Abstract
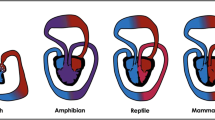
In the four-chambered human heart each cavity has its own morphological characteristics. As expected, they show also functional differences related to this morphology. It was a long nursed belief that hemodynamic changes after birth were largely responsible for these morphological and functional differences. This was clinically important as in patients with congenital heart disease, e.g. the univentricular correction (so-called Fontan procedure) was believed to lead to myocardial remodelling of the non-systemic right ventricle (RV) into a ventricle that could sustain the systemic circulation. This view proved to be too optimistic. Nowadays we know that in development (1) the RV and left ventricle (LV) derive from a temporo-spatially different source of cardiomyocytes that acquire their own specific architecture and genetic profile, (2) that the modulating epicardial contribution is different, and (3) that the coronary vascular system and microvasculature between the RV and LV differ. Based on these developmental data there is clearly a case for specific morphological, functional and remodelling capacities of the RV that set it apart from the LV.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Bleasdale RA, Frenneaux MP. Prognostic importance of right ventricular dysfunction. Heart. 2002;88:323–4.
Haddad F, Doyle R, Murphy DJ, Hunt SA. Right ventricular function in cardiovascular disease, part II: pathophysiology, clinical importance, and management of right ventricular failure. Circulation. 2008;117:1717–31.
Dore A, Houde C, Chan KL, et al. Angiotensin receptor blockade and exercise capacity in adults with systemic right ventricles: a multicenter, randomized, placebo-controlled clinical trial. Circulation. 2005;112:2411–6.
Provencher S, Herve P, Jais X, et al. Deleterious effects of beta-blockers on exercise capacity and hemodynamics in patients with portopulmonary hypertension. Gastroenterology. 2006; 130:120–6.
van der Bom T, Winter MM, Bouma BJ, et al. Effect of valsartan on systemic right ventricular function: a double-blind, randomized, placebo-controlled pilot trial. Circulation. 2013;127: 322–30.
Thum T, Borlak J. Gene expression in distinct regions of the heart. Lancet. 2000;355:979–83.
Gittenberger-de Groot AC, Sauer U, Bindl L, Babic R, Essed CE, Buhlmeyer K. Competition of coronary arteries and ventriculo-coronary arterial communications in pulmonary atresia with intact ventricular septum. Int J Cardiol. 1988;18:243–58.
Gittenberger-de Groot AC, Tennstedt C, Chaoui R, Lie-Venema H, Sauer U, Poelmann RE. Ventriculo coronary arterial communications (VCAC) and myocardial sinusoids in hearts with pulmonary artresia with intact ventricular septum: two different diseases. Prog Pediatr Cardiol. 2001;13:157–64.
Daubeney PE, Delany DJ, Anderson RH, et al. Pulmonary atresia with intact ventricular septum: range of morphology in a population-based study. J Am Coll Cardiol. 2002;39:1670–9.
Umar S, de Visser YP, Steendijk P, et al. Allogenic stem cell therapy improves right ventricular function by improving lung pathology in rats with pulmonary hypertension. Am J Physiol Heart Circ Physiol. 2009;297:H1606–16.
Castellani C, Padalino M, China P, et al. Bone-marrow-derived CXCR4-positive tissue-committed stem cell recruitment in human right ventricular remodeling. Hum Pathol. 2010;41: 1566–76.
van Mierop LH, Kutsche LM. Development of the ventricular septum of the heart. Heart Vessels. 1985;1:114–9.
Wenink ACG. Embryology of the ventricular septum. Separate origin of its components. Virchows Arch. 1981;390:71–9.
Pexieder T. Development of the outflow tract of the embryonic heart. Birth Defects. 1978;14:29–68.
Viragh S, Challice CE. Origin and differentiation of cardiac muscle cells in the mouse. J Ultrastruct Res. 1973;42:1–24.
De la Cruz MV, Gomez CS, Arteaga MM, Argüello C. Experimental study of the development of the truncus and the conus in the chick embryo. J Anat. 1977;123:661–86.
Mjaatvedt CH, Nakaoka T, Moreno-Rodriguez R, et al. The outflow tract of the heart is recruited from a novel heart-forming field. Dev Biol. 2001;238:97–109.
Waldo KL, Hutson MR, Ward CC, et al. Secondary heart field contributes myocardium and smooth muscle to the arterial pole of the developing heart. Dev Biol. 2005;281:78–90.
Cai CL, Liang X, Shi Y, et al. Isl1 identifies a cardiac progenitor population that proliferates prior to differentiation and contributes a majority of cells to the heart. Dev Cell. 2003;5: 877–89.
Abu-Issa R, Waldo K, Kirby ML. Heart fields: one, two or more? Dev Biol. 2004;272:281–5.
Meilhac SM, Esner M, Kelly RG, Nicolas JF, Buckingham ME. The clonal origin of myocardial cells in different regions of the embryonic mouse heart. Dev Cell. 2004;6:685–98.
Kelly RG. Building the right ventricle. Circ Res. 2007;100:943–5.
Bajolle F, Zaffran S, Kelly RG, et al. Rotation of the myocardial wall of the outflow tract is implicated in the normal positioning of the great arteries. Circ Res. 2006;98:421–8.
Douglas YL, Jongbloed MR, DeRuiter MC, Gittenberger-de Groot AC. Normal and abnormal development of pulmonary veins: state of the art and correlation with clinical entities. Int J Cardiol. 2010;147:13–24.
Lescroart F, Mohun T, Meilhac SM, Bennett M, Buckingham M. Lineage tree for the venous pole of the heart: clonal analysis clarifies controversial genealogy based on genetic tracing. Circ Res. 2012;111:1313–22.
Pexieder T. Cell death in the morphogenesis and teratogenesis of the heart. Adv Anat Embryol Cell Biol. 1975;51:1–99.
Bajolle F, Zaffran S, Meilhac SM, et al. Myocardium at the base of the aorta and pulmonary trunk is prefigured in the outflow tract of the heart and in subdomains of the second heart field. Dev Biol. 2008;313:25–34.
Scherptong RW, Jongbloed MR, Wisse LJ, et al. Morphogenesis of outflow tract rotation during cardiac development: the pulmonary push concept. Dev Dyn. 2012;241:1413–22.
Kruithof BP, Kruithof-de Julio M, Poelmann RE, Gittenberger-de-Groot AC, Gaussin V, Goumans MJ. Early myocardial trabeculation and differential remodeling of the left and right atrioventricular myocardium; implications for cardiac valve formation and a role for TGFbeta2. Int J Dev Biol. 2013; in press.
Sedmera D, Pexieder T, Rychterova V, Hu N, Clark EB. Remodeling of chick embryonic ventricular myoarchitecture under experimentally changed loading conditions. Anat Rec. 1999;254:238–52.
Wenink ACG, Gittenberger-de Groot AC. Left and right ventricular trabecular patterns. Consequence of ventricular septation and valve development. Br Heart J. 1982;48:462–8.
Gittenberger-de Groot AC, Winter EM, Bartelings MM, Goumans MJ, DeRuiter MC, Poelmann RE. The arterial and cardiac epicardium in development, disease and repair. Differentiation. 2012;84:41–53.
Vrancken Peeters M-PFM, Mentink MMT, Poelmann RE, Gittenberger-de Groot AC. Cytokeratins as a marker for epicardial formation in the quail embryo. Anat Embryol. 1995;191:503–8.
Perez-Pomares JM, Pompa JL. Signaling during epicardium and coronary vessel development. Circ Res. 2011;109:1429–42.
Limana F, Capogrossi MC, Germani A. The epicardium in cardiac repair: from the stem cell view. Pharmacol Ther. 2011;129:82–96.
Smart N, Dube KN, Riley PR. Epicardial progenitor cells in cardiac regeneration and neovascularisation. Vascul Pharmacol. 2013;58:164–73.
Bax NA, Van Oorschot AA, Maas S, et al. In vitro epithelial-to-mesenchymal transformation in human adult epicardial cells is regulated by TGFbeta-signaling and WT1. Basic Res Cardiol. 2011;106:829–47.
Acharya A, Baek ST, Huang G, et al. The bHLH transcription factor Tcf21 is required for lineage-specific EMT of cardiac fibroblast progenitors. Development. 2012;139:2139–49.
Gittenberger-de Groot AC, Vrancken Peeters MP, Bergwerff M, Mentink MM, Poelmann RE. Epicardial outgrowth inhibition leads to compensatory mesothelial outflow tract collar and abnormal cardiac septation and coronary formation. Circ Res. 2000;87:969–71.
Bogers AJJC, Gittenberger-de Groot AC, Poelmann RE, Péault BM, Huysmans HA. Development of the origin of the coronary arteries, a matter of ingrowth or outgrowth? Anat Embryol. 1989;180:437–41.
Eralp I, Lie-Venema H, DeRuiter MC, et al. Coronary artery and orifice development is associated with proper timing of epicardial outgrowth and correlated Fas ligand associated apoptosis patterns. Circ Res. 2005;96:526–34.
Tian X, Hu T, He L, et al. Peritruncal coronary endothelial cells contribute to proximal coronary artery stems and their aortic orifices in the mouse heart. PLoS One. 2013;8:e80857.
Lie-Venema H, Gittenberger-de Groot AC, van Empel LJP, et al. Ets-1 and Ets-2 transcription factors are essential for normal coronary and myocardial development in chicken embryos. Circ Res. 2003;92:749–56.
Sauer U, Gittenberger-de Groot AC, Geishauser M, Babic R, Buhlmeyer K. Coronary arteries in the hypoplastic left heart syndrome. Circulation. 1989;80:168–76.
Oosthoek PW, Moorman AFM, Sauer U, Gittenberger-de Groot AC. Capillary distribution in the ventricles of hearts with pulmonary atresia and intact ventricular septum. Circulation. 1995;91:1790–7.
Sauer U, Bindl L, Pilossoff V, et al. Pulmonary atresia with intact ventricular septum and right ventricle coronary artery fistulae: selection of patients for surgery. In: Doyle EF, Engler ME, Gersony WM, Rashlund WJ, Talmer NS, editors. Pediatric cardiology. New York: Springer; 1986. p. 566–78.
Hokken RB, Bartelings MM, Bogers AJJC, Gittenberger-de Groot AC. Morphology of the pulmonary and aortic roots with regard to the pulmonary autograft procedure. J Thorac Cardiovasc Surg. 1997;113:453–61.
Bartelings MM, Gittenberger-de Groot AC. The arterial orifice level in the early human embryo. Anat Embryol. 1988;177:537–42.
Lalezari S, Hazekamp MG, Bartelings MM, Schoof PH, Gittenberger-de Groot AC. Pulmonary artery remodeling in transposition of the great arteries: relevance for neoaortic root dilatation. J Thorac Cardiovasc Surg. 2003;126:1053–60.
Torrent-Guasp F, Kocica MJ, Corno AF, et al. Towards new understanding of the heart structure and function. Eur J Cardiothorac Surg. 2005;27:191–201.
Meilhac SM, Esner M, Kerszberg M, Moss JE, Buckingham ME. Oriented clonal cell growth in the developing mouse myocardium underlies cardiac morphogenesis. J Cell Biol. 2004;164: 97–109.
Poelmann RE, Mikawa T, Gittenberger-de Groot AC. Neural crest cells in outflow tract septation of the embryonic chicken heart: differentiation and apoptosis. Dev Dyn. 1998;212:373–84.
van den Hoff MJ, Moorman AF, Ruijter JM, et al. Myocardialization of the cardiac outflow tract. Dev Biol. 1999;212:477–90.
Waldo K, Miyagawa-Tomita S, Kumiski D, Kirby ML. Cardiac neural crest cells provide new insight into septation of the cardiac outflow tract: aortic sac to ventricular septal closure. Dev Biol. 1998;196:129–44.
Kirby ML, Gale TF, Stewart DE. Neural crest cells contribute to normal aorticopulmonary septation. Science. 1983;220:1059–61.
Gittenberger-de Groot AC, Bartelings MM, DeRuiter MC, Poelmann RE. Basics of cardiac development for the understanding of congenital heart malformations. Pediatr Res. 2005;57: 169–76.
Wenink ACG, Oppenheimer-Dekker A, Moulaert AJ. Muscular ventricular septal defects: a reappraisal of the anatomy. Am J Cardiol. 1979;43:259–64.
Lamers WH, Wessels A, Verbeek FJ, et al. New findings concerning ventricular septation in the human heart. Implications for maldevelopment. Circulation. 1992;86:1194–205.
Moorman AFM, Christoffels VM. Cardiac chamber formation: development, genes and evolution. Physiol Rev. 2003;83:1223–67.
Voelkel NF, Natarajan R, Drake JI, Bogaard HJ. Right ventricle in pulmonary hypertension. Compr Physiol. 2011;1:525–40.
Bogaard HJ, Natarajan R, Mizuno S, et al. Adrenergic receptor blockade reverses right heart remodeling and dysfunction in pulmonary hypertensive rats. Am J Respir Crit Care Med. 2010;182:652–60.
Borgdorff MA, Bartelds B, Dickinson MG, Steendijk P, Berger RM. A cornerstone of heart failure treatment is not effective in experimental right ventricular failure. Int J Cardiol. 2013;169:183–9.
Winter EM, Grauss RW, Hogers B, et al. Preservation of left ventricular function and attenuation of remodeling after transplantation of human epicardium-derived cells into the infarcted mouse heart. Circulation. 2007;116:917–27.
Winter EM, Van Oorschot AA, Hogers B, et al. A new direction for cardiac regeneration therapy: application of synergistically acting epicardium-derived cells and cardiomyocyte progenitor cells. Circ Heart Fail. 2009;2:643–53.
Zhou B, Pu WT. Epicardial epithelial-to-mesenchymal transition in injured heart. J Cell Mol Med. 2011;15:2781–3.
Gittenberger-de-Groot AC, Winter EM, Poelmann RE. Epicardium-derived cells (EPDCs) in development, cardiac disease and repair of ischemia. J Cell Mol Med. 2010;14:1056–60.
Smart N, Riley PR. The epicardium as a candidate for heart regeneration. Future Cardiol. 2012;8:53–69.
Jongbloed MR, Vicente SR, Hahurij ND, et al. Normal and abnormal development of the cardiac conduction system; implications for conduction and rhythm disorders in the child and adult. Differentiation. 2012;84:131–48.
Acknowledgements
The authors gratefully thank Ron Slagter, Bert Wisse en Judith den Boeft for their help in preparing the figures.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Video 1.1
Animated three-dimensional reconstruction demonstrating the asymmetric contribution of Nkx2.5 expressing cells (bright yellow) within the heart and anterior heart field at embryonic day (ED) 12.5. This column is rendered transparent during part of the animation to demonstrate its relation to the aorta (red) and pulmonary trunk (dark blue). The outflow tract and right ventricle are depicted in light-yellow, and the left ventricle is depicted in grey. Additional colour coding: Light blue: endocardial cushion tissue. Movie published in [28], and reproduced with permission. (AVI 33624 kb)
Rights and permissions
Copyright information
© 2015 Springer Science+Business Media New York
About this chapter
Cite this chapter
Groot, A.L.Gd., Poelmann, R.E., Vicente-Steijn, R., Bartelings, M.M., Bogaard, H.J., Jongbloed, M.R.M. (2015). Normal Development and Morphology of the Right Ventricle: Clinical Relevance. In: Voelkel, N., Schranz, D. (eds) The Right Ventricle in Health and Disease. Respiratory Medicine. Humana Press, New York, NY. https://doi.org/10.1007/978-1-4939-1065-6_1
Download citation
DOI: https://doi.org/10.1007/978-1-4939-1065-6_1
Published:
Publisher Name: Humana Press, New York, NY
Print ISBN: 978-1-4939-1064-9
Online ISBN: 978-1-4939-1065-6
eBook Packages: MedicineMedicine (R0)