Abstract
MD is a 32-year-old woman who presented with pain behind her left eye and loss of central vision. The pain worsened on looking horizontally in either direction. Examination revealed visual acuity in that eye of 20/200, a positive afferent pupil defect, and a normal-appearing optic disc. The presumed diagnosis of retrobulbar neuritis was made based on the clinical setting.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
MD is a 32-year-old woman who presented with pain behind her left eye and loss of central vision. The pain worsened on looking horizontally in either direction. Examination revealed visual acuity in that eye of 20/200, a positive afferent pupil defect, and a normal-appearing optic disc. The presumed diagnosis of retrobulbar neuritis was made based on the clinical setting.
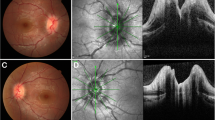
Echography was performed, and A-scan measured the right optic nerve to be 3.2 mm in greatest diameter and the left nerve 3.88 mm (Fig. 1). The 30° test was negative with a nonsignificant reduction to 3.74 mm on abduction of the left eye. B-scan showed mild echolucency of subtenon’s space posterior to the left globe. These findings were consistent with optic nerve edema secondary to retrobulbar neuritis.
Most cases of optic neuritis are the result of demyelinating disease, but there are rarely other causes such as sarcoidosis. These patients usually present with a chronic course with fluctuating vision and low-grade pain over time. They may have other areas of ocular inflammation such as iritis, panuveitis, vitritis, and retinal vasculitis.
Author information
Authors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media New York
About this chapter
Cite this chapter
Harrie, R.P., Kendall, C.J. (2014). Case Study 55 Retrobulbar Neuritis. In: Clinical Ophthalmic Echography. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-7082-3_55
Download citation
DOI: https://doi.org/10.1007/978-1-4614-7082-3_55
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-7081-6
Online ISBN: 978-1-4614-7082-3
eBook Packages: MedicineMedicine (R0)