Abstract
Background
Relative myocardial perfusion imaging may underestimate severity of coronary disease (CAD), particularly in cases of balanced ischemia. Can quantification of peak left (LV) and right (RV) ventricular Rb-82 uptake measurements identify patients with left main or 3 vessel disease?
Methods
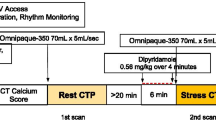
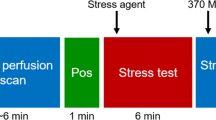
Patients (N = 169) who underwent Rb-82 PET MPI and coronary angiography were categorized as having no significant coronary stenosis (n = 60), 1 or 2 vessel disease (n = 81), or left main disease/3 vessel disease (n = 28), based on angiography. Maximal LV and RV ventricular myocardial Rb-82 uptake was measured during stress and rest.
Results
Failure to augment LV uptake by ≥ 8500 Bq/cc at stress, predicted left main or 3 vessel disease with a sensitivity of 93% and specificity of 61% (area under curve = 0.83). A ≥10% increase in RV: LV uptake ratios with stress over rest was 93% specific (area under curve = 0.74) for left main or 3 vessel disease. These indices incrementally predicted left main or 3 vessel disease compared to models including age, gender, cardiac risk factors, and summed stress and difference scores.
Conclusion
Quantifying maximal rest and stress LV and RV uptake with PET myocardial perfusion imaging may independently and incrementally identify patients with left main or 3 vessel disease.





Similar content being viewed by others
References
DePuey EG, Garcia EV. Updated imaging guidelines for nuclear cardiology procedures, part 1. J Nucl Cardiol 2001;8:G5-58.
Williams KA, Schneider CM. Increased stress right ventricular activity on dual isotope perfusion SPECT: A sign of multivessel and/or left main coronary artery disease. J Am Coll Cardiol 1999;34:420-7.
Toba M, Kumita S, Cho K, Ibuki C, Kumazaki T, Takano T. Usefulness of gated myocardial perfusion SPECT imaging soon after exercise to identify postexercise stunning in patients with single-vessel coronary artery disease. J Nucl Cardiol 2004;11:697-703.
Druz RS, Akinboboye OA, Grimson R, Nichols KJ, Reichek N. Postischemic stunning after adenosine vasodilator stress. J Nucl Cardiol 2004;11:534-41.
Abidov A, Bax JJ, Hayes SW, et al. Transient ischemic dilation ratio of the left ventricle is a significant predictor of future cardiac events in patients with otherwise normal myocardial perfusion SPECT. J Am Coll Cardiol 2003;42:1818-25.
Paul AK, Hasegawa S, Yoshioka J, et al. Characteristics of regional myocardial stunning after exercise in gated myocardial SPECT. J Nucl Cardiol 2002;9:388-94.
Marcassa C, Galli M, Baroffio C, Campini R, Giannuzzi P. Transient left ventricular dilation at quantitative stress-rest sestamibi tomography: Clinical, electrocardiographic, and angiographic correlates. J Nucl Cardiol 1999;6:397-405.
Mazzanti M, Germano G, Kiat H, et al. Identification of severe and extensive coronary artery disease by automatic measurement of transient ischemic dilation of the left ventricle in dual-isotope myocardial perfusion SPECT. J Am Coll Cardiol 1996;27:1612-20.
Chouraqui P, Rodrigues EA, Berman DS, Maddahi J. Significance of dipyridamole-induced transient dilation of the left ventricle during thallium-201 scintigraphy in suspected coronary artery disease. Am J Cardiol 1990;66:689-94.
Dorbala S, Vangala D, Sampson U, Limaye A, Kwong R, Di Carli MF. Value of vasodilator left ventricular ejection fraction reserve in evaluating the magnitude of myocardium at risk and the extent of angiographic coronary artery disease: A 82Rb PET/CT study. J Nucl Med 2007;48:349-58.
Owada K, Machii K, Tsukahara Y, et al. Quantitative estimation of the right ventricular overloading by thallium-201 myocardial scintigraphy. Jpn Circ J 1982;46:715-24.
Movahed MR, Hepner A, Lizotte P, Milne N. Flattening of the interventricular septum (D-shaped left ventricle) in addition to high right ventricular tracer uptake and increased right ventricular volume found on gated SPECT studies strongly correlates with right ventricular overload. J Nucl Cardiol 2005;12:428-34.
Mannting F, Zabrodina YV, Dass C. Significance of increased right ventricular uptake on 99mTc-sestamibi SPECT in patients with coronary artery disease. J Nucl Med 1999;40:889-94.
Schulman DS, Lazar JM, Ziady G, Grandis DJ, Flores AR, Orie JE. Right ventricular thallium-201 kinetics in pulmonary hypertension: Relation to right ventricular size and function. J Nucl Med 1993;34:1695-700.
Rabinovitch M, Fischer KC, Treves S. Quantitative thallium-201 myocardial imaging in assessing right ventricular pressure in patients with congenital heart defects. Br Heart J 1981;45:198-205.
Reduto LA, Berger HJ, Johnstone DE, et al. Radionuclide assessment of right and left ventricular exercise reserve after total correction of tetralogy of Fallot. Am J Cardiol 1980;45:1013-8.
Nestico PF, Hakki AH, Felsher J, Heo J, Iskandrian AS. Implications of abnormal right ventricular thallium uptake in acute myocardial infarction. Am J Cardiol 1986;58:230-4.
Brunken RC, Perloff JK, Czernin J, et al. Myocardial perfusion reserve in adults with cyanotic congenital heart disease. Am J Physiol Heart Circ Physiol 2005;289:H1798-806.
Schelbert HR, Beanlands R, Bengel F, et al. PET myocardial perfusion and glucose metabolism imaging: Part 2-Guidelines for interpretation and reporting. J Nucl Cardiol 2003;10:557-71.
Chow BJ, Ananthasubramaniam K, dekemp RA, Dalipaj MM, Beanlands RS, Ruddy TD. Comparison of treadmill exercise versus dipyridamole stress with myocardial perfusion imaging using rubidium-82 positron emission tomography. J Am Coll Cardiol 2005;45:1227-34.
Port SC. Imaging guidelines for nuclear cardiology procedures, part 2. American Society of Nuclear Cardiology. J Nucl Cardiol 1999;6:G47-84.
Hachamovitch R, Berman DS, Shaw LJ, et al. Incremental prognostic value of myocardial perfusion single photon emission computed tomography for the prediction of cardiac death: Differential stratification for risk of cardiac death and myocardial infarction. Circulation 1998;97:535-43.
Ostrom MP, Gopal A, Ahmadi N, et al. Mortality incidence and the severity of coronary atherosclerosis assessed by computed tomography angiography. J Am Coll Cardiol 2008;52:1335-43.
Parkash R, dekemp RA, Ruddy TD, et al. Potential utility of rubidium 82 PET quantification in patients with 3-vessel coronary artery disease. J Nucl Cardiol 2004;11:440-9.
Choi Y, Huang SC, Hawkins RA, et al. A simplified method for quantification of myocardial blood flow using nitrogen-13-ammonia and dynamic PET. J Nucl Med 1993;34:488-97.
dekemp RA, Ruddy TD, Hewitt T, Dalipaj MM, Beanlands RS. Detection of serial changes in absolute myocardial perfusion with 82Rb PET. J Nucl Med 2000;41:1426-35.
Gewirtz H, Skopicki HA, Abraham SA, et al. Quantitative PET measurements of regional myocardial blood flow: Observations in humans with ischemic heart disease. Cardiology 1997;88:62-70.
Gould KL, Kirkeeide RL, Buchi M. Coronary flow reserve as a physiologic measure of stenosis severity. J Am Coll Cardiol 1990;15:459-74.
Herrero P, Markham J, Shelton ME, Weinheimer CJ, Bergmann SR. Noninvasive quantification of regional myocardial perfusion with rubidium-82 and positron emission tomography Exploration of a mathematical model. Circulation 1990;82:1377-86.
Hutchins GD, Schwaiger M, Rosenspire KC, Krivokapich J, Schelbert H, Kuhl DE. Noninvasive quantification of regional blood flow in the human heart using N-13 ammonia and dynamic positron emission tomographic imaging. J Am Coll Cardiol 1990;15:1032-42.
Kuhle WG, Porenta G, Huang SC, et al. Quantification of regional myocardial blood flow using 13N-ammonia and reoriented dynamic positron emission tomographic imaging. Circulation 1992;86:1004-17.
Lin JW, Sciacca RR, Chou RL, Laine AF, Bergmann SR. Quantification of myocardial perfusion in human subjects using 82Rb and wavelet-based noise reduction. J Nucl Med 2001;42:201-8.
Nienaber CA, Ratib O, Gambhir SS, et al. A quantitative index of regional blood flow in canine myocardium derived noninvasively with N-13 ammonia and dynamic positron emission tomography. J Am Coll Cardiol 1991;17:260-9.
Scott NS, Le May MR, de Kemp R, et al. Evaluation of myocardial perfusion using rubidium-82 positron emission tomography after myocardial infarction in patients receiving primary stent implantation or thrombolytic therapy. Am J Cardiol 2001;88:886-9. A6.
deKemp RA, Yoshinaga K, Beanlands RS. Will 3-dimensional PET-CT enable the routine quantification of myocardial blood flow? J Nucl Cardiol 2007;14:380-97.
Acknowledgments
The authors extend their gratitude to Quintin Armour, May Aung, Sandina Jamieson, Ann Guo, Kim Gardner, and Matt Raegele for their technical assistance and expertise.
Author information
Authors and Affiliations
Corresponding author
Additional information
Arun Abraham is supported by the Whit and Heather Tucker Research Fellowship. Rob Beanlands is a Career Investigator supported by the Heart and Stroke Foundation of Ontario. Benjamin Chow is supported by CIHR New Investigator Award #MSH-83718, and receives research and fellowship support from GE Healthcare and educational support from TeraRecon Inc.
Rights and permissions
About this article
Cite this article
Abraham, A., Kass, M., Ruddy, T.D. et al. Right and left ventricular uptake with Rb-82 PET myocardial perfusion imaging: Markers of left main or 3 vessel disease. J. Nucl. Cardiol. 17, 52–60 (2010). https://doi.org/10.1007/s12350-009-9153-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-009-9153-2