Abstract
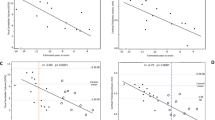
Although the main clinical manifestations of spinocerebellar ataxias (SCAs) result from damage of the cerebellum, other systems may also be involved. Olfactory deficits have been reported in other types of ataxias, especially in SCA3; however, there are no studies on olfactory deficits in SCA type 10 (SCA10). To analyze olfactory function of SCA10 patients compared with that of SCA3, Parkinson’s, and healthy controls. Olfactory identification was tested in three groups of 30 patients (SCA10, SCA3, and Parkinson’s disease (PD)) and 44 healthy controls using the Sniffin’ Sticks (SS16) test. Mean SS16 score was 11.9 ± 2.9 for the SCA10 group, 12.3 ± 1.9 for the SCA3 group, 6.6 ± 2.8 for the PD group, and 12.1 ± 2.0 for the control group. Mean SS16 score for the SCA10 group was not significantly different from the scores for the SCA3 and control groups but was significantly higher than the score for the PD group (p < 0.001) when adjusted for age, gender, and history of smoking. There was no association between SS16 scores and disease duration in the SCA10 or SCA3 groups or number of repeat expansions. SS16 and Mini Mental State Examination scores were correlated in the three groups: SCA10 group (r = 0.59, p = 0.001), SCA3 group (r = 0.50, p = 0.005), and control group (r = 0.40, p = 0.007). We found no significant olfactory deficits in SCA10 in this large series.

Similar content being viewed by others
References
Teive HAG, Ashizawa T. Primary and secondary ataxias. Curr Opin Neurol. 2015;28(4):413–22.
Matsuura T, Ashizawa T. Spinocerebellar ataxia type 10: a disease caused by a large ATTCT repeat expansion. Adv Exp Med Biol. 2002a;516:79–97.
Matsuura T, Ashizawa T. Polymerase chain reaction amplification of expanded ATTCT repeat in spinocerebellar ataxia type 10. Ann Neurol. 2002b;51(2):271–2.
Teive HAG, Roa BB, Raskin S, Fang P, Arruda WO, Neto YC, et al. Clinical phenotype of Brazilian families with spinocerebellar ataxia 10. Neurology. 2004;63(8):1509–12.
Moscovich M, Munhoz RP, Teive HA, Raskin S, Carvalho M de J, Barbosa ER, et al. Olfactory impairment in familial ataxias. J Neurol Neurosurg Psychiatry. 2012;83(10):970–4.
Moro A, Munhoz RP, Moscovich M, Arruda WO, Raskin S, Silveira-Moriyama L, et al. Nonmotor symptoms in patients with spinocerebellar ataxia type 10. Cerebellum. 2017;16(5–6):938–44.
Teive HA, Munhoz RP, Raskin S, Arruda WO, de Paola L, Werneck LC, et al. Spinocerebellar ataxia type 10: frequency of epilepsy in a large sample of Brazilian patients. Mov Disord. 2010;25(16):2875–8.
Moro A, Munhoz RP, Arruda WO, Raskin S, Moscovich M, Teive HA. Spinocerebellar ataxia type 3: subphenotypes in a cohort of Brazilian patients. Arq Neuropsiquiatr. 2014;72(9):659–62.
Paulson H. Machado-Joseph disease/spinocerebellar ataxia type 3. Handb Clin Neurol. 2012;103:437–49.
Ahlskog JE, Waring SC, Petersen RC, Esteban-Santillan C, Craig UK, O'Brien PC, et al. Olfactory dysfunction in Guamanian ALS, parkinsonism, and dementia. Neurology. 1998;51(6):1672–7.
Mesholam RI, Moberg PJ, Mahr RN, Doty RL. Olfaction in neurodegenerative disease: a meta-analysis of olfactory functioning in Alzheimer’s and Parkinson’s diseases. Arch Neurol. 1998;55(1):84–90.
Silveira-Moriyama L, Guedes LC, Kingsbury A, Ayling H, Shaw K, Barbosa ER, et al. Hyposmia in G2019S LRRK2-related parkinsonism: clinical and pathologic data. Neurology. 2008;71(13):1021–6.
Braga-Neto P, Felicio AC, Pedroso JL, Dutra LA, Bertolucci PH, Gabbai AA, et al. Clinical correlates of olfactory dysfunction in spinocerebellar ataxia type 3. Parkinsonism Relat Disord. 2011;17(5):353–6.
Velazquez-Perez L, Fernandez-Ruiz J, Diaz R, Gonzalez RP, Ochoa NC, Cruz GS, et al. Spinocerebellar ataxia type 2 olfactory impairment shows a pattern similar to other major neurodegenerative diseases. J Neurol. 2006;253(9):1165–9.
Fernandez-Ruiz J, Diaz R, Hall-Haro C, Vergara P, Fiorentini A, Nunez L, et al. Olfactory dysfunction in hereditary ataxia and basal ganglia disorders. Neuroreport. 2003;14(10):1339–41.
Galvez V, Diaz R, Hernandez-Castillo CR, Campos-Romo A, Fernandez-Ruiz J. Olfactory performance in spinocerebellar ataxia type 7 patients. Parkinsonism Relat Disord. 2014;20(5):499–502.
Connelly T, Farmer JM, Lynch DR, Doty RL. Olfactory dysfunction in degenerative ataxias. J Neurol Neurosurg Psychiatry. 2003;74(10):1435–7.
Houlden H. Sniffing out the cerebellum. J Neurol Neurosurg Psychiatry. 2012;83(10):952–3.
Brucki SM, Nitrini R, Caramelli P, Bertolucci PH, Okamoto IH. Suggestions for utilization of the mini-mental state examination in Brazil. Arq Neuropsiquiatr. 2003;61(3B):777–81.
Teive HA, Munhoz RP, Arruda WO, Raskin S, Werneck LC, Ashizawa T. Spinocerebellar ataxia type 10—a review. Parkinsonism Relat Disord. 2011;17(9):655–61.
Teive HA, Munhoz RP, Raskin S, Werneck LC. Spinocerebellar ataxia type 6 in Brazil. Arq Neuropsiquiatr. 2008;66(3B):691–4.
Hughes AJ, Daniel SE, Kilford L, Lees AJ. Accuracy of clinical diagnosis of idiopathic Parkinson’s disease: a clinico-pathological study of 100 cases. J Neurol Neurosurg Psychiatry. 1992;55(3):181–4.
Kobal G, Hummel T, Sekinger B, Barz S, Roscher S, Wolf S. “Sniffin’ sticks”: screening of olfactory performance. Rhinology. 1996;34(4):222–6.
Schmitz-Hubsch T, du Montcel ST, Baliko L, Berciano J, Boesch S, Depondt C, et al. Scale for the assessment and rating of ataxia: development of a new clinical scale. Neurology. 2006;66(11):1717–20.
Subramony SH. SARA—a new clinical scale for the assessment and rating of ataxia. Nat Clin Pract Neurol. 2007;3(3):136–7.
Abele M, Riet A, Hummel T, Klockgether T, Wullner U. Olfactory dysfunction in cerebellar ataxia and multiple system atrophy. J Neurol. 2003;250(12):1453–5.
Hawkes C. Olfaction in neurodegenerative disorder. J Mov Disord. 2003;18(4):364–72.
Silveira-Moriyama L, Azevedo AM, Ranvaud R, Barbosa ER, Doty RL, Lees AJ. Applying a new version of the Brazilian-Portuguese UPSIT smell test in Brazil. Arq Neuropsiquiatr. 2010a;68(5):700–5.
Morley JF, Weintraub D, Mamikonyan E, Moberg PJ, Siderowf AD, Duda JE. Olfactory dysfunction is associated with neuropsychiatric manifestations in Parkinson’s disease. Movement disorders. J Mov Disord. 2011;26(11):2051–7.
Silveira-Moriyama L, Hughes G, Church A, Ayling H, Williams DR, Petrie A, et al. Hyposmia in progressive supranuclear palsy. J Mov Disord 2010b;25(5):570–7.
Kovacs T. Mechanisms of olfactory dysfunction in aging and neurodegenerative disorders. Ageing Res Rev. 2004;3(2):215–32.
Hummel T, Kobal G. Differences in human evoked potentials related to olfactory or trigeminal chemosensory activation. Electroencephalogr Clin Neurophysiol. 1992;84(1):84–9.
Savic I. Brain imaging studies of the functional organization of human olfaction. Neuroscientist. 2002;8(3):204–11.
Yousem DM, Williams SC, Howard RO, Andrew C, Simmons A, Allin M, et al. Functional MR imaging during odor stimulation: preliminary data. Radiology. 1997;204(3):833–8.
Savic I, Gulyas B, Berglund H. Odorant differentiated pattern of cerebral activation: comparison of acetone and vanillin. Hum Brain Mapp. 2002;17(1):17–27.
Qureshy A, Kawashima R, Imran MB, Sugiura M, Goto R, Okada K, et al. Functional mapping of human brain in olfactory processing: a PET study. J Neurophysiol. 2000;84(3):1656–66.
Author information
Authors and Affiliations
Contributions
M Moscovich conceptualized the study, analyzed the data in the study, drafted the manuscript, and revised the manuscript. R P Munhoz drafted the manuscript and revised the manuscript. H A Teive designed the study and revised the manuscript. S Raskin revised the manuscript. A Moro revised the manuscript. K McFarland revised the manuscript. T Ashizawa revised the manuscript. L Silveira-Moriyama designed the study, interpreted the data in the study, analyzed the data in the study, drafted the manuscript, and revised the manuscript.
Corresponding author
Ethics declarations
Informed consent was obtained from all participants, and the protocol was approved by the local (UFPR) ethics committee.
Conflict of Interest
Dr. Moscovich, Dr. Munhoz, Dr. Moro, Dr. Raskin, and Dr. McFarland report no disclosure. Dr. Ashizawa is funded by NIH grant NS083564. Teive received personal compensation for educational activities with Allergan, Ipsen, Teva, and UCB and serves as an editor-in-chief of Arquivos de Neuro-Psiquiatria and editorial board member of Movement Disorder Clinical Practice, the Journal of Neurology Research, Parkinson’s Disease, Current Neurology and Neuroscience Reports, and Arquivos de Neuropsiquiatria. Dr. Laura Silveira-Moriyama received travel grants from Teva and supervised scholarships from Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP) and Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES).
Rights and permissions
About this article
Cite this article
Moscovich, M., Munhoz, R.P., Moro, A. et al. Olfactory Function in SCA10. Cerebellum 18, 85–90 (2019). https://doi.org/10.1007/s12311-018-0954-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12311-018-0954-1