Key summary points
To assess the prevalence of inappropriate prescriptions of antithrombotic therapies (AT) in older outpatients, and to examine the associated factors.
AbstractSection Findings22.6% patients featured ≥ 1 in AT-STOPP criteria, 12.4% ≥ 1 in AT-START criteria. The most frequent AT-STOPP criterion was AT prescription despite a concurrent significant bleeding risk. The most frequent AT-START criterion was lack of AT prescription for patients with chronic atrial fibrillation. Two factors were associated with ≥ 1 AT-STOPP criteria: polymedication and previous hospitalization for a serious adverse drug event. The only factor associated with ≥ 1 AT-START criteria was lack of information in the prescription regarding the duration of treatment.
AbstractSection MessageSuboptimal prescribing of AT is common in GP’s prescriptions for older autonomous outpatients. Special attention should be given to those with polymedication and a history of severe adverse drug event.
Abstract
Purpose
To assess the prevalence of inappropriate prescriptions of antithrombotic therapies (AT) in older outpatients and examine the associated factors.
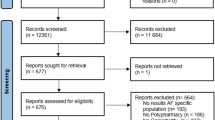
Methods
A multicenter cross-sectional study was performed in 75 community pharmacies of 11 French districts. The study included 1178 patients aged ≥ 75 years filling a prescription from a general practitioner (GP) at a community pharmacy (mean [SD] age 83 [± 5.5] years, 59% female, median prescribed drugs 7 [range 5–10]).75 pharmacy students prospectively collected data from structured interviews with patients and from prescriptions into an electronic case report. Updated 2014 STOPP/START criteria regarding AT were applied to each prescription. Factors associated with ≥ 1 AT-STOPP criteria and ≥ 1 AT-START criteria were studied (multivariate analysis).
Results
22.6% patients featured ≥ 1 in AT-STOPP criteria and 12.4% ≥ 1 in AT-START criteria. The most frequent AT-STOPP and AT-START criteria were AT prescription despite a concurrent significant bleeding risk and lack of AT prescription for patients with chronic atrial fibrillation, respectively. Two factors were associated with ≥ 1 AT-STOPP criteria: polymedication (≥ 5 drugs; p < 0.001) and previous hospitalization for a serious adverse drug event (ADE; p = 0.007). The only factor associated with ≥ 1 AT-START criteria was lack of information in the prescription regarding the duration of treatment.
Conclusion
Suboptimal prescribing of AT is common in GP’s prescriptions for older autonomous outpatients. The currently process of prescribing AT to older autonomous patients must be improved. Special attention should be given to those with polymedication and those with a history of severe ADEs.
Similar content being viewed by others
References
Gurwitz JH, Field TS, Harrold LR et al (2003) Incidence and preventability of adverse drug events among older persons in the ambulatory setting. JAMA 289:1107–1116
Kongkaew C, Hann M, Mandal J et al (2013) Risk factors for hospital admissions associated with adverse drug events. Pharmacotherapy 33(8):827–837
Shehab N, Lovegrove MC, Geller A et al (2016) US emergency department visits for outpatient adverse drug events, 2013–2014. JAMA 316(20):2115–2125
Eckman MH, Lip GY, Wise RE et al (2016) Using an atrial fibrillation decision support tool for thromboprophylaxis in atrial fibrillation: effect of sex and age. J Am Geriatr Soc 64(5):1054–1060
Chau SH, Jansen AP, van de Ven PM et al (2016) Clinical medication reviews in elderly patients with polypharmacy: across-sectional study on drug-related problems in the Netherlands. Int J Clin Pharm 38(1):46–53
Wester K, Jönsson AK, Spigset O et al (2008) Incidence of fatal adverse drug reactions. Br J Clin Pharmacol 65(4):573–579
O’Mahony D, O’Sullivan D, Byrne S et al (2014) Stopp & Start criteria for potentially inappropriate prescribing in older people: version 2. Age Ageing 44(2):213–218. https://doi.org/10.1093/ageing/afu145
O’Mahony D, Gallagher P, Ryan C et al (2010) Stopp&Start criteria: a new approach to detecting potentially inappropriate prescribing in old age. Eur Geriatr Med 1:45–51
Gallagher P, Ryan C, Byrne S et al (2008) STOPP and START: consensus validation. Int J Clin Pharm Ther 46:72–83
Barry PJ, Gallagher P, Ryan C et al (2007) Start: an evidence-based screening tool to detect prescribing omissions in elderly patients. Age Ageing 36:632–638
Levy HB, Marcus EL, Christen C (2010) Beyond the beers criteria: a comparative overview of explicit criteria. Ann Pharmacother 44(12):1968–1975
Page RL, Linnebur SA, Bryant LL et al (2010) Prescribing in the hospitalized elderly patients: defining the problem, evaluation tools, possible solutions. Clin Interv Aging 5:75–87
Hamilton H, Gallagher P, Ryan C et al (2011) Potentially inappropriate medications defined by STOPP criteria and the risk of adverse drug events in older hospitalized patients. Arch Intern Med 171(11):1013–1019
Steinman MA, Hanlon JA, Sloane RJ et al (2011) Do geriatric conditions increase risk of adverse drug reactions in ambulatory elders? Results from the VAGEM drug study. J Gerontol A Biol Sci Med Sci. 66(4):444–451
Getachew H, Bhagavathula AS, Abebe TB et al (2016) Inappropriate prescribing in anti-thrombotic therapy in Ethiopian elderly population using updated 2015 STOPP/START criteria: a cross-sectional study. Clin Interv Aging 11:819–827
Tommelein E, Mehuys E, Boussery K et al (2015) Potentially inappropriate prescribing in community-dwelling older people across Europe: a systematic literature review. Eur J Clin Pharmacol 71(12):1415–1427. https://doi.org/10.1007/s00228-015-1954-4
R Development Core Team (2008) R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. ISBN 3-900051-07-0. http://www.R-project.org
Ryan C, O’Mahony D, Kennedy J et al (2009) Potentially inappropriate prescribing in an Irish elderly population in primary care. Br J Clin Pharmacol 68:936–947
Vezmar Kovačević S, Simišić M, Stojkov Rudinski S et al (2014) Potentially inappropriate prescribing in older primary care patients. PLoS One 9(4):e95536
Filomena Paci J, García Alfaro M, Redondo Alonso FJ et al (2015) Inapropriate prescribing in polymedicated patients over 64 years old in primary care. Aten Primaria 47(1):38–47
Oliveira MG, Amorim WW, de Jesus SR et al (2015) A comparison of the Beers and STOPP criteria for identifying the use of potentially inappropriate medications among elderly patients in primary care. J Eval Clin Pract 21:320–325
Projovic I, Vukadinovic D, Milovanovic O et al (2016) Risk factors for potentially inappropriate prescribing to older patients in primary care. Eur J Clin Pharmacol 72(1):93–107
Ryan C, O’Mahony D, O’Donovan DÓ et al (2013) A comparison of the application of StoppStart to patients drugs lists with and without clinical information. Int J Clin Pharm 35:230–235
Bushardt RL, Massey EB, Simpson TW et al (2008) Polypharmacy: misleading, but manageable. Clin Interv Ageing 3(2):383–389
Beuscart JB, Dupont C, Defebvre MM et al (2014) Potentially inappropriate medications (PIMs) and anticholinergic levels in the elderly: a population-based study in a French region. Arch Gerontol Geriatr 59(3):630–635
Rapport IRDES. La polymédication au regard de différents indicateurs de sa mesure: impact sur la prévalence, les classes thérapeutiques concernées et les facteurs associés. Octobre 2015. Available in an English short version at: http://www.irdes.fr/english/issues-in-health-economics/204-polypharmacy-definitions-measurement-and-stakes-involved.pdf
Blanco-Reina E, García-Merino MR, Ocaña-Riola R et al (2016) Assessing potentially inappropriate prescribing in community-dwelling older patients using the updated version of STOPP-START criteria: a comparison of profiles and prevalences with respect to the original version. PLoS One 11(12):e0167586
O’Riordan D, Aubert CE, Walsh KA et al (2018) Prevalence of potentially inappropriate prescribing in a subpopulation of older European clinical trial participants: a cross-sectional study. BMJ Open 8(3):e019003
Jouin G, Paya D, Michel B et al (2014) Ré-évaluation thérapeutique des personnes âgées à l’occasion d’une hospitalisation: étude prospective auprès de 97 patients. Rev Med Int 35:77–78
Hernández Perella JA, Mas Garriga X, Riera Cervera D et al (2013) Inappropriate prescribing of drugs in older people attending primary care health centers: detection using STOPP-START criteria. Rev Esp Geriatr Gerontol 48(6):265–268
Budnitz DS, Lovegrove MC, Shehab N et al (2011) Emergency hospitalizations for adverse drug events in older Americans. New Engl J Med 365:2002–2012
Milos V, Rekman E, Bondesson A et al (2013) Imporving the quality of pharmacotherapy in elderly primary care patients through medication reviews: a randomized controlled study. Drugs Aging 30:235–246
Hanlon JT, Weinberger M, Samsa GP et al (1996) A randomized, controlled trial of a clinical pharmacist intervention to improve inappropriate prescribing in elderly outpatients with polypharmacy. Am J Med 100:430–437
Hanlon JT, Schmader KE, Ruby CM (2001) Suboptimal prescribing in older inpatients and outpatients. JAGS 49:200–209
Acknowledgements
We are indebted to the 6th-year pharmacy students from Paris-Sud University for their outstanding efforts in collecting data.
Author information
Authors and Affiliations
Contributions
Dubois-Puechlong, Tubach and Bonnet-Zamponi had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Dubois-Puechlong, Fernandez, Hindlet, Tubach, Bonnet-Zamponi: study concept and design. Dubois-Puechlong, Mille: acquisition of data. Dubois-Puechlong, Mille, Hindlet, de Rycke, Fernandez, Tubach, Bonnet-Zamponi: analysis and interpretation of data. Dubois-Puechlong, Bonnet-Zamponi: drafting of the manuscript. All authors: critical revision of the manuscript for important intellectual content. Mille, De Rycke: statistical analysis. Hindlet, Fernandez, Tubach, Bonnet-Zamponi: study supervision. All authors have seen and approved the final version of the submission.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no financial or any other kind of personal conflicts with this paper.
Ethical approval
The university ethics committee approved the study protocol (no. NI-2016-03-03) and all procedures performed in studies involving human participants were in accordance with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dubois-Puechlong, S., Mille, F., Hindlet, P. et al. Potentially inappropriate prescriptions of antithrombotic therapies in older outpatients: a French multicenter cross-sectional study. Eur Geriatr Med 10, 473–481 (2019). https://doi.org/10.1007/s41999-019-00176-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41999-019-00176-2