Abstract
Background
In the presence of multimorbidity and limited life expectancy (LLE), the need for continued use of preventive medicines becomes uncertain as they may neither improve health nor confer continued health benefits.
Objective
Our objective was to systematically review the literature to examine the discontinuation of preventive medicines in older people with LLE.
Methods
A systematic literature search was conducted using the Ovid MEDLINE, Embase, Cumulative Index to Nursing and Allied Health Literature, and the Cochrane Central Register databases. Studies investigating discontinuation of preventive medicines in older individuals (mean age ≥65 years) with LLE (≤12 months) published between 1 January 1997 and 28 February 2017 were included. The Cochrane risk-of-bias assessment criteria and the Newcastle–Ottawa Scale were used to assess the quality of the studies.
Results
Ten studies—a randomized controlled trial (RCT), two case–control studies, and seven cohort studies—involving 26,854 participants with a mean age ranging from 66.0 to 85.0 years were included in this review. The studies were primarily conducted in palliative care (n = 3), residential facility (n = 2), and community (n = 1) settings, and the remainder were pharmacoepidemiological studies (n = 4). The most common life-limiting illnesses were cancer (n = 5), followed by other unspecified illnesses (n = 4) and advanced dementia (n = 1). The most common preventive medicine discontinued was statins, followed by warfarin and aspirin. LLE potentially prompted discontinuation; however, some individuals continued to receive preventive medicines until they died.
Conclusions
The review found that withdrawal of preventive medicines at the end of life is challenging. Decisions about the discontinuation of preventive medicines for individuals approaching the end of life are increasingly complicated by the lack of clear deprescribing guidelines for these medicines.

Similar content being viewed by others
References
Narayan SW, Tordoff JM, Nishtala PS. Temporal trends in the utilisation of preventive medicines by older people: a 9-year population-based study. Arch Gerontol Geriatr. 2016;62:103–11.
McNeil MJ, Kamal AH, Kutner JS, Ritchie CS, Abernethy AP. The Burden of polypharmacy in patients near the end of life. J Pain Symptom Manage. 2016;51(2):178–83.e2.
Nishtala PS, Narayan SW, Wang T, Hilmer SN. Associations of drug burden index with falls, general practitioner visits, and mortality in older people. Pharmacoepidemiol Drug Saf. 2014;23(7):753–8.
Narayan SW, Nishtala PS. Associations of potentially inappropriate medicine use with fall-related hospitalisations and primary care visits in older New Zealanders: a population-level study using the updated 2012 Beers Criteria. Drugs Real World Outcomes. 2015;2(2):137–41.
Todd A, Husband A, Andrew I, et al. Inappropriate prescribing of preventative medication in patients with life-limiting illness: a systematic review. BMJ Support Palliat Care. 2017;7(2):113–21.
Narayan SW, Nishtala PS. Decade-long temporal trends in the utilization of preventive medicines by centenarians. J Clin Pharm Ther. 2017;42(2):165–9. doi:10.1111/jcpt.12487 (Epub 2016 Dec 10).
Kakar P. Preventive medicine in the older patient: a United Kingdom perspective. Int J Prev Med. 2012;3(6):379–85.
Currow DC, Abernethy AP. Frameworks for approaching prescribing at the end of life. Arch Intern Med. 2006;166(21):2404.
Bain KT, Holmes HM, Beers MH, et al. Discontinuing medications: a novel approach for revising the prescribing stage of the medication-use process. J Am Geriatr Soc. 2008;56(10):1946–52.
Parsons C, Hughes CM, Passmore AP, Lapane KL. Withholding, discontinuing and withdrawing medications in dementia patients at the end of life: a neglected problem in the disadvantaged dying? Drugs Aging. 2010;27(6):435–49.
Kutner JS, Blatchford PJ, Taylor DH Jr, et al. Safety and benefit of discontinuing statin therapy in the setting of advanced, life-limiting illness: a randomized clinical trial. JAMA Intern Med. 2015;175(5):691–700.
Bayliss EA, Bronsert MR, Reifler LM, et al. Statin prescribing patterns in a cohort of cancer patients with poor prognosis. J Palliat Med. 2013;16(4):412–8.
Riechelmann RP, Krzyzanowska MK, Zimmermann C. Futile medication use in terminally ill cancer patients. Support Care Cancer. 2009;17(6):745–8.
Ailabouni NJ, Nishtala PS, Mangin D, Tordoff JM. General practitioners’ insight into deprescribing for the multimorbid older individual: a qualitative study. Int J Clin Pract. 2016;70(3):261–76.
Holmes HM, Hayley DC, Alexander GC, Sachs GA. Reconsidering medication appropriateness for patients late in life. Arch Intern Med. 2006;166(6):605–9.
Stevenson J, Abernethy AP, Miller C, Currow DC. Managing comorbidities in patients at the end of life. BMJ. 2004;329(7471):909–12.
Schuling J, Gebben H, Veehof LJ, Haaijer-Ruskamp FM. Deprescribing medication in very elderly patients with multimorbidity: the view of Dutch GPs. A qualitative study. BMC Fam Pract. 2012;13:56.
Todd A, Nazar H, Pearson S, et al. Inappropriate prescribing in patients accessing specialist palliative day care services. Int J Clin Pharm. 2014;36(3):535–43.
The New Zealand Formulary. http://nzformulary.org/. Accessed 22 July 2016.
The Cochrane Collaboration’s tool for assessing risk of bias. London: Cochrane Collaboration. http://handbook.cochrane.org/chapter_8/8_5_the_cochrane_collaborations_tool_for_assessing_risk_of_bias.htm. Accessed 24 Mar 2017.
The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 24 Mar 2017.
STROBE Statement. https://www.strobe-statement.org/index.php?id=strobe-home. Accessed 24 Mar 2017.
Hoffmann TC, Glasziou PP, Boutron I, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ. 2014;348:g1687.
Tjia J, Cutrona SL, Peterson D, et al. Statin discontinuation in nursing home residents with advanced dementia. J Am Geriatr Soc. 2014;62(11):2095–101.
Bertozzo G, Zoppellaro G, Granziera S, et al. Reasons for and consequences of vitamin K antagonist discontinuation in very elderly patients with non-valvular atrial fibrillation. J Thromb Haemost. 2016;14(11):2124–31.
Stavrou EP, Buckley N, Olivier J, Pearson SA. Discontinuation of statin therapy in older people: does a cancer diagnosis make a difference? An observational cohort study using data linkage. BMJ Open. 2012;2(3):1–6.
Tanvetyanon T, Choudhury AM. Physician practice in the discontinuation of statins among patients with advanced lung cancer. J Palliat Care. 2006;22(4):281–5.
Nishtala PS, Gnjidic D, Chyou T, Hilmer SN. Discontinuation of statins in a population of older New Zealanders with limited life expectancy. Intern Med J. 2016;46(4):493–6.
Silveira MJ, Kazanis AS, Shevrin MP. Statins in the last six months of life: a recognizable, life-limiting condition does not decrease their use. J Palliat Med. 2008;11(5):685–93.
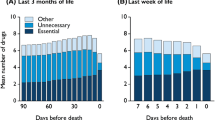
Currow DC, Stevenson JP, Abernethy AP, Plummer J, Shelby-James TM. Prescribing in palliative care as death approaches. J Am Geriatr Soc. 2007;55(4):590–5.
Holmes HM, Min LC, Yee M, et al. Rationalizing prescribing for older patients with multimorbidity: considering time to benefit. Drugs Aging. 2013;30(9):655–66.
Holmes HM, Todd A. Evidence-based deprescribing of statins in patients with advanced illness. JAMA Intern Med. 2015;175(5):701–2.
Poudel A, Yates P, Rowett D, Nissen LM. Use of preventive medication in patients with limited life expectancy: a systematic review. J Pain Symptom Manage. 2017;53(6):1097–1110.e1. doi: 10.1016/j.jpainsymman.2016.12.350 (Epub 2017 Feb 9).
Todd A, Husband A, Andrew I, et al. Inappropriate prescribing of preventative medication in patients with life-limiting illness: a systematic review. BMJ Support Palliat Care. 2017;7(2):113–21. doi:10.1136/bmjspcare-2015-000941 (Epub 2016 Jan 5).
Lee SJ, Leipzig RM, Walter LC. Incorporating lag time to benefit into prevention decisions for older adults. JAMA. 2013;310(24):2609–10.
American Geriatrics Society Beers Criteria Update Expert Panel. American Geriatrics Society updated Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2012;60(4):616–31.
Shrank WH, Polinski JM, Avorn J. Quality indicators for medication use in vulnerable elders. J Am Geriatr Soc. 2007;55(Suppl 2):S373–82.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The authors thank the RiPE (Research in Pharmacoepidemiology) group, School of Pharmacy, University of Otago, New Zealand, for providing support. Sujita Narayan is supported by a doctoral scholarship from the School of Pharmacy, University of Otago, Dunedin, New Zealand. The funding institution did not play a role in the study concept, data analysis, or interpretation.
Conflicts of interest
Sujita Narayan and Prasad Nishtala have no conflicts of interest relevant to the content of this review.
Ethical considerations
All patient data evaluated in this review were de-identified.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Narayan, S.W., Nishtala, P.S. Discontinuation of Preventive Medicines in Older People with Limited Life Expectancy: A Systematic Review. Drugs Aging 34, 767–776 (2017). https://doi.org/10.1007/s40266-017-0487-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-017-0487-1