Abstract
The pituitary gland and the hypothalamus can be affected by autoimmune-mediated structural and functional disruption. These autoimmune-mediated diseases occur more commonly in females and are often found during pregnancy or in the post-partum period. Autoimmune diseases can either affect parts of the pituitary or hypothalamus, or can involve both sellar and suprasellar structures. Most of these cases comprise primary hypophysitis (PRH). Over the years, there has been a tremendous increase in the number of reported PRH cases and related disorders, including hypophysitis induced by immune checkpoint inhibitors. With this increasing data, more light is being shed on the spectrum of clinical presentations, biochemical and imaging abnormalities of these disorders. Regardless, these disorders are still relatively rare. The clinical presentation can vary vastly, based on the type of pituitary cell or the area of the suprasellar region affected. The severity can range from clinically silent disease to progressive and rapid deterioration and death, likely due to unrecognized central adrenal insufficiency. Although biopsy remains a gold standard for diagnosing these disorders, the current standard of practice is biochemical assessment for hormonal deficiencies and imaging studies. In several instances, these disorders spontaneously resolve, but medical or surgical intervention might be necessary to treat symptomatic disease. Due to the subtlety and a vast spectrum of clinical manifestations which could often be asymptomatic, and the rarity of the occurrence of these diseases in clinical practice, the diagnosis can be easily missed which could potentially lead to substantial morbidity or mortality. Therefore, it is crucial to have a strong clinical suspicion and pursue timely biochemical and imaging studies to initiate prompt treatment. In this article, we review the various autoimmune conditions that affect the sellar and suprasellar structures, their diagnostic approach and management of these disorders.



Similar content being viewed by others
Abbreviations
- LAH:
-
Lymphocytic adenohypophysitis
- LINH:
-
Lymphocytic infundibuloneurohypophysitis
- LPH:
-
Lymphocytic panhypophysitis
- PRH:
-
Primary hypophysitis
- GRH:
-
Granulomatous hypophysitis
- XH:
-
Xanthomatous hypophysitis
- NH:
-
Necrotizing hypophysitis
- IgG4H:
-
IgG4 mediated hypophysitis
References
Caturegli P, Lupi I, Landek-Salgado M, Kimura H, Rose NR. Pituitary autoimmunity: 30 years later. Autoimmun Rev. 2008;7(8):631–7.
Goudie R, Pinkerton P. Anterior hypophysitis and Hashimoto's disease in a young woman. J Pathol Bacteriol. 1962;83(2):584–5.
Rupp J, Paschkis KE. Panhypopituitarism and hypocalcemic tetany in a male: case presentation. Ann Intern Med. 1953;39(5):1103–6.
Chung T-T, Koch CA, Monson JP. Hypopituitarism. In: De Groot LJ, Chrousos G, Dungan K, Feingold KR, Grossman A, Hershman JM, Koch C, Korbonits M, McLachlan R, New M, Purnell J, Rebar R, Singer F, Vinik A, editors. Endotext [Internet]. South Dartmouth: MDText.com, Inc.; 2000. 2018 Jul 25 https://www.ncbi.nlm.nih.gov/pubmed/25905222.
Ferrari SM, Fallahi P, Galetta F, Citi E, Benvenga S, Antonelli A. Thyroid disorders induced by checkpoint inhibitors. Rev Endocr Metab Disord. 2018:1–9.
Melcescu E, Hogan IIRB, Brown K, Boyd SA, Abell TL, Koch CA. The various faces of autoimmune endocrinopathies: non-tumoral hypergastrinemia in a patient with lymphocytic colitis and chronic autoimmune gastritis. Exp Mol Pathol. 2012;93(3):434–40.
Melcescu E, Kemp E, Majithia V, Vijayakumar V, Uwaifo G, Koch C. Graves' disease, hypoparathyroidism, systemic lupus erythematosus, alopecia, and angioedema: autoimmune polyglandular syndrome variant or coincidence? Int J Immunopathol Pharmacol. 2013;26(1):217–22.
Witebsky E, Rose NR, Terplan K, Paine JR, Egan RW. Chronic thyroiditis and autoimmunization. J Am Med Assoc. 1957;164(13):1439–47.
Yantorno C, Debanne MT, Vottero-Cima E. Autoimmune orchitis induced by autoimmunization with seminal plasma in the rabbit. J Reprod Fertil. 1971;27(3):311–20.
Colover J, Glynn L. Experimental iso-immune adrenalitis. Immunology. 1958;1(2):172.
Caturegli P, Di Dalmazi G, Lombardi M, Grosso F, Larman HB, Larman T, et al. Hypophysitis secondary to cytotoxic T-lymphocyte–associated protein 4 blockade: insights into pathogenesis from an autopsy series. Am J Pathol. 2016;186(12):3225–35.
Caturegli P, Newschaffer C, Olivi A, Pomper MG, Burger PC, Rose NR. Autoimmune hypophysitis. Endocr Rev. 2005;26(5):599–614.
Bayram F, Keleştimur F, Öztürk F, Selcuklu A, Patiroğlu T, Beyhan Z. Lymphocytic hypophysitis in a patient with Graves’ disease. J Endocrinol Investig. 1998;21(3):193–7.
Bellastella G, Maiorino MI, Bizzarro A, Giugliano D, Esposito K, Bellastella A, et al. Revisitation of autoimmune hypophysitis: knowledge and uncertainties on pathophysiological and clinical aspects. Pituitary. 2016;19(6):625–42.
Hussain S, Shahriar HM, Drake W, editors. Lymphocytic hypophysitis in a pregnant patient with type 1 diabetes. Society for Endocrinology Endocrine Update 2018; 2018: BioScientifica.
Gonzalez J, Diez A, Prieto A, Fernandez M, editors. Lymphocytic hypophysitis which underwent surgery despite the absence of compression of nearby structures. A case report. 19th European Congress of Endocrinology; 2017: BioScientifica.
Wang S, Wang L, Yao Y, Feng F, Yang H, Liang Z, et al. Primary lymphocytic hypophysitis: clinical characteristics and treatment of 50 cases in a single Centre in China over 18 years. Clin Endocrinol. 2017;87(2):177–84.
Angelousi A, Cohen C, Sosa S, Danilowicz K, Papanastasiou L, Tsoli M, et al. Clinical, endocrine and imaging characteristics of patients with primary hypophysitis. Horm Metab Res. 2018;50(04):296–302.
Chiloiro S, Tartaglione T, Angelini F, Bianchi A, Arena V, Giampietro A, et al. An overview of diagnosis of primary autoimmune hypophysitis in a prospective single-center experience. Neuroendocrinology. 2017;104(3):280–90.
Bellastella A, Bizzarro A, Coronella C, Bellastella G, Sinisi AA, De Bellis A. Lymphocytic hypophysitis: a rare or underestimated disease? Eur J Endocrinol. 2003;149(5):363–76.
Fehn M, Sommer C, Lüdecke DK, Plöckinger U, Saeger W. Lymphocytic hypophysitis: light and electron microscopic findings and correlation to clinical appearance. Endocr Pathol. 1998;9(1):71–8.
Falorni A, Minarelli V, Bartoloni E, Alunno A, Gerli R. Diagnosis and classification of autoimmune hypophysitis. Autoimmun Rev. 2014;13(4–5):412–6.
Simmonds M. Über das Vorkommen von Riesenzellen in der Hypophyse. Virchows Archiv für pathologische Anatomie und Physiologie und für klinische Medizin. 1917;223(3):281–90.
Cosman F, Post KD, Holub D, Wardlaw S. Lymphocytic hypophysitis. Medicine. 1989;68(4):240.
Guay AT, Agnello V, Tronic BC, Gresham DG, Freidberg SR. Lymphocytic hypophysitis in a man. J Clin Endocrinol Metabol. 1987;64(3):631–4.
Nussbaum CE, Okawara S-H, Jacobs LS. Lymphocytic hypophysitis with involvement of the cavernous sinus and hypothalamus. Neurosurgery. 1991;28(3):440–4.
Supler ML, Mickle JP. Lymphocytic hypophysitis: report of a case in a man with cavernous sinus involvement. Surg Neurol. 1992;37(6):472–6.
Lee JH, Laws ER Jr, Guthrie BL, Dina TS, Nochomovitz LE. Lymphocytic hypophysitis: occurrence in two men. Neurosurgery. 1994;34(1):159–62.
Quencer RM. Lymphocytic adenohypophysitis: autoimmune disorder of the pituitary gland. Am J Neuroradiol. 1980;1(4):343–5.
Saito T, Yoshida S, Nakao K, Takanashi R. Chronic hypernatremia associated with inflammation of the neurohypophysis. J Clin Endocrinol Metabol. 1970;31(4):391–6.
Brown T, Dhillon S, Chung B, Richfield E, Lubitz S. Lymphocytic hypophysitis in the elderly: a case presentation and review of the literature. Interdiscip Neurosurg. 2017;8:43–9.
Chandan JS, Gittoes N, Toogood A, Karavitaki N, editors. Recurrent lymphocytic hypophysitis during two pregnancies: a very rare care. Society for Endocrinology BES 2017; 2017: BioScientifica.
Imber BS, Lee HS, Kunwar S, Blevins LS, Aghi MK. Hypophysitis: a single-center case series. Pituitary. 2015;18(5):630–41.
Leung GK, Lopes M-BS, Thorner MO, Vance ML, Laws ER. Primary hypophysitis: a single-center experience in 16 cases. J Neurosurg. 2004;101(2):262–71.
Buxton N, Robertson I. Lymphocytic and granulocytic hypophysitis: a single centre experience. Br J Neurosurg. 2001;15(3):242–6.
Cheung CC, Ezzat S, Smyth HS, Asa SL. The spectrum and significance of primary hypophysitis. J Clin Endocrinol Metabol. 2001;86(3):1048–53.
Rumana M, Kirmani A, Khursheed N, Besina S, Khalil M. Lymphocytic hypophysitis with normal pituitary function mimicking a pituitary adenoma: a case report and review of literature. Clin Neuropathol. 2010;29(1):26–31.
Kalra AA, Riel-Romero RMS, Gonzalez-Toledo E. Lymphocytic hypophysitis in children: a novel presentation and literature review. J Child Neurol. 2011;26(1):87–94.
Sellayah R, Gonzales M, Fourlanos S, King J. Lymphocytic hypophysitis in the elderly. J Clin Neurosci. 2015;22(11):1842–3.
Tsur A, Leibowitz G, Samueloff A, Gross DJ. Successful pregnancy in a patient with preexisting lymphocytic hypophysitis. Acta Obstet Gynecol Scand. 1996;75(8):772–4.
Hayes F, McKenna T. The occurrence of lymphocytic hypophysitis in a first but not subsequent pregnancy. J Clin Endocrinol Metabol. 1996;81(8):3131–2.
Gagneja H, Arafah B, Taylor HC. Histologically proven lymphocytic hypophysitis: spontaneous resolution and subsequent pregnancy. Mayo Clin Proc. 1999;74(2):150-4.
Sautner D, Saeger W, Lüdecke DK, Jansen V, Puchner MJ. Hypophysitis in surgical and autoptical specimens. Acta Neuropathol. 1995;90(6):637–44.
Lupi I, Zhang J, Gutenberg A, Landek-Salgado M, Tzou S-C, Mori S, et al. From pituitary expansion to empty sella: disease progression in a mouse model of autoimmune hypophysitis. Endocrinology. 2011;152(11):4190–8.
Karaca Z, Tanriverdi F, Unluhizarci K, Kelestimur F, Donmez H. Empty sella may be the final outcome in lymphocytic hypophysitis. Endocr Res. 2009;34(1–2):10–7.
Heaney AP, Sumerel B, Rajalingam R, Bergsneider M, Yong WH, Liau LM. HLA markers DQ8 and DR53 are associated with lymphocytic hypophysitis and may aid in differential diagnosis. J Clin Endocrinol Metabol. 2015;100(11):4092–7.
Thodou E, Asa SL, Kontogeorgos G, Kovacs K, Horvath E, Ezzat S. Clinical case seminar: lymphocytic hypophysitis: clinicopathological findings. J Clin Endocrinol Metabol. 1995;80(8):2302–11.
Pekic S, Bogosavljevic V, Peker S, Doknic M, Miljic D, Stojanovic M, et al. Lymphocytic Hypophysitis successfully treated with stereotactic radiosurgery: case report and review of the literature. Journal of neurological surgery part a. Cen Eur Neurosurg. 2018;79(01):077–85.
Tubridy N, Saunders D, Thom M, Asa S, Powell M, Plant G, et al. Infundibulohypophysitis in a man presenting with diabetes insipidus and cavernous sinus involvement. J Neurol Neurosurg Psychiatry. 2001;71(6):798–801.
Khare S, Jagtap VS, Budyal SR, Kasaliwal R, Kakade HR, Bukan A, et al. Primary (autoimmune) hypophysitis: a single centre experience. Pituitary. 2015;18(1):16–22.
Honegger J, Schlaffer S, Menzel C, Droste M, Werner S, Elbelt U, et al. Diagnosis of primary hypophysitis in Germany. J Clin Endocrinol Metabol. 2015;100(10):3841–9.
Vasikaran S, Tallis G, Braund W. Secondary hypoadrenalism presenting with hypercalcaemia. Clin Endocrinol. 1994;41(2):261–4.
Jensen MD, Handwerger BS, Scheithauer BW, Carpenter PC, Mirakian R, Banks PM. Lymphocytic hypophysitis with isolated corticotropin deficiency. Ann Intern Med. 1986;105(2):200–3.
Richtsmeier AJ, Henry RA, Bloodworth J, Ehrlich EN. Lymphoid hypophysitis with selective adrenocorticotropic hormone deficiency. Arch Intern Med. 1980;140(9):1243–5.
JAIn A, Dhanwal DK. A rare case of autoimmune hypophysitis presenting as temperature dysregulation. J Clin Diagn Res. 2015;9(2):OD09.
Fleseriu M, Hashim IA, Karavitaki N, Melmed S, Murad MH, Salvatori R, et al. Hormonal replacement in hypopituitarism in adults: an endocrine society clinical practice guideline. J Clin Endocrinol Metabol. 2016;101(11):3888–921.
Lupi I, Cosottini M, Caturegli P, Manetti L, Urbani C, Cappellani D, et al. Diabetes insipidus is an unfavorable prognostic factor for response to glucocorticoids in patients with autoimmune hypophysitis. Eur J Endocrinol. 2017;177(2):127–35.
Elizondo G, Saldivar D, Nanez H, Todd LE, Villarreal JZ. Pituitary gland growth during normal pregnancy: an in vivo study using magnetic resonance imaging. Am J Med. 1988;85(2):217–20.
Holder CA, Elster AD. Magnetization transfer imaging of the pituitary: further insights into the nature of the posterior “bright spot”. J Comput Assist Tomogr. 1997;21(2):171–4.
Kucharczyk W, Lenkinski RE, Kucharczyk J, Henkelman RM. The effect of phospholipid vesicles on the NMR relaxation of water: an explanation for the MR appearance of the neurohypophysis? AJNR Am J Neuroradiol 1990;11(4):693–700
Fujisawa I, Murakami N, Furuto-Kato S, Araki N, Konishi J. Plasma and neurohypophyseal content of vasopressin in diabetes mellitus. J Clin Endocrinol Metab 1996;81(8):2805–9
Brooks BS, El Gammal T, Allison JD, Hoffman WH. Frequency and variation of the posterior pituitary bright signal on MR images. Am J Roentgenol. 1989;153(5):1033–8.
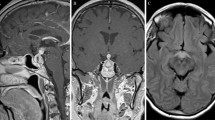
Ahmadi J, Meyers GS, Segall HD, Sharma OP, Hinton DR. Lymphocytic adenohypophysitis: contrast-enhanced MR imaging in five cases. Radiology. 1995;195(1):30–4.
Saiwai S, Inoue Y, Ishihara T, Matsumoto S, Nemoto Y, Tashiro T, et al. Lymphocytic adenohypophysitis: skull radiographs and MRI. Neuroradiology. 1998;40(2):114–20.
Powrie J, Powell Y, Ayers A, Lowy C, Sönksen P. Lymphocytic adenohypophysitis: magnetic resonance imaging features of two new cases and a review of the literature. Clin Endocrinol. 1995;42(3):315–22.
Terao T, Taya K, Sawauchi S, Nakazaki H, Numoto RT, Yamaguchi Y, et al. Lymphocytic infundibuloneurohypophysitis の 2 例. No Shinkei Geka. 2003;31(11):1229–35.
Leggett D, Hill P, Anderson R. Stalkitis’ in a pregnant 32-year-old woman: a rare cause of diabetes insipidus. Australas Radiol. 1999;43(1):104–7.
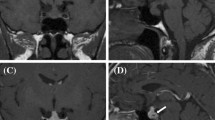
Gutenberg A, Larsen J, Lupi I, Rohde V, Caturegli P. A radiologic score to distinguish autoimmune hypophysitis from nonsecreting pituitary adenoma preoperatively. Am J Neuroradiol. 2009;30(9):1766–72.
Terano T, Seya A, Tamura Y, Yoshida S, Hirayama T. Characteristics of the pituitary gland in elderly subjects from magnetic resonance images: relationship to pituitary hormone secretion. Clin Endocrinol. 1996;45(3):273–9.
Heshmati HM, Kujas M, Casanova S, Wollan PC, Racadot J, Van Effenterre R, et al. Prevalence of lymphocytic infiltrate in 1400 pituitary adenomas. Endocr J. 1998;45(3):357–61.
Flanagan D, Ibrahim A, Ellison D, Armitage M, Gawne-Cain M, Lees P. Inflammatory hypophysitis–the spectrum of disease. Acta Neurochir. 2002;144(1):47–56.
Crock PA. Cytosolic autoantigens in lymphocytic hypophysitis. J Clin Endocrinol Metabol. 1998;83(2):609–18.
Manetti L, Lupi I, Morselli LL, Albertini S, Cosottini M, Grasso L, et al. Prevalence and functional significance of antipituitary antibodies in patients with autoimmune and non-autoimmune thyroid diseases. J Clin Endocrinol Metabol. 2007;92(6):2176–81.
Mau M, Phillips TM, Ratner RE. Presence of anti-pituitary hormone antibodies in patients with empty sella syndrome and pituitary tumours. Clin Endocrinol. 1993;38(5):495–500.
Ricciuti A, De Remigis A, Landek-Salgado MA, De Vincentiis L, Guaraldi F, Lupi I, et al. Detection of pituitary antibodies by immunofluorescence: approach and results in patients with pituitary diseases. J Clin Endocrinol Metabol. 2014;99(5):1758–66.
Lupi I, Manetti L, Raffaelli V, Grasso L, Sardella C, Cosottini M, et al. Pituitary autoimmunity is associated with hypopituitarism in patients with primary empty sella. J Endocrinol Investig. 2011;34(8):e240–e4.
Kovacs K. Sheehan syndrome. Lancet. 2003;361(9356):520–2.
Park SM, Bae JC, Joung JY, Cho YY, Kim TH, Jin S-M, et al. Clinical characteristics, management, and outcome of 22 cases of primary hypophysitis. Endocrinol Metab. 2014;29(4):470–8.
Kristof RA, Van Roost D, Klingmüller D, Springer W, Schramm J. Lymphocytic hypophysitis: non-invasive diagnosis and treatment by high dose methylprednisolone pulse therapy? J Neurol Neurosurg Psychiatry. 1999;67(3):398–402.
Prete A, Salvatori R. Hypophysitis. In: DeGroot LJ, Chrousos G, Dungan K, Feingold KR, Grossman A, Hershman JM, Koch C, Korbonits M, McLachlan R, New M, Purnell J, Rebar R, Singer F, Vinik A, editors. Endotext (Internet). South Dartmouth (MA): MDText.com, Inc. 2000; 2018.
Schreckinger M, Francis T, Rajah G, Jagannathan J, Guthikonda M, Mittal S. Novel strategy to treat a case of recurrent lymphocytic hypophysitis using rituximab. J Neurosurg. 2012;116(6):1318–23.
Ray D, Yen C, Vance M, Laws E, Lopes B, Sheehan J. Gamma knife surgery for lymphocytic hypophysitis. J Neurosurg. 2010;112(1):118.
Honegger J, Buchfelder M, Schlaffer S, Droste M, Werner S, Strasburger C, et al. Treatment of primary hypophysitis in Germany. J Clin Endocrinol Metabol. 2015;100(9):3460–9.
Sotoudeh H, Yazdi HR. A review on dural tail sign. World J Radiol. 2010;2(5):188.
Catford S, Wang YY, Wong R. Pituitary stalk lesions: systematic review and clinical guidance. Clin Endocrinol. 2016;85(4):507–21.
Folkerth RD, Price DL Jr, Schwartz M, Black PM, De Girolami U. Xanthomatous hypophysitis. Am J Surg Pathol. 1998;22(6):736–41.
Duan K, Asa SL, Winer D, Gelareh Z, Gentili F, Mete O. Xanthomatous hypophysitis is associated with ruptured Rathke’s cleft cyst. Endocr Pathol. 2017;28(1):83–90.
Kleinschmidt-DeMasters B, Lillehei KO, Hankinson TC. Review of xanthomatous lesions of the sella. Brain Pathol. 2017;27(3):377–95.
Oishi M, Hayashi Y, Fukui I, Kita D, Miyamori T, Nakada M. Xanthomatous hypophysitis associated with autoimmune disease in an elderly patient: a rare case report. Surg Neurol Int. 2016;7(Suppl 16):S449.
Khosroshahi A, Wallace Z, Crowe J, Akamizu T, Azumi A, Carruthers M, et al. International consensus guidance statement on the management and treatment of IgG4-related disease. Arthritis Rheum. 2015;67(7):1688–99.
Lin W, Lu S, Chen H, Wu Q, Fei Y, Li M, et al. Clinical characteristics of immunoglobulin G4–related disease: a prospective study of 118 Chinese patients. Rheumatology. 2015;54(11):1982–90.
Stone JH, Zen Y, Deshpande V. IgG4-related disease. N Engl J Med. 2012;366(6):539–51.
Barroso-Sousa R, Barry WT, Garrido-Castro AC, Hodi FS, Min L, Krop IE, et al. Incidence of endocrine dysfunction following the use of different immune checkpoint inhibitor regimens: a systematic review and meta-analysis. JAMA Oncol. 2018;4(2):173–82.
Funding
This work was supported in part by the Intramural Research Program, NICHD, NIH.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Prof. Koch declares no direct conflict with this article. He has served on the Advisory Board of Novartis on the topic acromegaly and has participated in educational conferences on the topics neuroendocrine tumors and acromegaly sponsored by Novartis and Ipsen. The other authors Drs. Sriram Gubbi, Fady Hannah-Shmouni, and Constantine A. Stratakis declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Gubbi, S., Hannah-Shmouni, F., Stratakis, C.A. et al. Primary hypophysitis and other autoimmune disorders of the sellar and suprasellar regions. Rev Endocr Metab Disord 19, 335–347 (2018). https://doi.org/10.1007/s11154-018-9480-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11154-018-9480-1