Abstract
Background
We hypothesized that transfer of the olecranon tip for simulated type III coronoid fracture would restore posterior ulnohumeral translation to a level not different from that in the intact state.
Methods
The collateral ligaments were left intact in 12 fresh-frozen cadaveric elbows, and all other soft tissues were removed. The entire coronoid process was osteotomized flush with the ventral aspect of the ulna and was reconstructed using the tip of the olecranon process. Specimens were tested with an axial load of 100 N at 0.25 mm/s in 15° increments from 15 to 120° of flexion. Intact, osteotomized, and reconstructed posterior ulnohumeral displacement was measured.
Results
The bony reconstruction did not obstruct range of motion of the elbow. Intact translation (mean ± SD) ranged from 0.3 ± 0.1 to 1.1 ± 0.6 mm, and translation in the osteotomized state ranged from 1.3 ± 1.0 to 2.0 ± 1.0 mm. Resection of the coronoid resulted in a significant increase in posterior ulnar translation compared with intact at all flexion angles (p < 0.05) except at 75°. Reconstruction decreased translation versus the osteotomized state at all flexion angles, significantly at 60 and 120°. No significant difference in translation was found between reconstructed and intact states at five of eight positions tested.
Conclusions
In this biomechanical study of irreparable coronoid fracture, autograft olecranon tip transfer restored posterior elbow stability to a level not significantly different from the intact elbow in five of eight elbow positions tested.
Similar content being viewed by others
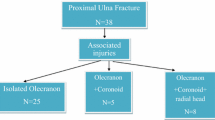
Introduction
The coronoid is crucial for elbow stability [3, 8]. Biomechanical studies have shown that this structure prevents posterior ulnar subluxation and resists posteromedial and posterolateral rotatory forces [1, 3, 14]. Fractures of the coronoid process are commonly associated with elbow dislocation and radial head fracture in terrible triad injury of the elbow. In biomechanical studies, repair of type II and III [11] coronoid fractures has been shown to be critical in restoring elbow stability after this injury [3, 10].
Few repair options exist in coronoid fractures where the coronoid process is extensively comminuted. The anterior capsule of the elbow can be sutured to the coronoid fragments to help restore stability [9], but this soft tissue repair is inherently less stable than the bony constraint provided by the native coronoid and often limits elbow extension [5, 13]. Use of structural allograft and radial head allograft for coronoid reconstruction has shown mixed results [16]. A procedure in which the tip of the olecranon is transferred to replace the missing coronoid [6] could offer the advantage of an osteochondral autograft anatomically similar to the coronoid with minimal donor site morbidity. We are not aware of any studies that have evaluated the biomechanical effect of this procedure on elbow stability. We evaluated the effect of olecranon tip transfer on posterior ulnar translation in a cadaver model of type III coronoid fracture. We hypothesized that this procedure would restore elbow stability to a level not different from that of the intact specimen.
Materials and Methods
We tested 12 fresh-frozen cadaveric elbows in this study. Average age was 82 years (range, 71–92), and sex was two females and ten males. We thawed specimens at room temperature for 12 h before testing. We removed skin and all subcutaneous soft tissues including the musculature about the elbow and took great care in preserving the integrity of the joint capsule and all of the collateral ligaments. The humerus was transected at the midshaft and the forearm 15 cm distal to the elbow joint. We placed a Steinmann pin between the radius and ulna distally to lock the forearm in neutral rotation and potted the specimens using polyester resin (Bondo, 3M, St. Paul, MN).
We used a custom jig to administer posterior loading of the ulnohumeral joint within an arc of 0 to 120° (Fig. 1). Once mounted in the custom jig, the specimen was secured on an electromechanical load frame (MTS Systems, Inc., Eden Prairie, MN). The load was 0.25 mm/s until a load of 100 N was obtained. This rate was used to simulate mild physiologic strain in the collateral ligaments [3, 12, 18]. Posterior ulnar translation was measured using load frame crosshead displacement in a manner similar to that described previously [3].
We measured posterior ulnar translation at 15° intervals of ulnohumeral flexion from 15 to 120°. We did not test specimens at 0° because some specimens had slight flexion contractures. A total of ten loading cycles were done at each flexion position, and average displacement was used in the analysis.
Once the intact specimens were tested, we used a microsagittal saw to resect the coronoid flush with the ventral aspect of the ulna [11]. The level of the cut was determined by drawing an imaginary line along the anterior cortex of the ulna, corresponding with the ventral aspect of the ulna (Fig. 2). The bone was resected using a microsagittal saw. We confirmed the level of resection fluoroscopically in multiple planes (Fig. 3). After resection of the coronoid, the specimens were similarly secured in the load frame and loaded as described above.
Pilot specimens were used to determine the size of olecranon tip that would be required to replace the resected coronoid process. We determined that cutting the tip of olecranon using the line used to resect the coronoid as a guide for the exit of our cut would yield an olecranon tip fragment of similar dimensions to the resected coronoid (Figs. 3 and 4). To achieve this, we extended the line that we used to cut the coronoid through the joint until it intersected the olecranon. This was determined to be the exit point of the olecranon cut. We resected the tip of the olecranon with a 10-mm microsagittal saw at a 15° anterosuperior tilt to avoid taking articular cartilage from the ulna. Care was also taken avoid violating the articular cartilage of the posterior humerus. The size of the olecranon fragment varied depending on specimen size, but the typical resection was approximately 8 mm or approximately 50 % of the olecranon. The olecranon tip in this model did not have any substantial triceps attachment.
After harvesting, the olecranon graft was flipped for placement on the coronoid to ensure a continuous osteochondral articular surface. The graft was fashioned for a precise contoured fit. The olecranon is slightly wider than the coronoid in its medial-to-lateral dimension, and therefore, approximately 3 mm of the lateral graft was resected to prevent impingement of the graft into the proximal radioulnar joint. Once appropriate positioning was achieved, the graft was secured to the coronoid with clamps and a guide wire for a 4.0-mm cannulated screw was used to secure the fragments. Precise alignment of the graft was confirmed via fluoroscopy. A 4.0-mm cannulated screw of adequate length to secure the graft was then placed using a lag screw technique (Fig. 5). Anteroposterior fixation was used because compression or lag fixation in this setting is readily accomplished clinically under direct visualization. Fluoroscopy was used to confirm anatomic positioning of the olecranon graft, appropriate screw trajectory, and good apposition of the bone fragments (Fig. 6).
After reconstruction, specimens were taken through range of motion to make sure that there was a smooth arc free from impingement by the graft. Specimens were then mounted on the testing jig and loaded as for the previous stages (Fig. 7).
Statistical Analysis
Power analysis based on three groups with standard deviation of 0.24 found that 12 specimens per group at 15° of elbow flexion would have 90 % power to identify a significant difference in posterior ulnar translation (effect size, 0.39) at the p = 0.05 level if such a difference existed.
Data were analyzed with repeated measures analysis of variance with Tukey post hoc test if significant difference was found. A p value of ≤0.05 was considered significant.
Results
The olecranon graft provided a continuous osteochondral articular surface in all specimens, and the bony reconstruction did not obstruct range of motion of the elbow in any specimens before loading. Intact posterior ulnar translation (mean ± SD) ranged from 0.3 ± 0.1 to 1.2 ± 0.6 mm, and translation in the osteotomized state ranged from 1.3 ± 1.0 to 2.0 ± 1.0 mm (Table 1).
Resection of the coronoid resulted in a significant increase in posterior ulnohumeral translation compared with intact at all flexion angles except 75° (Table 1). Reconstruction improved translation versus the osteotomized state to some extent at all flexion angles, significantly at 60 and 120° of flexion. Reconstruction decreased translation to a level not different from the intact state at 15, 45, 60, 90, and 120° of flexion. During testing, there was no visual evidence of any gross graft displacement or rotation.
Discussion
In this biomechanical study of irreparable coronoid fracture, autograft olecranon tip transfer restored posterior elbow stability to a level not significantly different from the intact elbow in five of eight elbow positions tested. These findings suggest that olecranon tip transfer offers biomechanical qualities conducive to elbow stability in type III coronoid fractures where repair is not possible because of the size of the fragment or the amount of comminution.
Our results support those of previous biomechanical studies that have tested elbow instability with coronoid fracture [3, 4]. Closkey et al. [3] observed posterior ulnohumeral displacement of up to 2.4 mm after type III coronoid fractures. King et al. [4] found that rebuilding the coronoid with a metallic prosthesis can return varus-valgus stability to the elbow. Their results suggested that stability can be returned to the elbow by replacing the coronoid, whether it is with a prosthesis or with an autograft, as our study shows.
Our study evaluated isolated coronoid fracture to control for all other factors contributing to elbow instability, such as the collateral ligaments and joint capsule. We kept the collateral ligaments and all other osseous structures intact to isolate the effect of this procedure on the instability caused by coronoid fracture. This method allowed us to directly measure the effect of olecranon tip transfer on posterior ulnar translation. In vivo, these injuries seldom occur in isolation but rather are seen in association with terrible triad injuries where multiple ligaments and osseous structures have been violated, yielding several sources of instability [15]. This biomechanical study is thus narrowly focused on only one aspect of a complex treatment scenario.
The olecranon tip may offer advantages as a graft option for unreconstructable coronoid fractures. The olecranon is local to the surgical site and thus decreases concerns for donor site morbidity at a different site, such as in iliac crest harvest [7]. The use of osteochondral autograft olecranon graft offers the theoretical advantage of reduced potential for posttraumatic arthritis. The approximately 50 % resection of the olecranon used in this study is well below the 87 % level of olecranon resection associated with gross instability of the elbow [2]. The procedure is relatively simple with low cost in that only a single cannulated screw is required. We found that the graft can be fashioned to be almost identical to the coronoid fragment for a close anatomic fit similar to that observed in hemihamate arthroplasty for unreconstructable phalangeal base fractures [17]. The lack of substantial triceps attachment in this model should allow for harvesting while preserving the triceps, and compression or lag fixation from anterior to posterior is readily accomplished under direct visualization.
Use of the olecranon tip for coronoid reconstruction may also offer other advantages over use of radial head or iliac crest graft. Radial head graft is nonanatomic and does not incorporate cartilage, and iliac crest graft is not osteochondral bone. In a recent study, one of six patients in whom an osteoarticular radial head fragment was used for coronoid reconstruction in terrible triad injury had complete resorption of the graft and severe osteoarthritis at 54 months [16]. Mayo Elbow Performance Scores were one excellent, two good, one fair, and two poor. The use of iliac crest bone graft for coronoid reconstruction in terrible triad injury resulted in good clinical results at 1 year with limited range of motion from 45 to 120° and a Morrey score of 94 [5]. Moritomo et al. reported on use of an olecranon tip autograft for coronoid reconstruction in two patients with chronic elbow instability after terrible triad injury [6]. One patient had range of motion of 25–120° at 1 year without recurrent instability, and the second had similar range of motion and no limitations in activities of daily living at 5 years without evidence of arthritis or graft resorption. Although not seen in these two cases, resorption of the graft is a potential concern after this procedure. We believe that the risk of resorption with olecranon tip graft may be mitigated by the fact that this is an autologous graft. However, larger clinical series will be required to assess this risk. Although clinical evidence for this procedure is limited, our findings suggest that osteochondral olecranon graft provides biomechanical stability in treatment of irreparable coronoid fractures.
There are several limitations to our study. This biomechanical study was based on a model of an isolated coronoid fracture and does not replicate terrible triad injury with collateral ligament and radial head injury. Our study design did not allow definitive determination of the reason for continued statistical difference in displacement between the reconstructed and intact specimens at 30 and 105°, but we believe that it is reasonable to assume normal variation among the specimens played a role. We tested only posterior displacement of the elbow. Several studies have shown that coronoid fractures also can affect varus and valgus instability of the elbow [4]. A future direction of this study is to develop a multidimensional testing construct that would allow us to test ulnohumeral displacement in all planes. However, the current study design allowed us to isolate a critical component of stability in the elbow after type III coronoid fracture.
In this biomechanical study of irreparable coronoid fracture, autograft olecranon tip transfer restored posterior elbow stability to a level not significantly different from the intact elbow in five of eight elbow positions tested.
References
Beingessner DM, Stacpoole RA, Dunning CE, et al. The effect of suture fixation of type I coronoid fractures on the kinematics and stability of the elbow with and without medial collateral ligament repair. J Shoulder Elb Surg. 2007;16:213–7.
Bell TH, Ferreira LM, McDonald CP, et al. Contribution of the olecranon to elbow stability: an in vitro biomechanical study. J Bone Joint Surg Am. 2010;92:949–57.
Closkey RF, Goode JR, Kirschenbaum D, et al. The role of the coronoid process in elbow stability. A biomechanical analysis of axial loading. J Bone Joint Surg Am. 2000;82-A:1749–53.
Gray AB, Alolabi B, Ferreira LM, et al. The effect of a coronoid prosthesis on restoring stability to the coronoid-deficient elbow: a biomechanical study. J Hand Surg [Am]. 2013;38:1753–61.
Kohls-Gatzoulis J, Tsiridis E, Schizas C. Reconstruction of the coronoid process with iliac crest bone graft. J Shoulder Elb Surg. 2004;13:217–20.
Moritomo H, Tada K, Yoshida T, et al. Reconstruction of the coronoid for chronic dislocation of the elbow. Use of a graft from the olecranon in two cases. J Bone Joint Surg (Br). 1998;80:490–2.
Myeroff C, Archdeacon M. Autogenous bone graft: donor sites and techniques. J Bone Joint Surg Am. 2011;93:2227–36.
O’Driscoll SW. Classification and evaluation of recurrent instability of the elbow. Clin Orthop Relat Res. 2000;370:34–43.
O’Driscoll SW, Jupiter JB, Cohen MS, et al. Difficult elbow fractures: pearls and pitfalls. Instr Course Lect. 2003;52:113–34.
Pollock JW, Pichora J, Brownhill J, et al. The influence of type II coronoid fractures, collateral ligament injuries, and surgical repair on the kinematics and stability of the elbow: an in vitro biomechanical study. J Shoulder Elb Surg. 2009;18:408–17.
Regan W, Morrey B. Fractures of the coronoid process of the ulna. J Bone Joint Surg Am. 1989;71:1348–54.
Regan WD, Korinek SL, Morrey BF, et al. Biomechanical study of ligaments around the elbow joint. Clin Orthop. 1991;271:170–9.
Regan WD, Morrey BF. Coronoid process and Moteggia fractures. In: Morrey BF, Sanchez-Sotelo J, editors. The elbow and its disorders. 4th ed. Philadelphia: Saunders Elsevier; 2009. p. 419–35.
Schneeberger AG, Sadowski MM, Jacob HA. Coronoid process and radial head as posterolateral rotatory stabilizers of the elbow. J Bone Joint Surg Am. 2004;86-A:975–82.
Steinmann SP. Coronoid process fracture. J Am Acad Orthop Surg. 2008;16:519–29.
Van Riet RP, Morrey BF, O’Driscoll SW. Use of osteochondral bone graft in coronoid fractures. J Shoulder Elb Surg. 2005;14:519–23.
Williams RM, Kiefhaber TR, Sommerkamp TG, et al. Treatment of unstable dorsal proximal interphalangeal fracture/dislocations using a hemi-hamate autograft. J Hand Surg [Am]. 2003;28:856–65.
Woo SL, Peterson RH, Ohland KJ, et al. The effects of strain rate on the properties of the medial collateral ligament in skeletally immature and mature rabbits: a biomechanical and histological study. J Orthop Res. 1990;8:712–21.
Acknowledgments
We thank Lyn Camire, MA, ELS, of our department for editorial assistance.
Conflict of Interest
Miguel A Ramirez declares that he has no conflict of interest.
Jose M. Ramirez declares that he has no conflict of interest.
Brent G. Parks declares that he has no conflict of interest.
Michael A. Tsai declares that he has no conflict of interest.
Anand M. Murthi declares that he has no conflict of interest.
Statement of Human and Animal Rights
This study does not involve live human or animal subjects.
Statement of Informed Consent
Informed consent is not applicable to this study.
Funding
None. There was no external source of funding for this project.
Disclaimer
None.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Ramirez, M.A., Ramirez, J.M., Parks, B.G. et al. Olecranon tip osteoarticular autograft transfer for irreparable coronoid process fracture: a biomechanical study. HAND 10, 695–700 (2015). https://doi.org/10.1007/s11552-015-9776-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11552-015-9776-5