Abstract
Background
Oral chemotherapy use is increasing due to new drug approvals as well as the convenience of the administration of oral drugs. This increased use also raises concern regarding drug–drug interactions (DDIs) with concomitantly administered drugs, resulting in loss of therapeutic effect, decreased tolerability, and/or increased toxicity.
Objective
The objective of this study was to review existing evidence of the clinical impact of DDIs with oral chemotherapeutic agents.
Methods
A comprehensive search of literature using PubMed was conducted in April 2018 for studies of DDIs associated with oral chemotherapy. Included studies were in English. We included randomized clinical trials, observational studies, and case reports evaluating a DDI between any oral chemotherapy drug and any other drug. Included studies needed to have at least one outcome of clinical relevance potentially attributed to the DDI, for example, effects on survival or toxicity. The quality of the articles was determined using published metrics appropriate for the study design.
Results
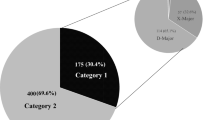
There were 2626 studies identified in the initial search, of which 35 met all eligibility criteria. These included 15 retrospective cohort studies, 16 case reports or case series and four post hoc analyses of clinical trials. Among these, DDIs contributed to a statistically significant change in a clinical outcome in 12 studies. Eight of these studies evaluated overall survival and progression-free survival and found that the presence of the DDI was associated with reduced survival.
Conclusion
Our findings suggest that more real-world studies evaluating the association between oral chemotherapy DDIs and clinical outcomes are needed. The adverse clinical outcomes due to DDIs may be a reason for treatment failures and therapy discontinuation.

Similar content being viewed by others
References
Roop JC, Wu HS. Current practice patterns for oral chemotherapy: results of a national survey. Oncol Nurs Forum. 2014;41(2):185–94.
Sun J, et al. A systematic analysis of FDA-approved anticancer drugs. BMC Syst Biol. 2017;11(Suppl 5):87. https://doi.org/10.1186/s12918-017-0464-7.
Bartel SB. Safe practices and financial considerations in using oral chemotherapeutic agents. Am J Health Syst Pharm. 2007;64(9 Suppl 5):S8–14.
Sharma M, et al. Polypharmacy and potentially inappropriate medication use in geriatric oncology. J Geriatr Oncol. 2016;7(5):346–53.
Solomon JM, et al. Evaluation of the prescribing patterns, adverse effects, and drug interactions of oral chemotherapy agents in an outpatient cancer center. J Oncol Pharm Pract. 2018. https://doi.org/10.1177/1078155218798150.
van Leeuwen RW, et al. Prevalence of potential drug-drug interactions in cancer patients treated with oral anticancer drugs. Br J Cancer. 2013;108(5):1071–8.
Gustafson E, Kettle J. Analyzing trends in oral anticancer agents in an academic medical facility. J Hematol Oncol Pharm. 2015;5(2):34–7.
Wells GA, O’Connell BS, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2018. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 16 Aug 2018.
Murad MH, Sultan S, Haffar S, Bazerbachi F. Methodological quality and synthesis of case series and case reports. BMJ Evid Based Med. 2018;23:60–63.
Xing D, et al. Osteoarthritis and all-cause mortality in worldwide populations: grading the evidence from a meta-analysis. Sci Rep. 2016;6:24393.
Casadei Gardini A, et al. Metformin and insulin impact on clinical outcome in patients with advanced hepatocellular carcinoma receiving sorafenib: validation study and biological rationale. Eur J Cancer. 2017;86:106–14.
Chen YM, et al. Antacid use and de novo brain metastases in patients with epidermal growth factor receptor-mutant non-small cell lung cancer who were treated using first-line first-generation epidermal growth factor receptor tyrosine kinase inhibitors. PLoS One. 2016;11(2):e0149722.
Chen H, et al. Synergistic effects of metformin in combination with EGFR-TKI in the treatment of patients with advanced non-small cell lung cancer and type 2 diabetes. Cancer Lett. 2015;369(1):97–102.
Chu MP, et al. Gastric Acid suppression is associated with decreased erlotinib efficacy in non-small-cell lung cancer. Clin Lung Cancer. 2015;16(1):33–9.
Ha VH, et al. Does gastric acid suppression affect sunitinib efficacy in patients with advanced or metastatic renal cell cancer? J Oncol Pharm Pract. 2015;21(3):194–200.
Kelly CM, et al. Selective serotonin reuptake inhibitors and breast cancer mortality in women receiving tamoxifen: a population based cohort study. BMJ. 2010;340:c693.
Kumarakulasinghe NB, et al. EGFR kinase inhibitors and gastric acid suppressants in EGFR-mutant NSCLC: a retrospective database analysis of potential drug interaction. Oncotarget. 2016;7(51):85542–50.
Lam LH, Capparelli EV, Kurzrock R. Association of concurrent acid-suppression therapy with survival outcomes and adverse event incidence in oncology patients receiving erlotinib. Cancer Chemother Pharmacol. 2016;78(2):427–32.
Zenke Y, et al. Clinical impact of gastric acid-suppressing medication use on the efficacy of erlotinib and gefitinib in patients with advanced non-small-cell lung cancer harboring EGFR mutations. Clin Lung Cancer. 2016;17(5):412–8.
Samaras P, et al. Concomitant statin use does not impair the clinical outcome of patients with diffuse large B cell lymphoma treated with rituximab-CHOP. Ann Hematol. 2010;89(8):783–7.
Lalani AA, et al. Proton pump inhibitors and survival outcomes in patients with metastatic renal cell carcinoma. Clin Genitourin Cancer. 2017;15(6):724–32.
Hilton JF, et al. An evaluation of the possible interaction of gastric acid suppressing medication and the EGFR tyrosine kinase inhibitor erlotinib. Lung Cancer. 2013;82(1):136–42.
Siegelmann-Danieli N, et al. Potent CYP2D6 Inhibiting drugs do not increase relapse rate in early breast cancer patients treated with adjuvant tamoxifen. Breast Cancer Res Treat. 2011;125(2):505–10.
Chu MP, et al. Association of proton pump inhibitors and capecitabine efficacy in advanced gastroesophageal cancer: secondary analysis of the TRIO-013/LOGiC randomized clinical trial. JAMA Oncol. 2017;3(6):767–73.
Relling MV, et al. Adverse effect of anticonvulsants on efficacy of chemotherapy for acute lymphoblastic leukaemia. Lancet. 2000;356(9226):285–90.
Isaacs K, Haim N. Adverse interaction between capecitabine and warfarin resulting in altered coagulation parameters and bleeding: case report and review of the literature. J Chemother. 2005;17(3):339–42.
Janney LM, Waterbury NV. Capecitabine-warfarin interaction. Ann Pharmacother. 2005;39(9):1546–51.
Shah HR, et al. A retrospective study of coagulation abnormalities in patients receiving concomitant capecitabine and warfarin. Clin Colorect Cancer. 2006;5(5):354–8.
Ikenishi M, et al. A study on drug interaction between warfarin and capecitabine with special reference to the co-administered term or the discontinuation term of capecitabine. Gan To Kagaku Ryoho. 2015;42(7):833–9.
Thomas KS, et al. Elevated international normalized ratio associated with concomitant warfarin and erlotinib. Am J Health Syst Pharm. 2010;67(17):1426–9.
Moretti LV, Montalvo RO. Elevated International Normalized Ratio associated with concurrent use of sorafenib and warfarin. Am J Health Syst Pharm. 2009;66(23):2123–5.
Lim S, Houranieh J, Crawford R. Elevated International Normalized Ratio in a patient concurrently using warfarin and vismodegib. Am J Health Syst Pharm. 2014;71(3):200–3.
Wiczer T, et al. Evaluation of incidence and risk factors for high-dose methotrexate-induced nephrotoxicity. J Oncol Pharm Pract. 2016;22(3):430–6.
Jolivot PA, et al. A case of melphalan sustained accumulation in an 80-year old patient. Int J Clin Pharm. 2015;37(6):984–7.
Mulder KE, Egorin MJ, Sawyer MB. Renal dysfunction in a renal transplant patient treated concurrently with cyclosporine and imatinib. Invest New Drugs. 2012;30(6):2400–2.
Kim K, et al. Regorafenib in advanced hepatocellular carcinoma (HCC): considerations for treatment. Cancer Chemother Pharmacol. 2017;80(5):945–54.
Ashrafi F, et al. Osteonecrosis of the jaws in patient received bisphosphonates and sunitinib separately: a case report. J Res Pharm Pract. 2017;6(3):182–5.
Zimmerman MS, Ruckdeschel JC, Hussain M. Chemotherapy-induced interstitial pneumonitis during treatment of small cell anaplastic lung cancer. J Clin Oncol. 1984;2(5):396–405.
Baena-Cañada JM, et al. Interaction between capecitabine and brivudin in a patient with breast cancer. Nat Rev Clin Oncol. 2010;7(1):55–8.
Yin OQ, et al. Concurrent use of proton pump inhibitors or H2 blockers did not adversely affect nilotinib efficacy in patients with chronic myeloid leukemia. Cancer Chemother Pharmacol. 2012;70(2):345–50.
Severino G, et al. Adverse reactions during imatinib and lansoprazole treatment in gastrointestinal stromal tumors. Ann Pharmacother. 2005;39(1):162–4.
Segal EM, et al. Oral chemotherapy food and drug interactions: a comprehensive review of the literature. J Oncol Pract. 2014;10(4):e255–68.
American Geriatrics Society 2015 updated beers criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2015;63(11):2227–46.
O’Mahony D, et al. STOPP/START criteria for potentially inappropriate prescribing in older people: version 2. Age Ageing. 2015;44(2):213–8.
Kruse V, et al. Sunitinib for metastatic renal cell cancer patients: observational study highlighting the risk of important drug-drug interactions. J Clin Pharm Ther. 2014;39(3):259–65.
Lambert Kuhn E, et al. Adverse event potentially due to an interaction between ibrutinib and verapamil: a case report. J Clin Pharm Ther. 2016;41(1):104–5.
Ozenne V, et al. Suspected interaction between sorafenib and HAART in an HIV-1 infected patient: a case report. Hepatogastroenterology. 2011;58(105):161–2.
Hashimoto S, et al. Fatal thromboembolism in acute promyelocytic leukemia during all-trans retinoic acid therapy combined with antifibrinolytic therapy for prophylaxis of hemorrhage. Leukemia. 1994;8(7):1113–5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The work in this manuscript was supported in part by CCSG P30 CA016672, a Cancer Center Support (CORE) grant to MD Anderson Cancer Center.
Conflict of interest
Mariana Chavez-MacGregor has received institutional research support from Novartis. Manvi Sharma, Aisha Vadhariya, Soumya Chikermane, Suma Gopinathan, Sharon H. Giordano, Michael L. Johnson, and Holly M. Holmes declare that they have no conflicts of interest that might be relevant to the contents of this manuscript.
Rights and permissions
About this article
Cite this article
Sharma, M., Vadhariya, A., Chikermane, S. et al. Clinical Outcomes Associated with Drug–Drug Interactions of Oral Chemotherapeutic Agents: A Comprehensive Evidence-Based Literature Review. Drugs Aging 36, 341–354 (2019). https://doi.org/10.1007/s40266-019-00640-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-019-00640-5