Abstract
Purpose of the Review
Frailty as a concept has been developed a lot during the last 25 years. From its start in geriatrics, its usefulness has also been demonstrated in most other clinical specialties including anesthesia, surgery, and intensive care. Several tools have been found useful to characterize frailty status: frailty phenotype, clinical frailty scale, or specific scores for surgical patients. The purpose of this review is to discuss how frailty interactive with acute critical illness and may alter ICU outcomes, particularly in the old patients.
Recent Findings
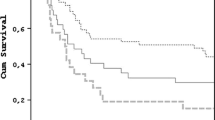
Frailty has in many studies been found to have a substantial impact on most outcome parameters in ICU patients, mainly mortality, but also as non-mortality outcomes. Risk ratio for mortality in frail versus non-frail ICU patients is significantly increased.
Frailty affects several important body functions like the endocrine system and brain, muscular, and immune functions. In the ICU, these impaired body functions add to the traditional acute vital organ dysfunctions, well described in the ICU patient. This combination of reduced body function in patients that in addition develops a critical illness is the most likely cause of not only increased short-term but also long-term mortality found in frail ICU patients.
Summary
This review summarizes current tools to identify frailty and summarizes recent findings of the prognostic role of frailty in the ICU.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Shem Tov L, Matot I. Frailty and anesthesia. Curr Opin Anaesthesiol. 2017;30(3):409–17. https://doi.org/10.1097/ACO.0000000000000456.
Hewitt J, Long S, Carter B, Bach S, McCarthy K, Clegg A. The prevalence of frailty and its association with clinical outcomes in general surgery: a systematic review and meta-analysis. Age Ageing. 2018;47(6):793–800. https://doi.org/10.1093/ageing/afy110.
McDermid RC, Bagshaw SM. Scratching the surface: the burden of frailty in critical care. Intensive Care Med. 2014;40(5):740–2. https://doi.org/10.1007/s00134-014-3246.
•• Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet. 2013;381(9868):752–62. https://doi.org/10.1016/S0140-6736(12)62167-9. A comprehensive review of frailty in the elderly.
•• Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146–56. A classical study and evaluation of the concept of frailty, making way for the phenotype model to describe frailty.
•• Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, et al. A global clinical measure of fitness and frailty in elderly people. Can Med Assoc J. 2005;173(5):489–95. https://doi.org/10.1503/cmaj.050051. Results from a large Canadian study of frailty, resulting in the alternative description of frailty as cumulative deficits.
Farhat JS, Velanovich V, Falvo AJ, Horst HM, Swartz A, Patton JH Jr, et al. Are the frail destined to fail? Frailty index as predictor of surgical morbidity and mortality in the elderly. J Trauma Acute Care Surg. 2012;72(6):1526–30. https://doi.org/10.1097/TA.0b013e3182542fab.
Flaatten H, Clegg A. Frailty: we need valid and reliable tools in critical care. Intensive Care Med. 2018;56(11):M146–3. https://doi.org/10.1007/s00134-018-5404-5.
Clegg A, Bates C, Young J, Ryan R, Nichols L, Ann Teale E, et al. Development and validation of an electronic frailty index using routine primary care electronic health record data. Age Ageing. 2016;45(3):353–30. https://doi.org/10.1093/ageing/afw039.
Le Maguet P, Roquilly A, Lasocki S, Asehnoune K, Carise E, Saint Martin M, et al. Prevalence and impact of frailty on mortality in elderly ICU patients: a prospective, multicenter, observational study. Intensive Care Med. 2014;40(5):674–82. https://doi.org/10.1007/s00134-014-3253-4.
Chong E, Ho E, Baldevarona-Llego J, Chan M, Wu L, Tay L. Frailty and risk of adverse outcomes in hospitalized older adults: a comparison of different frailty measures. J Am Med Dir Assoc. 2017;18(7):638.e7–638.e11. https://doi.org/10.1016/j.jamda.2017.04.011.
• Muscedere J, Waters B, Varambally A, Bagshaw SM, Boyd JG, Maslove D, et al. The impact of frailty on intensive care unit outcomes: a systematic review and meta-analysis. Intensive Care Med. 2017;43(8):1105–22. https://doi.org/10.1007/s00134-017-4867-0. A large meta-analysis of frailty impact on outcomes in ICU patients.
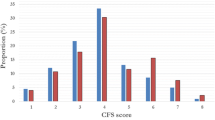
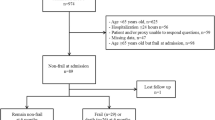
• Flaatten H, de Lange DW, Morandi A, Andersen FH, Artigas A, Bertolini G, et al. The impact of frailty on ICU and 30-day mortality and the level of care in very elderly patients (≥ 80 years). Intensive Care Med. 2017;43(12):1820–8. https://doi.org/10.1007/s00134-017-4940-8. The largest prospective multi-national study on frailty in elderly ICU patients.
The VIP2 study. https://www.vip2study.com/. Accessed 1 Feb 2019.
Zampieri FG, Iwashyna TJ, Viglianti EM, Taniguchi LU, Viana WN, Costa R, et al. Association of frailty with short-term outcomes, organ support and resource use in critically ill patients. Intensive Care Med. 2018;44(9):1512–20. https://doi.org/10.1007/s00134-018-5342-2.
Guidet B, Flaatten H, Boumendil A, Morandi A, Andersen F, Artigas A, et al. Withholding or withdrawing of life sustaining therapy in very elderly patients (≥ 80 years) admitted to the intensive care unit. Intensive Care Med. 2018;44(7):1027–38. https://doi.org/10.1007/s00134-018-5196-7.
Brummel NE, Bell SP, Girard TD, Pandharipande PP, Jackson JC, Morandi A, et al. Frailty and subsequent disability and mortality among patients with critical illness. Am J Respir Crit Care Med. 2017;196(1):64–72. https://doi.org/10.1164/rccm.201605-0939OC.
Heyland DK, Garland A, Bagshaw SM, Cook D, Rockwood K, Stelfox HT, et al. Recovery after critical illness in patients aged 80 years or older: a multi-center prospective observational cohort study. Intensive Care Med. 2015;41(11):1911–20. https://doi.org/10.1007/s00134-015-4028-2.
Hope AA, Hsieh SJ, Petti A, Hurtado-Sbordoni M, Verghese J, Gong MN. Assessing the usefulness and validity of frailty markers in critically ill adults. Ann Am Thorac Soc. 2017;14(6):952–9. https://doi.org/10.1513/AnnalsATS.201607-538OC.
Kim S-w, Han H-S, Jung H-w, Kim K-i, Hwang DW, Kang S-B, et al. Multidimensional frailty score for the prediction of postoperative mortality risk. JAMA Surg. 2014;149(7):633–40. https://doi.org/10.1001/jamasurg.2014.241.
Kirkwood TB. Understanding the odd science of aging. Cell. 2005;120:437–47.
Clegg A, Hassan-Smith Z. Frailty and the endocrine system. Lancet Diabetes Endocrinol. 2018;6(9):743–52. https://doi.org/10.1016/S2213-8587(18)30110-4.
Mosoni L, Dardevet D, Combaret L, et al. Altered responses in skeletal muscle protein turnover during aging in anabolic and catabolic periods. Int J Biochem Cell Biol. 2005;37:1962–73.
Doi T, Makizako H, Tsutsumimoto K, Hotta R, Nakakubo S, Makino K, et al. Association between insulin-like growth Factor-1 and frailty among older adults. J Nutr Health Aging. 2018;22(1):68–72. https://doi.org/10.1007/s12603-017-0916-1.
Bishop NA, Lu T, Yankner BA. Neural mechanisms of ageing and cognitive decline. Nature. 2010;464:529–35. https://doi.org/10.1038/nature08983.
Cunningham C, Wilcockson DC, Campion S, Lunnon K, Perry VH. Central and systemic endotoxin challenges exacerbate the local inflammatory response and increase neuronal death during chronic neurodegeneration. J Neurosci. 2005;25:9275–84.
Eeles EMP, White SV, O'Mahony SM, Bayer AJ, Hubbard RE. The impact of frailty and delirium on mortality in older inpatients. Age Ageing. 2012;41(3):412–6. https://doi.org/10.1093/ageing/afs021.
Salluh JIF, Wang H, Schneider EB, Nagaraja N, Yenokyan G, Damluji A, et al. Outcome of delirium in critically ill patients: systematic review and meta-analysis. BMJ. 2015;350(may19):h2538. https://doi.org/10.1136/bmj.h2538.
Dodds R, Sayer AA. Sarcopenia and frailty: new challenges for clinical practice. Clin Med. 2016;16(5):455–8. https://doi.org/10.7861/clinmedicine.16-5-455.
Gale CR, Cooper C, Sayer A. Prevalence of frailty and disability: findings from the English longitudinal study of ageing. Age Ageing. 2015;44:162–5. https://doi.org/10.1093/ageing/afu/148.
Roberts HC, Denison HJ, Martin HJ, Patel HP, Syddall H, Cooper C, et al. A review of the measurement of grip strength in clinical and epidemiological studies: towards a standardised approach. Age Ageing. 2011;40:423–9. https://doi.org/10.1093/ageing/afr051.
Ticinesi A, Meschi T, Narici MV, Lauretani F, Maggio M. Muscle ultrasound and sarcopenia in older individuals: a clinical perspective. J Am Med Dir Assoc. 2017;18(4):290–300. https://doi.org/10.1016/j.jamda.2016.11.013.
Martín S, Pérez A, Aldecoa C. Sepsis and Immunosenescence in the elderly patient: a review. Front Med. 2017;4(Suppl 1):20. https://doi.org/10.3389/fmed.2017.00020.
Walston J, McBurnie MA, Newman A, Tracy RP, Kop WJ, Hirsch CH, et al. Frailty and activation of the inflammation and coagulation systems with and without clinical comorbidities: results from the cardiovascular health study. Arch Intern Med. 2002;162:2333–41.
Johnson SA, Cambier JC. Ageing, autoimmunity and arthritis: senescence of the B cell compartment - implications for humoral immunity. Arthritis Res Ther. 2004;6(4):131–9. https://doi.org/10.1186/ar1180.
Naylor K, Li G, Vallejo AN, Lee WW, Koetz K, Bryl E, et al. The influence of age on T cell generation and TCR diversity. J Immunol. 2005;174(11):7446–52.
Sansoni P, Vescovini R, Fagnoni F, Biasini C, Zanni F, Zanlari L, et al. The immune system in extreme longevity. Exp Gerontol. 2008;43(2):61–5. https://doi.org/10.1016/j.exger.2007.06.008.
Fulop T, Larbi A, Douziech N, Fortin C, Guerard KP, Lesur O, et al. Signal transduction and functional changes in neutrophils with aging. Aging Cell. 2004;3(4):217–26. https://doi.org/10.1111/j.1474-9728.2004.00110.x.
Knoop ST, Skrede S, Langeland N, Flaatten HK. Epidemiology and impact on all-cause mortality of sepsis in Norwegian hospitals: a national retrospective study. PLoS One. 2017;12(11):e0187990. https://doi.org/10.1371/journal.pone.0187990.
Vincent JL, de Mendonça A, Cantraine F, Moreno R, Takala J, Suter PM, et al. Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Working group on “sepsis-related problems” of the European Society of Intensive Care Medicine. Crit Care Med. 1998;26(11):1793–800.
Minne L, Ludikhuize J, de Jonge E, de Rooij S, Abu-Hanna A. Prognostic models for predicting mortality in elderly ICU patients: a systematic review. Intensive Care Med. 2011;37(8):1258–68. https://doi.org/10.1007/s00134-011-2265-6.
Flaatten H, Oyen S, deLange D. Predicting outcomes in very old ICU patients: time to focus on the past? ICM. 2018;44:1344–5. https://doi.org/10.1007/s00134-018-5262-1.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Hans Flaatten declares that he has no conflict of interest.
Christian Jung has received research funding from Actelion Pharmaceuticals, Bayer Healthcare, Vifor Pharma, ZOLL Medical Corporation, Novartis, and Medicure, Inc.; has received compensation from Actelion Pharmaceuticals, Bayer Healthcare, Vifor Pharma, ZOLL Medical Corporation, Pfizer, Bristol-Myers Squibb, Abbott Vascular, Boston Scientific, Boehringer Ingelheim, Sanofi Aventis, Novartis, and Orion Pharma for service as a consultant; and has received non-financial support from Actelion Pharmaceuticals, Abbott Vascular, Novartis, and Orion Pharma.
Helene Vallet declares that she has no conflict of interest.
Bertrand Guidet declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Critical Care Anesthesia
Rights and permissions
About this article
Cite this article
Flaatten, H., Jung, C., Vallet, H. et al. How Does Frailty Affect ICU Outcome?. Curr Anesthesiol Rep 9, 144–150 (2019). https://doi.org/10.1007/s40140-019-00324-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40140-019-00324-1