karydis, Pandis, & Lelieveld, 2016). To compute the public health impacts attributable to air pollution, the model simulations have been combined with integrated exposure–response (IER) functions that use annual mean pollution concentrations to assess long-term health outcomes, following Anenberg et al. (2010), Lim et al. (2012), Burnett et al. (2014), and Lelieveld, Evans, Fnais, Giannadaki, and Pozzer (2015). We applied the updated IER coefficients according to the Global Burden of Disease (GBD, 2017) and Cohen et al. (2017) to compute the relative risk of mortality by cardiovascular and respiratory diseases and lung cancer (Lelieveld, 2017). Data sets used as inputs, such as country-level baseline mortality rates for the different disease categories and population data, have been adopted from the WHO Global Health Observatory (www.who.int/gho/database/en/), being representative of the year 2015.
Multi-pollutant Index (MPI)
Considering that human health is affected by multiple gas and aerosol species, it is helpful to combine them into an air quality metric, accounting for the so-called criteria pollutants SO2, NO2, carbon monoxide (CO), O3 and PM2.5, for which many countries have implemented control measures based on health standards. To assess air quality changes globally, regionally and nationally, and also account for the number of people subjected to poor air conditions, we adopted a Multi-pollutant Index, MPI (Pozzer et al., 2012b). The index is population weighted to represent the impact on public health. The scale extends from −1 to infinity, whereby levels above zero indicate poor air quality according to the pollution thresholds of the WHO for the criteria pollutants. Figure 9.2 compares the air quality development in seven regions since preindustrial times.
Figure 9.2 illustrates the differences between regions and the time development in the Anthropocene, that is, since the preindustrial period. For example, in the Middle East, air quality has been relatively low even without human-induced emissions, related to the high concentration of airborne desert dust, which has a significant impact on human health (Giannadaki, Pozzer, & Lelieveld, 2014). Figure 9.2 also includes results from future projections with the EMAC model according to a business-as-usual (BaU) emission scenario for the years 2025 and 2050 (Pozzer et al., 2012b). BaU means that only current legislation is being considered in the modeled emission scenario. Therefore, the projections represent the present trajectory into the future.
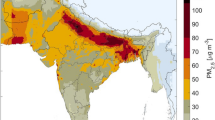
The largest changes in the population-weighted MPI occurred during industrialization in the twentieth century, that is, between the preindustrial period and 2005. This is related to the rapidly growing pollution emissions, especially since the middle of the twentieth century (the great acceleration), which strongly impacted air quality for a large fraction of the world population. Although the changes between 2005 and 2050 are smaller, they partly occur rather abruptly. In Europe, the Americas and Africa, the anticipated MPI differences are incremental; however, in economically emerging regions, such as East Asia, very rapid increases have taken place, and may continue in the near future, especially in South Asia (Fig. 9.3). On a global scale, the population-weighted MPI has increased from −0.63 (PI) to −0.13 in 2005, and an additional strong increase up to +0.18 is projected until 2050. This implies that the BaU scenario will lead to worldwide violation of WHO air quality standards.
Figure 9.3 presents the projected population-weighted MPI increase per country. Under the BaU scenario, India may experience the strongest air quality degradation, followed by Bangladesh and China. Figure 9.3 also includes countries in the Middle East where both air pollution and population growth are rapid; hence, many more people may become exposed to poor air quality. The large, densely populated countries with high levels of air pollution, notably in Asia, relatively strongly affect the global mean decline of air quality, and thus adversely influence the health conditions of the “average citizen.” Note that Asia is projected to continually dominate the world population (about four of globally seven billion in 2010, and about five of globally nine billion in 2050). Further, it is expected that the urban population will grow relatively rapidly from 3.6 billion in 2010 to 5.2 billion in 2050.
Health Impacts of Air Pollution
The model results have been combined with integrated exposure–response (IER) functions. We computed the relative risk of mortality by acute lower respiratory infections (ALRI) in childhood, chronic obstructive pulmonary disease (COPD), cerebrovascular disease (CEV) leading to mortality by ischemic and hemorrhagic strokes (CEVI and CEVH, respectively), ischemic heart disease (IHD) leading to mortality by heart attacks, and lung cancer (LC). These diseases are related to PM2.5, while COPD is additionally related to O3 (Fig. 9.4). Our methodology follows that of the Global Burden of Disease for 2010 (Lim et al., 2012), being updated for the year 2015 (GBD, 2017).
The minimum risk exposure level distribution for annual mean PM2.5, applied in the IER functions, is 2.4–5.9 μg/m3, which is lower than the previously assumed range of 5.8–8.8 μg/m3 for the Global burden of Disease 2010, and that of O3 is 33.3–41.9 ppbv (unchanged). The recent downward adjustment of the “safe threshold” for PM2.5 is the main reason for the higher mortality rates presented here compared to previous estimates for 2010, since a larger fraction of the population is exposed to hazardous levels of air pollution. In particular, the mortality rates for COPD are significantly higher than reported previously. Thus, the state-of-the-science is that only very low mean PM2.5 concentrations under 4.2 ± 1.8 μg/m3 do not significantly contribute to morbidity and mortality. The global results presented here agree with the GBD for the year 2015, on average within a few percent.
The updated calculations indicate a total excess mortality rate attributable to ambient (outdoor) air pollution of 4.5 million persons per year, which is about a third higher than estimated previously by Lelieveld et al. (2015) and the GBD for the year 2010 (Lim et al., 2012). The statistical uncertainty range is estimated at 3.4–5.6 million per year (95% confidence interval), hence approximately ±25%, being dominated by uncertainties in the IER functions and to a lesser extent to estimates of annual mean pollution concentrations (Kushta, Pozzer, & Lelieveld, 2018). Note that the IER functions for very high levels of PM2.5 are associated with relatively large uncertainty, as epidemiological data for such conditions are scarce.
The estimated mortality attributable to air pollution is about 265,000 per year in the EU-28, 373,000 per year for Europe as a whole (not including Russia), and 120,000 per year for the United States. The global total number of years of life lost (YLL) is about 122 million per year (92–148 million per year), which implies that each individual who dies from diseases incited by air pollution loses about 28 ± 7 years of his or her life. The life expectancy reduction is greatest for ALRI as it also affects children, especially in countries where nutrition and medical care are inadequate, being on average 54 years, and 20–25 years for the other disease categories. Among the leading GBD risk factors, ambient particulate matter pollution ranks fifth, after high blood pressure, tobacco smoking, diabetes, and being overweight (GBD, 2017). Poor air quality is the largest environmental risk factor worldwide.
To put the problem in perspective, the WHO estimates that the number of people who die annually from malaria and HIV/AIDS together is about 1.5 million, which is roughly one third compared to outdoor air pollution. The additional mortality attributable to household (indoor) air pollution is about 2.9 million per year (GBD, 2017). Even though the global implementation of the WHO air quality guideline for PM2.5 of 10 μg/m3 would significantly reduce mortality attributable to air pollution by more than 50% (Giannadaki, Pozzer, & Lelieveld, 2016), this threshold is still too high, especially because the minimum risk exposure level has decreased to 4.2 ± 1.8 μg/m3 (Lelieveld & Pöschl, 2017). While the control of emissions in polluted regions such as South and East Asia and Eastern Europe has a high potential to reduce mortality, air quality improvements at relatively low concentrations still have major health benefits because of the nonlinear response to exposure (Cohen et al., 2017).
Table 9.1 ranks the countries where mortality exceeds 30,000 individuals per year. China and India lead, partly related to their large population size because comparatively large numbers of people are exposed to poor air quality. The attribution to source sectors in Table 9.1 has been adopted from Lelieveld et al. (2015), calculated by omitting the respective emissions in the EMAC model. These results represent the elimination of source categories one at a time, which to a large extent represents the efficiency of PM2.5 reductions by controlling these sources, as mortality attributable to O3 represents only 6% of the total. On a global scale, residential energy use for heating and cooking is the largest source category (31%), notably because it is the major one in Asia. In eastern Asia and Europe, agricultural emissions are important, such as ammonia (NH3) from animal husbandry and fertilizer use, because this gas is an effective precursor of PM2.5 (Pozzer, Tsimpidi, Karydis, de Meij, & Lelieveld, 2017).
World Avoided by Improving Technology in the EU
To illustrate the effectiveness of air pollution legislation and the consequent public health improvement in the past, an emission scenario was adopted, which accounts for trends in gaseous and particulate pollution sources in the period 1970–2010 (Crippa et al., 2016). The scenario focuses on the EU where the EURO norms for light- and heavy-duty vehicles have been introduced. The EU additionally imposed standards on fuel quality and flue gas desulfurization in the power production sector. The measures taken in the EU not only impacted European air pollution but also worldwide, because the EURO standards penetrated global markets through European and Japanese manufacturers, thus effectively exporting EU regulations. The scenario assesses end-of-pipe reduction measures in the EU by comparing actual emissions to historical fuel consumption along with a stagnation of technology, by applying constant emission factors since 1970, that is, without abatement measures imposed by European emission standards. It includes three regulated sectors—power generation, manufacturing industry and road traffic—which together account for 28% of mortality attributable to air pollution (Table 9.1).
The scenario calculations indicate that, without emission regulation, the European sources of SO2 and NOx would have been about 70% and PM2.5 would have been a factor of 2.3 higher in 2010 compared to 1970, mainly due to end-of-pipe controls (Crippa et al., 2016). The model calculations suggest that regulation of the road transport sector has made a relatively large contribution to emission control of SO2, NOx, non-methane hydrocarbons (NMHC), and PM2.5 (including black and organic carbon, BC and OC), while power production also contributed strongly, particularly to the reduction of SO2 and PM2.5. In Europe, the 2010 emissions by industry were higher than from power production, as abatement strategies for this sector have been less stringent. Globally, European emission controls in power production have played a significant role in reducing SO2 and BC, and road traffic in the reduction of NMHC, NOx, and BC emissions. Power production was still the largest contributor to SO2 emissions, both in 1970 and 2010. Nevertheless, without EU emission controls, global SO2 emissions would have been 30% higher in 2010.
Emissions that have been avoided as a consequence of EU legislation have led to a reduction of annual mean European concentrations of PM2.5 by about 5 μg/m3 and of O3 by about 2.5 ppbv, and in Asia 1–2 μg/m3 and ppbv, respectively. Comparing the scenario with uncontrolled EU emissions to the reference calculations suggests that the mortality rate attributable to air pollution in the EU has been reduced by about 61,000 persons per year, which means that 18–19% have been avoided. Globally, the reduction has been about 163,000 persons per year, that is, 3–4% were avoided; in China and Japan, approximately 2% and 7% were avoided, respectively. Within the EU, relatively large reductions have been achieved in Western Europe, such as in Germany (21%), France (23%), and the Netherlands (27%).
Discussion and Conclusions
Based on recently updated data on air pollution, disease and population statistics, the excess mortality rate attributable to outdoor air pollution is estimated at 4.5 million individuals per year, associated with about 122 million years of life lost in the year 2015. This represents mortality through cardiovascular and respiratory ailments that could have been avoided when annual average PM2.5 would be below 4.2 ± 1.8 μg/m3 and O3 below 37.6 ± 4.3 ppbv. The fractional contribution of PM2.5 to mortality is about 94%, and of O3 about 6%; hence, fine particulates constitute the main health risk. Recent downward adjustment of the minimum risk exposure level for PM2.5 to ~4.2 μg/m3 (from ~7.3 μg/m3) is a main reason for the 30% higher mortality presented here for 2015 compared to previous estimates that referred to the year 2010 (Lelieveld et al., 2015; Lim et al., 2012), since a much larger fraction of the population is exposed to hazardous levels of air pollution.
In view of the revised minimum risk exposure level of ~4.2 μg/m3, air quality standards should be adjusted accordingly, currently being 12 μg/m3 in the USA and 25 μg/m3 in the EU, and higher or absent in Asian and African countries. The air quality guideline by the WHO of 10 μg/m3 for PM2.5 should also be reevaluated. While the global implementation of this WHO guideline would reduce mortality attributable to air pollution by more than 50% (Giannadaki et al., 2016), further reduction will be necessary. About 75% of the global mortality occurs in Asia, and more than 50% in China and India (together 2.4 million per year). While the latter countries lead the ranking of total mortality, the per capita mortality rate is highest in Eastern Europe (e.g., Russia) with 1.6 deaths per 1000 inhabitants annually, being more than twice that in India and four times compared to North America.
The most rapid increase in mortality attributable to air pollution worldwide occurs in South Asia, particularly in India. Although the leading source category is residential energy use, the recent increase is largely related to fossil fuel consumption, notably of coal, which doubled in the past decade (IEA, 2016). Worldwide, approximately 31% of mortality is due to residential energy use, amounting to about 1.4 million per year. This source category is also a main cause of household (indoor) air pollution-related mortality, which adds about 2.9 million per year (GBD, 2017). In South and Southeast Asia, residential energy use contributes >50% to mortality attributable to outdoor air pollution. Globally, approximately 18% (~800,000 deaths per year) is related to natural processes and is difficult to avoid, mostly due to eolian desert dust in Africa and Asia.
Pozzer et al. (2017) found that strong reductions of PM2.5 can be achieved by controlling agricultural ammonia (NH3) emissions from animal husbandry and fertilizer use. The absolute impact of NH3 on PM2.5 is largest in East Asia, even for relatively small emission decreases. In Europe and North America, the formation of PM2.5 is not directly limited by NH3, but strong emission controls could nevertheless substantially decrease PM2.5 and associated mortality, especially when the NH3 limited regime is reached at about 50% emission reduction. In other regions, including South Asia, the influence of NH3 emissions on public health is relatively minor. Based on the fractional contribution of agricultural emissions to PM2.5, it is estimated that a 50% reduction of global NH3 emissions could avoid about 350,000 deaths per year. A theoretical reduction of 100% could avoid about 900,000 deaths per year.
A study of European technology development illustrates the public health benefit achieved by emission controls (Crippa et al., 2016). An emission scenario shows the actual world avoided by EU legislation since 1970 through the EURO norms for light- and heavy-duty vehicles, and standards on fuel quality and flue gas desulfurization in the power production sector. The EU measures have influenced pollution emissions in Europe and worldwide because the EURO standards penetrated global markets. The scenario calculations suggest that mortality attributable to air pollution in the EU has decreased by about 61,000 persons per year, which means that about 18–19% mortality have been avoided. Globally, the reduction has been about 163,000 persons per year, which means 3–4% were avoided. It should be noted that these calculations do not account for illegitimate diesel-related NOx emissions. Anenberg et al. (2017) estimated that about a third of heavy-duty and more than half of light-duty diesel vehicle emissions have been in excess of certification limits, associated with about 38,000 deaths globally in 2015.
Zhang et al. (2017) investigated the relationship between exports of goods and services and the exposure to poor air quality. In effect, by exporting goods and services, countries with emerging economies in Asia and eastern Europe “import” air pollution-related mortality. These countries trade monetary revenue against health expenditures through emissions embodied in exports. It is likely that some polluting industries have been transferred internationally, such as from the EU and the USA to regions with more permissive environmental regulations. To prevent such practices, international norms and agreements are needed. It would be an important signal if the UN adopts a sustainable development goal on “clean air.” It can be argued that actions to mitigate climate change and improve air quality have co-benefits. Furthermore, clean air contributes to other sustainable development goals that aim at good health, sustainable cities, clean energy, taking climate action, and protecting life on land and in the water.
References
Akimoto, H. (2003). Global air quality and pollution. Science, 302, 1716–1719.
Anenberg, S. C., Horowitz, L. W., Tong, D. Q., & West, J. J. (2010). An estimate of the global burden of anthropogenic ozone and fine particulate matter on premature human mortality using atmospheric modeling. Environmental Health Perspectives, 118, 1189–1195.
Anenberg, S. C., Miller, J., Minjares, R., Du, L., Henze, D. K., Lacey, F., et al. (2017). Impacts and mitigation of excess diesel-related NOx emissions in 11 major vehicle markets. Nature, 445, 467–471.
Brauer, M., Freedman, G., Frostad, J., van Donkelaar, A., Martin, R. V., Dentener, F., et al. (2016). Ambient air pollution exposure estimation for the global burden of disease 2013. Environmental Science & Technology, 50, 79–88.
Burnett, R. T., Pope III, C. A., Ezzati, M., Olives, C., Lim, S. S., Mehta, S., et al. (2014). An integrated risk function for estimating the Global Burden of Disease attributable to ambient fine particulate matter exposure. Environmental Health Perspectives, 122, 397–403.
Cohen, A. J., Brauer, M., Burnett, R., Anderson, H. R., Frostad, J., Estep, K., et al. (2017). Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: An analysis of data from the Global Burden of Diseases Study 2015. The Lancet, 389, 1907–1918.
Crippa, M., Janssens-Maenhout, G., Dentener, F., Guizzardi, D., Sindelarova, K., Muntean, M., et al. (2016). Regional policy-industry interactions with global impacts. Atmospheric Chemistry and Physics, 16, 3825–3841.
Crutzen, P. J. (2002). Geology of mankind. Nature, 415, 23.
Dockery, D. W., Pope II, C. A., Xu, X., Spengler, J. D., Ware, J. H., Martha, E. F., et al. (1993). An association between air pollution and mortality in six US cities. The New England Journal of Medicine, 329, 1753–1759.
Giannadaki, D., Pozzer, A., & Lelieveld, J. (2014). Modeled global effects of airborne desert dust on air quality and premature mortality. Atmospheric Chemistry and Physics, 14, 957–968.
Giannadaki, D., Pozzer, A., & Lelieveld, J. (2016). Implementing the US air quality standard for PM2.5 worldwide can prevent millions of premature deaths per year. Environmental Health, 15, 88. https://doi.org/10.1186/s12940-016-0170-8
Global Burden of Disease (GBD)—Risk Factors Collaborators (2017). Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. The Lancet, 388, 1659–1724.
Jöckel, P., Tost, H., Pozzer, A., Brühl, C., Buchholz, J., Ganzeveld, L., et al. (2006). The atmospheric chemistry general circulation model ECHAM5/MESSy: Consistent simulation of ozone from the surface to the mesosphere. Atmospheric Chemistry and Physics, 6, 5067–5104.
Jöckel, P., Kerkweg, A., Pozzer, A., Sander, R., Tost, H., Riede, H., et al. (2010). Development cycle 2 of the Modular Earth Submodel System (MESSy2). Geoscientific Model Development, 3, 717–752.
Karydis, V. A., Tsimpidi, A. P., Bacer, S., Pozzer, A., Nenes, A., & Lelieveld, J. (2017). Global impact of mineral dust on cloud droplet number concentration. Atmospheric and Physics, 17, 5601–5621.
Karydis, V. A., Tsimpidi, A. P., Pozzer, A., Astitha, M., & Lelieveld, J. (2016). Effects of mineral dust on global atmospheric nitrate concentrations. Atmospheric Chemistry and Physics, 16, 1491–1509.
Kushta, J., Pozzer, A., & Lelieveld, J. (2018). Uncertainties in estimates of mortality attributable to ambient PM2, 5 in Europe. Environmental Research Letters, 13, 064029.
Lelieveld, J. (2017). Clean air in the Anthropocene. Faraday Discussions, 200, 693–703.
Lelieveld, J., & Dentener, F. J. (2000). What controls tropospheric ozone? Journal of Geophysical Research, 105, 3531–3551.
Lelieveld, J., Evans, J. S., Fnais, M., Giannadaki, D., & Pozzer, A. (2015). The contribution of outdoor air pollution sources to premature mortality on a global scale. Nature, 525, 367–371.
Lelieveld, J., Gromov, S., Pozzer, A., & Taraborrelli, D. (2016). Global tropospheric hydroxyl distribution, budget and reactivity. Atmospheric Chemistry and Physics, 16, 12477–12493.
Lelieveld, J., & Pöschl, U. (2017). Chemists can help to solve the air pollution health crisis. Nature, 551, 291–293.
Lim, S. S., Vos, T., Flaxman, A. D., Danaei, G., Shibuya, K., Adair-Rohani, H., et al. (2012). A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. The Lancet, 380, 2224–2260.
Pope III, C. A., Burnett, R. T., Thun, M. J., Calle, E. E., Krewski, D., Ito, K. et al. (2002). Lung cancer, cardiopulmonary mortality, and long-term exposure to fine particulate air pollution. Journal of the American Medical Association, 287, 1132–1141.
Pozzer, A., Jöckel, P., Kern, B., & Haak, H. (2011). The atmosphere-ocean general circulation model EMAC-MPIOM. Geoscientific Model Development, 4, 771–784.
Pozzer, A., Tsimpidi, A., Karydis, V., de Meij, A., & Lelieveld, J. (2017). Impact of agricultural emissions on fine particulate matter and public health. Atmospheric Chemistry and Physics, 17, 12813–12826.
Pozzer, A., de Meij, A., Pringle, K. J., Tost, H., Doering, U. M., van Aardenne, J. et al. (2012a). Distributions and regional budgets of aerosols and their precursors simulated with the EMAC chemistry-climate model. Atmospheric Chemistry and Physics, 12, 961–987.
Pozzer, A., Zimmermann, P., Doering, U. M., van Aardenne, J., Tost, H., Dentener, F. et al. (2012b). Effects of business-as-usual anthropogenic emissions on air quality. Atmospheric Chemistry and Physics, 12, 6915–6937.
Roeckner, E., Brokopf, R., Esch, M., Giorgetta, M., Hagemann, S., Kornblüh, E., et al. (2006). Sensitivity of simulated climate to horizontal and vertical resolution in the ECHAM5 atmosphere model. Journal of Climate, 19, 3771–3791.
Steffen, W., Grinevald, J., Crutzen, P., & McNeill, J. (2011). The Anthropocene: conceptual and historical perspectives. Philosophical Transactions of the Royal Society A: Mathematical, Physical and Engineering Sciences, 369, 842–867.
Tsimpidi, A. P., Karydis, V. A., Pandis, S. N., & Lelieveld, J. (2016). Global combustion sources of organic aerosols: Model comparison with 84 AMS factor analysis data sets. Atmospheric Chemistry and Physics, 16, 8939–8962.
van Donkelaar, A., Martin, R. V., Brauer, M., Kahn, R., Levy, R., Verduzco, C. et al. (2010). Global estimates of ambient fine particulate matter concentrations from satellite-based aerosol optical depth: Development and application. Environmental Health Perspectives, 118, 847–885.
Wang, X., & Mauzerall, D. L. (2006). Evaluating impacts of air pollution in China on public health: Implications for future air pollution and energy policies. Atmospheric Environment, 40, 1706–1721.
Zhang, Q., Jiang, X., Tong, D., Davis, S. J., Zhao, H., & Geng, G. (2017). Transboundary health impacts of transported global air pollution and international trade. Nature, 543, 705–709.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2020 The Author(s)
About this chapter
Cite this chapter
Lelieveld, J. (2020). Reducing Air Pollution: Avoidable Health Burden. In: Al-Delaimy, W., Ramanathan, V., Sánchez Sorondo, M. (eds) Health of People, Health of Planet and Our Responsibility. Springer, Cham. https://doi.org/10.1007/978-3-030-31125-4_9
Download citation
DOI: https://doi.org/10.1007/978-3-030-31125-4_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-31124-7
Online ISBN: 978-3-030-31125-4
eBook Packages: Earth and Environmental ScienceEarth and Environmental Science (R0)