Abstract
Purpose of Review
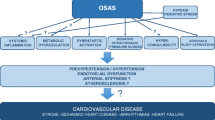
In this paper, we analyzed the principal mechanisms linking OSA and cardiovascular diseases, the magnitude of this association, and the effect of treatment on cardiovascular risk reduction. Furthermore, we focused on big data and genomic approaches that may expand the innovative horizon aimed at personalized treatment of OSA.
Recent Findings
Patients with obstructive sleep apnea (OSA) are more prone to suffer from cardiovascular diseases and their complications. Arousal from sleep, changes in intrathoracic pressures, and intermittent episodes of hypoxemia and re-oxygenation trigger intermediate mechanisms that are responsible for the cardiovascular consequences of OSA.
Summary
The impact of OSA on cardiovascular health, such as the effect of continuous positive airway pressure (CPAP) treatment on cardiovascular risk, may vary among different patient profiles. In spite of increasing interest towards personalized therapy for OSA, observational studies and randomized clinical trials have failed to conclusively determine which OSA phenotypes may benefit most from treatment, particularly in terms of reducing cardiovascular risk.



Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
WHO | Cardiovascular diseases (CVDs). WHO. World Health Organization; 2017.
Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013;177(9):1006–14. https://doi.org/10.1093/aje/kws342.
Javaheri S, Barbe F, Campos-Rodriguez F, Dempsey JA, Khayat R, Javaheri S, et al. Sleep apnea. J Am Coll Cardiol. 2017;69(7):841–58. https://doi.org/10.1016/j.jacc.2016.11.069.
•• Peppard PE, Young T, Palta M, Skatrud J. Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med. 2000;342:1378–84. In this paper, a dose response relation between sleep apnea and the presence of hypertension has been observed in the Winsconsin Sleep Cohort. Thus, for the first time, OSA has been suggested as a risk factor for developing hypertension and other cardiovascular diseases.
•• Hla KM, Young T, Finn L, Peppard PE, Szklo-Coxe M, Stubbs M. Longitudinal association of sleep-disordered breathing and nondipping of nocturnal blood pressure in the Wisconsin Sleep Cohort Study. Sleep. 2008;31:795–800. Observing the same Winsconsin cohort, the researchers found a dose-response increase in development of systolic nondipping of blood pressure depending on the severity of sleep disordered breathing at baseline. This study proposed the “nocturnal systolic nondipping” as a mechanism by which sleep disordered breathing contributes to increase cardiovascular disease risk.
Mokhlesi B, Finn LA, Hagen EW, Young T, Hla KM, Van Cauter E, et al. Obstructive sleep apnea during REM sleep and hypertension. Results of the Wisconsin sleep cohort. Am J Respir Crit Care Med Am Thoracic Soc. 2014;190(10):1158–67. https://doi.org/10.1164/rccm.201406-1136OC.
O’Connor GT, Caffo B, Newman AB, Quan SF, Rapoport DM, Redline S, et al. Prospective study of sleep-disordered breathing and hypertension. Am J Respir Crit Care Med. 2009;179(12):1159–64. https://doi.org/10.1164/rccm.200712-1809OC.
•• Cano-Pumarega I, Durán-Cantolla J, Aizpuru F, Miranda-Serrano E, Rubio R, Martínez-Null C, et al. Obstructive sleep apnea and systemic hypertension. Am J Respir Crit Care Med. 2011;184:1299–304. In contrast with previous findings, in this article, the authors do not observe an association between obstructive sleep apnea and the incidence of systemic hypertension in the middle-aged general population.
Cano-Pumarega I, Barbé F, Esteban A, Martínez-Alonso M, Egea C, Durán-Cantolla J, et al. Sleep apnea and hypertension. Chest. 2017;152(4):742–50. https://doi.org/10.1016/j.chest.2017.03.008.
Logan AG, Perlikowski SM, Mente A, Tisler A, Tkacova R, Niroumand M, et al. High prevalence of unrecognized sleep apnoea in drug-resistant hypertension. J Hypertens. 2001;19(12):2271–7. https://doi.org/10.1097/00004872-200112000-00022.
Weber MA, Schiffrin EL, White WB, Mann S, Lindholm LH, Kenerson JG, et al. Clinical practice guidelines for the management of hypertension in the community. A statement by the American Society of Hypertension and the International Society of Hypertension. J Hypertens. 2014;32(1):3–15. https://doi.org/10.1097/HJH.0000000000000065.
Johnson KG, Johnson DC. Frequency of sleep apnea in stroke and TIA patients: a meta-analysis. J Clin Sleep Med Am Acad Sleep Med. 2010;6:131–7.
Li M, Hou W-S, Zhang X-W, Tang Z-Y. Obstructive sleep apnea and risk of stroke: a meta-analysis of prospective studies. Int J Cardiol. 2014;172(2):466–9. https://doi.org/10.1016/j.ijcard.2013.12.230.
Kernan WN, Ovbiagele B, Black HR, Bravata DM, Chimowitz MI, Ezekowitz MD, et al. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45(7):2160–236. https://doi.org/10.1161/STR.0000000000000024.
Mehra R, Benjamin EJ, Shahar E, Gottlieb DJ, Nawabit R, Kirchner HL, et al. Association of nocturnal arrhythmias with sleep-disordered breathing. Am J Respir Crit Care Med. 2006;173(8):910–6. https://doi.org/10.1164/rccm.200509-1442OC.
Kanagala R, Murali NS, Friedman PA, Ammash NM, Gersh BJ, Ballman KV, et al. Obstructive sleep apnea and the recurrence of atrial fibrillation. Circulation. 2003;107(20):2589–94. https://doi.org/10.1161/01.CIR.0000068337.25994.21.
•• Gottlieb DJ, Yenokyan G, Newman AB, O’Connor GT, Punjabi NM, Quan SF, et al. Prospective study of obstructive sleep apnea and incident coronary heart disease and heart failure: the sleep heart health study. Circulation. 2010;122:352–60. In this prospective study, the authors found a significant association between obstructive sleep apnea and an increased risk of incident heart failure in middle-aged and older men.
Hla KM, Young T, Hagen EW, Stein JH, Finn LA, Nieto FJ, et al. Coronary heart disease incidence in sleep disordered breathing: the Wisconsin sleep cohort study. Sleep. 2015;38(5):677–84. https://doi.org/10.5665/sleep.4654.
Loke YK, Brown JWL, Kwok CS, Niruban A, Myint PK. Association of obstructive sleep apnea with risk of serious cardiovascular events: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2012;5(5):720–8. https://doi.org/10.1161/CIRCOUTCOMES.111.964783.
•• Gami AS, Olson EJ, Shen WK, Wright RS, Ballman KV, Hodge DO, et al. Obstructive sleep apnea and the risk of sudden cardiac death: a longitudinal study of 10,701 adults. J Am Coll Cardiol. 2013;62:610–6. NIH Public Access. In this study, the authors reported that people with OSA have a peak in sudden death from cardiac causes during the sleeping hours, which contrasts strikingly with the nadir of sudden death from cardiac causes during this period in people without OSA and in the general population.
Martins EF, Martinez D, da Silva FABS, Sezerá L, da RosadeCamargo R, Fiori CZ, et al. Disrupted day–night pattern of cardiovascular death in obstructive sleep apnea. Sleep Med. 2017;38:144–50. https://doi.org/10.1016/j.sleep.2017.06.027.
Lyons OD, Bradley TD. Heart failure and sleep apnea. Can J Cardiol. 2015;31(7):898–908. https://doi.org/10.1016/j.cjca.2015.04.017.
Redline S, Yenokyan G, Gottlieb DJ, Shahar E, O’Connor GT, Resnick HE, et al. Obstructive sleep apnea–hypopnea and incident stroke. Am J Respir Crit Care Med. 2010;182(2):269–77. https://doi.org/10.1164/rccm.200911-1746OC.
Campos-Rodriguez F, Martinez-Garcia MA, de la Cruz-Moron I, Almeida-Gonzalez C, Catalan-Serra P, Montserrat JM. Cardiovascular mortality in women with obstructive sleep apnea with or without continuous positive airway pressure treatment. Ann Intern Med. 2012;156(2):115–22. https://doi.org/10.7326/0003-4819-156-2-201201170-00006.
Martínez-García M-A, Campos-Rodríguez F, Catalán-Serra P, Soler-Cataluña J-J, Almeida-Gonzalez C, De la Cruz Morón I, et al. Cardiovascular mortality in obstructive sleep apnea in the elderly: role of long-term continuous positive airway pressure treatment. Am J Respir Crit Care Med. 2012;186(9):909–16. https://doi.org/10.1164/rccm.201203-0448OC.
Javaheri S, Blackwell T, Ancoli-Israel S, Ensrud KE, Stone KL, Redline S, et al. Sleep-disordered breathing and incident heart failure in older men. Am J Respir Crit Care Med Am Thoracic Soc. 2016;193(5):561–8. https://doi.org/10.1164/rccm.201503-0536OC.
Koo C-Y, de la Torre AS, Loo G, Torre MS, Zhang J, Duran-Cantolla J, et al. Effects of ethnicity on the prevalence of obstructive sleep apnoea in patients with acute coronary syndrome: a pooled analysis of the ISAACC trial and sleep and stent study. Hear Lung Circ. 2017;26(5):486–94. https://doi.org/10.1016/j.hlc.2016.09.010.
Fülöp T, Hickson DA, Wyatt SB, Bhagat R, Rack M, Gowdy O, et al. Sleep-disordered breathing symptoms among African-Americans in the Jackson heart study. Sleep Med. 2012;13(8):1039–49. https://doi.org/10.1016/j.sleep.2012.06.005.
Olafiranye O, Akinboboye O, Mitchell JE, Ogedegbe G, Jean-Louis G. Obstructive sleep apnea and cardiovascular disease in blacks: a call to action from the Association of Black Cardiologists. Am Heart J. 2013;165(4):468–76. https://doi.org/10.1016/j.ahj.2012.12.018.
MESA - Multi-Ethnic Study of Atherosclerosis [Internet]. [cited 2017 Nov 24]. Available from: https://www.mesa-nhlbi.org/default.aspx.
Budhiraja R, Thomas R, Kim M, Redline S. The role of big data in the management of sleep-disordered breathing. Sleep Med Clin. 2016;11(2):241–55. https://doi.org/10.1016/j.jsmc.2016.01.009.
Turino C, Bertran S, Gavaldá R, Teixidó I, Woehrle H, Rué M, et al. Characterization of the CPAP-treated patient population in Catalonia. Heiser C, editor. PLoS One Public Libr Sci. 2017;12:e0185191.
Castro-Grattoni AL, Alvarez-Buvé R, Torres M, Farré R, Montserrat JM, Dalmases M, et al. Intermittent hypoxia-induced cardiovascular remodeling is reversed by normoxia in a mouse model of sleep apnea. Chest. 2016;149(6):1400–8. https://doi.org/10.1016/j.chest.2015.11.010.
Cortese R, Gileles-Hillel A, Khalyfa A, Almendros I, Akbarpour M, Khalyfa AA, et al. Aorta macrophage inflammatory and epigenetic changes in a murine model of obstructive sleep apnea: potential role of CD36. Sci Rep. 2017;7:43648. https://doi.org/10.1038/srep43648.
Martínez-García M-A, Capote F, Campos-Rodríguez F, Lloberes P, Díaz de Atauri MJ, Somoza M, et al. Effect of CPAP on blood pressure in patients with obstructive sleep apnea and resistant hypertension. JAMA. 2013;310(22):2407–15. https://doi.org/10.1001/jama.2013.281250.
Sánchez-de-la-Torre M, Campos-Rodriguez F, Barbé F. Obstructive sleep apnoea and cardiovascular disease. Lancet Respir Med. 2013;1(1):61–72. https://doi.org/10.1016/S2213-2600(12)70051-6.
Kohler M, Stradling JR. Mechanisms of vascular damage in obstructive sleep apnea. Nat Rev Cardiol. 2010;7(12):677–85. https://doi.org/10.1038/nrcardio.2010.145.
Lavie L. Obstructive sleep apnoea syndrome—an oxidative stress disorder. Sleep Med Rev. 2003;7(1):35–51. https://doi.org/10.1053/smrv.2002.0261.
Somers VK, Dyken ME, Clary MP, Abboud FM. Sympathetic neural mechanisms in obstructive sleep apnea. J Clin Invest. 1995;96(4):1897–904. https://doi.org/10.1172/JCI118235.
Budhiraja R, Parthasarathy S, Quan SF. Endothelial dysfunction in obstructive sleep apnea. J Clin Sleep Med. 2007;3:409–15.
Rubinstein I. Nasal inflammation in patients with obstructive sleep apnea. Laryngoscope. 1995;105(2):175–7. https://doi.org/10.1288/00005537-199502000-00012.
Yamauchi M, Tamaki S, Tomoda K, Yoshikawa M, Fukuoka A, Makinodan K, et al. Evidence for activation of nuclear factor kappaB in obstructive sleep apnea. Sleep Breath. 2006;10(4):189–93. https://doi.org/10.1007/s11325-006-0074-x.
Rångemark C, Hedner JA, Carlson JT, Gleerup G, Winther K. Platelet function and fibrinolytic activity in hypertensive and normotensive sleep apnea patients. Sleep. 1995;18(3):188–94. https://doi.org/10.1093/sleep/18.3.188.
von Känel R, Dimsdale JE. Hemostatic alterations in patients with obstructive sleep apnea and the implications for cardiovascular disease. Chest. 2003;124(5):1956–67. https://doi.org/10.1378/chest.124.5.1956.
Bonsignore MR, Esquinas C, Barceló A, Sanchez-de-la-Torre M, Paternó A, Duran-Cantolla J, et al. Metabolic syndrome, insulin resistance and sleepiness in real-life obstructive sleep apnoea. Eur Respir J. 2012;39(5):1136–43. https://doi.org/10.1183/09031936.00151110.
Barcelo A, Pierola J, de la Pena M, Esquinas C, Fuster A, Sanchez-de-la-Torre M, et al. Free fatty acids and the metabolic syndrome in patients with obstructive sleep apnoea. Eur Respir J. 2011;37(6):1418–23. https://doi.org/10.1183/09031936.00050410.
Lacedonia D, Carpagnano GE, Sabato R, Lo SMM, Palmiotti GA, Capozzi V, et al. Characterization of obstructive sleep apnea-hypopnea syndrome (OSA) population by means of cluster analysis. J Sleep Res. 2016;25(6):724–30. https://doi.org/10.1111/jsr.12429.
Ye L, Pien GW, Ratcliffe SJ, Björnsdottir E, Arnardottir ES, Pack AI, et al. The different clinical faces of obstructive sleep apnoea: a cluster analysis. Eur Respir J. 2014;44(6):1600–7. https://doi.org/10.1183/09031936.00032314.
Zinchuk AV, Jeon S, Koo BB, Yan X, Bravata DM, Qin L, et al. Polysomnographic phenotypes and their cardiovascular implications in obstructive sleep apnoea. Thorax. 2017:thoraxjnl-2017-210431. https://doi.org/10.1136/thoraxjnl-2017-210431.
Marin JM, Agusti A, Villar I, Forner M, Nieto D, Carrizo SJ, et al. Association between treated and untreated obstructive sleep apnea and risk of hypertension. JAMA. 2012;307(20):2169–76. https://doi.org/10.1001/jama.2012.3418.
Gonçalves SC, Martinez D, Gus M, de Abreu-Silva EO, Bertoluci C, Dutra I, et al. Obstructive sleep apnea and resistant hypertension. Chest. 2007;132(6):1858–62. https://doi.org/10.1378/chest.07-1170.
Pedrosa RP, Drager LF, Gonzaga CC, Sousa MG, de Paula LKG, Amaro ACS, et al. Obstructive sleep apnea: the most common secondary cause of hypertension associated with resistant hypertension. Hypertension. 2011;58(5):811–7. https://doi.org/10.1161/HYPERTENSIONAHA.111.179788.
Demede M, Pandey A, Zizi F, Bachmann R, Donat M, McFarlane SI, et al. Resistant hypertension and obstructive sleep apnea in the primary-care setting. Int J Hypertens Hindawi. 2011;2011:340929.
Chen L, Kuang J, Pei J-H, Chen H-M, Chen Z, Li Z-W, et al. Continuous positive airway pressure and diabetes risk in sleep apnea patients: a systemic review and meta-analysis. Eur J Intern Med. 2017;39:39–50. https://doi.org/10.1016/j.ejim.2016.11.010.
Lin M-T, Lin H-H, Lee P-L, Weng P-H, Lee C-C, Lai T-C, et al. Beneficial effect of continuous positive airway pressure on lipid profiles in obstructive sleep apnea: a meta-analysis. Sleep Breath. 2015;19(3):809–17. https://doi.org/10.1007/s11325-014-1082-x.
Montesi SB, Edwards BA, Malhotra A, Bakker JP. The effect of continuous positive airway pressure treatment on blood pressure: a systematic review and meta-analysis of randomized controlled trials. J Clin Sleep Med. 2012;8(5):587–96. https://doi.org/10.5664/jcsm.2170.
Fava C, Dorigoni S, Dalle Vedove F, Danese E, Montagnana M, Guidi GC, et al. Effect of CPAP on blood pressure in patients with OSA/hypopnea. Chest. 2014;145(4):762–71. https://doi.org/10.1378/chest.13-1115.
Bratton DJ, Stradling JR, Barbé F, Kohler M. Effect of CPAP on blood pressure in patients with minimally symptomatic obstructive sleep apnoea: a meta-analysis using individual patient data from four randomised controlled trials. Thorax. 2014;69(12):1128–35. https://doi.org/10.1136/thoraxjnl-2013-204993.
Bakker JP, Edwards BA, Gautam SP, Montesi SB, Durán-Cantolla J, Aizpuru F, et al. Blood pressure improvement with continuous positive airway pressure is independent of obstructive sleep apnea severity. J Clin Sleep Med Ame Acad Sleep Med. 2014;10:365–9.
Mo LHQ. Effect of long-term continuous positive airway pressure ventilation on blood pressure in patients with obstructive and resistant hypertension: a meta-analysis of randomized controlled trial. J Clin Hypertens. 2016;18:153–8.
•• Bratton DJ, Gaisl T, Wons AM, Kohler M. CPAP vs mandibular advancement devices and blood pressure in patients with obstructive sleep apnea. JAMA. 2015;314:2280. In this randomized controlled trial, the authors showed that among patients with OSA, both CPAP and mandibular advanced devices were associated with reductions in BP. Network meta-analysis did not identify a statistically significant difference between the BP outcomes associated with these therapies.
Iftikhar IH, Valentine CW, Bittencourt LRA, Cohen DL, Fedson AC, Gíslason T, et al. Effects of continuous positive airway pressure on blood pressure in patients with resistant hypertension and obstructive sleep apnea. J Hypertens. 2014;32(12):2341–50. https://doi.org/10.1097/HJH.0000000000000372.
Liu L, Cao Q, Guo Z, Dai Q. Continuous positive airway pressure in patients with obstructive sleep apnea and resistant hypertension: a meta-analysis of randomized controlled trials. J Clin Hypertens. 2016;18(2):153–8. https://doi.org/10.1111/jch.12639.
Muxfeldt ES, Margallo V, Costa LMS, Guimaraes G, Cavalcante AH, Azevedo JCM, et al. Effects of continuous positive airway pressure treatment on clinic and ambulatory blood pressures in patients with obstructive sleep apnea and resistant hypertension: a randomized controlled trial. Hypertension. 2015;65(4):736–42. https://doi.org/10.1161/HYPERTENSIONAHA.114.04852.
Phillips CL, Yee BJ, Marshall NS, Liu PY, Sullivan DR, Grunstein RR. Continuous positive airway pressure reduces postprandial lipidemia in obstructive sleep apnea: a randomized, placebo-controlled crossover trial. Am J Respir Crit Care Med. 2011;184(3):355–61. https://doi.org/10.1164/rccm.201102-0316OC.
Iftikhar IH, Hoyos CM, Phillips CL, Magalang UJ. Meta-analyses of the association of sleep apnea with insulin resistance, and the effects of CPAP on HOMA-IR, adiponectin, and visceral adipose fat. J Clin Sleep Med. 2015;11(4):475–85. https://doi.org/10.5664/jcsm.4610.
Martínez-Cerón E, Barquiel B, Bezos A-M, Casitas R, Galera R, García-Benito C, et al. Effect of continuous positive airway pressure on glycemic control in patients with obstructive sleep apnea and type 2 diabetes. A randomized clinical trial. Am J Respir Crit Care Med. 2016;194(4):476–85. https://doi.org/10.1164/rccm.201510-1942OC.
Feng Y, Zhang Z, Dong Z. Effects of continuous positive airway pressure therapy on glycaemic control, insulin sensitivity and body mass index in patients with obstructive sleep apnoea and type 2 diabetes: a systematic review and meta-analysis. npj Prim Care Respir Med. 2015;25(1):15005. https://doi.org/10.1038/npjpcrm.2015.5.
Guo J, Sun Y, Xue L-J, Huang Z-Y, Wang Y-S, Zhang L, et al. Effect of CPAP therapy on cardiovascular events and mortality in patients with obstructive sleep apnea: a meta-analysis. Sleep Breath. 2016;20(3):965–74. https://doi.org/10.1007/s11325-016-1319-y.
Drager LF, Brunoni AR, Jenner R, Lorenzi-Filho G, Bensenor IM, Lotufo PA. Effects of CPAP on body weight in patients with obstructive sleep apnoea: a meta-analysis of randomised trials. Thorax. 2015;70(3):258–64. https://doi.org/10.1136/thoraxjnl-2014-205361.
•• Marin JM, Carrizo SJ, Vicente E, Agusti AG. Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet. 2005;365:1046–53. In this observational study, the authors described that, in men, severe OSA significantly increases the risk of fatal and non-fatal cardiovascular events and CPAP treatment reduces this risk.
•• Barbé F, Durán-Cantolla J, Sánchez-de-la-Torre M, Martínez-Alonso M, Carmona C, Barceló A, et al. Effect of continuous positive airway pressure on the incidence of hypertension and cardiovascular events in nonsleepy patients with obstructive sleep apnea. JAMA. 2012;307:2161–8. The results of this RCT highlight the importance of the compliance with CPAP to achieve benefits in cardiovascular risk reduction in OSA patients for primary prevention.
Valham F, Mooe T, Rabben T, Stenlund H, Wiklund U, Franklin KA. Increased risk of stroke in patients with coronary artery disease and sleep apnea: a 10-year follow-up. Circulation. 2008;118(9):955–60. https://doi.org/10.1161/CIRCULATIONAHA.108.783290.
Lee C-H, Sethi R, Li R, Ho H-H, Hein T, Jim M-H, et al. Obstructive sleep apnea and cardiovascular events after percutaneous coronary intervention clinical perspective. Circulation. 2016;133(21):2008–17. https://doi.org/10.1161/CIRCULATIONAHA.115.019392.
Fein AS, Shvilkin A, Shah D, Haffajee CI, Das S, Kumar K, et al. Treatment of obstructive sleep apnea reduces the risk of atrial fibrillation recurrence after catheter ablation. J Am Coll Cardiol. 2013;62(4):300–5. https://doi.org/10.1016/j.jacc.2013.03.052.
Holmqvist F, Guan N, Zhu Z, Kowey PR, Allen LA, Fonarow GC, et al. Impact of obstructive sleep apnea and continuous positive airway pressure therapy on outcomes in patients with atrial fibrillation—results from the outcomes registry for better informed treatment of atrial fibrillation (ORBIT-AF). Am Heart J. 2015;169(5):647–654.e2. https://doi.org/10.1016/j.ahj.2014.12.024.
Wang H, Parker JD, Newton GE, Floras JS, Mak S, Chiu K-L, et al. Influence of obstructive sleep apnea on mortality in patients with heart failure. J Am Coll Cardiol. 2007;49(15):1625–31. https://doi.org/10.1016/j.jacc.2006.12.046.
Lyons OD, Ryan CM. Sleep apnea and stroke. Can J Cardiol. 2015;31:918–27.
Peker Y, Glantz H, Eulenburg C, Wegscheider K, Herlitz J, Thunström E. Effect of positive airway pressure on cardiovascular outcomes in coronary artery disease patients with nonsleepy obstructive sleep apnea. The RICCADSA randomized controlled trial. Am J Respir Crit Care Med. 2016;194(5):613–20. https://doi.org/10.1164/rccm.201601-0088OC.
Parra O, Sánchez-Armengol Á, Capote F, Bonnin M, Arboix A, Campos-Rodríguez F, et al. Efficacy of continuous positive airway pressure treatment on 5-year survival in patients with ischaemic stroke and obstructive sleep apnea: a randomized controlled trial. J Sleep Res. 2015;24(1):47–53. https://doi.org/10.1111/jsr.12181.
McEvoy RD, Antic NA, Heeley E, Luo Y, Ou Q, Zhang X, et al. CPAP for prevention of cardiovascular events in obstructive sleep apnea. N Engl J Med. 2016;375(10):919–31. https://doi.org/10.1056/NEJMoa1606599.
Esquinas C, Sánchez-de-la Torre M, Aldomá A, Florés M, Martínez M, Barceló A, et al. Rationale and methodology of the impact of continuous positive airway pressure on patients with ACS and nonsleepy OSA: the ISAACC trial. Clin Cardiol. 2013;36(9):495–501. https://doi.org/10.1002/clc.22166.
Yu J, Zhou Z, McEvoy RD, Anderson CS, Rodgers A, Perkovic V, et al. Association of positive airway pressure with cardiovascular events and death in adults with sleep apnea: a systematic review and meta-analysis. JAMA. 2017;318(2):156–66. https://doi.org/10.1001/jama.2017.7967.
•• Bailly S, Destors M, Grillet Y, Richard P, Stach B, Vivodtzev I, et al. Obstructive sleep apnea: a cluster analysis at time of diagnosis. Paul F, editor. PLoS One. 2016;11:e0157318. This study is a cluster analysis of a wide cohort of OSA patients that contributes with relevant information about the clinical profile of OSA patients that develop cardiovascular comorbidity.
Castro-Grattoni AL, Torres G, Martínez-Alonso M, Barbé F, Turino C, Sánchez-de-la-Torre A, et al. Blood pressure response to CPAP treatment in subjects with obstructive sleep apnoea: the predictive value of 24-h ambulatory blood pressure monitoring. Eur Respir J. 2017;50(4):1700651. https://doi.org/10.1183/13993003.00651-2017.
•• Sánchez-de-la-Torre M, Khalyfa A, Sánchez-de-la-Torre A, Martinez-Alonso M, Martinez-García MÁ, Barceló A, et al. Precision medicine in patients with resistant hypertension and obstructive sleep apnea: blood pressure response to continuous positive airway pressure treatment. J Am Coll Cardiol. 2015;66:1023–32. In this study, the authors described the first personalized medicine tool to predict blood pressure response to CPAP treatment in patients with resistant hypertension and OSA.
Acknowledgements
The study was supported by Fondo de Investigación Sanitaria, Fondo Europeo de Desarrollo Regional (FEDER) (PI14/01266; PI16/00489; DTS15/00145), the Spanish Respiratory Society (SEPAR), Young Researchers Award from the AstraZeneca Foundation, and ALLER.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Gerard Torres, Cecilia Turino, Esther Sapiña, Manuel Sánchez-de-la-Torre, and Ferran Barbé declare no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Sleep and 3D (Cancer, Cardiovascular, Metabolic Diseases)
Rights and permissions
About this article
Cite this article
Torres, G., Turino, C., Sapiña, E. et al. Sleep Apnea and Cardiovascular Morbidity—a Perspective. Curr Sleep Medicine Rep 4, 79–87 (2018). https://doi.org/10.1007/s40675-018-0108-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40675-018-0108-5