Abstract
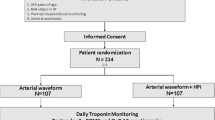
With pulseless electrical activity (PEA) emerging as one of the leading cardiac arrest arrhythmias, the rapid response and accurate diagnosis of PEA is essential to improve survival rates. Although the use of invasive blood pressure monitoring to more quickly detect changes in blood pressure is widespread, evidence for its use is largely anecdotal and placement is not without risk. This is a prospective, multi-center, randomized controlled trial involving 58 senior anesthesiology residents undergoing a simulation of intraoperative PEA using high-fidelity simulation. Of the total 58 participants, 28 subjects were randomized to invasive blood pressure monitoring and 30 to non-invasive blood pressure monitoring in order to investigate the effects of arterial line information on the response time of ACLS-trained anesthesiology residents. Response times of subjects in the group provided with invasive blood pressure monitoring were faster to palpate pulses (6.5 s faster, p = .0470), initiate chest compressions (17 s faster, p = .004), and administer 1 mg of epinephrine (21 s faster, p = .0005. The absolute number of pharmacologic interventions was increased in the group with invasive blood pressure monitoring (p = .020). These findings suggest that noninvasive blood pressure monitoring and other readily available monitors are not as powerful as invasive blood pressure monitoring in influencing decision-making during a PEA event. As there is currently no specific blood pressure at which the patient is considered to be in PEA, future studies are necessary to clarify the correlation between the arterial line tracing and the appropriate trigger for ACLS initiation.




Similar content being viewed by others
References
American Society of Anesthesiologists Standards for Basic Anesthetic Monitoring (2010) http://www.asahq.org/quality-and-practice-management/standards-and-guidelines/search?q=monitoring. Accessed 4 Apr 2016.
Schroeder RA, Barbeito A, Bar-Yosef S, Mark JB. Cardiovascular Monitoring. In: Miller RD, Eriksson LI, Fleisher LA, Wiener-Kronish JP, Young WL, editors. Miller's Anesthesia. 7th ed. Philadelphia: Churchill Livingstone Elsevier; 2010. p. 1267–328.
Scheer BV, Perel A, Pfeiffer UJ. Clinical review: complications and risk factors of peripheral arterial catheters used for haemodynamic monitoring in anaesthesia and intensive care medicine. Crit Care. 2002;6(3):199–204.
Garland A, Connors AF Jr. Indwelling arterial catheters in the intensive care unit: necessary and beneficial, or a harmful crutch? Am J Respir Crit Care Med. 2010;182(2):133–4.
Wax DB, Lin HM, Leibowitz AB. Invasive and concomitant noninvasive intraoperative blood pressure monitoring: observed differences in measurements and associated therapeutic interventions. Anesthesiology. 2011;115(5):973–8.
Walsh M, Devereaux PJ, Garg AX, et al. Relationship between intraoperative mean arterial pressure and clinical outcomes after noncardiac surgery: toward an empirical definition of hypotension. Anesthesiology. 2013;119(3):507–15.
Monk TG, Bronsert MR, Henderson WG, et al. Association between intraoperative hypotension and hypertension and 30-day postoperative mortality in noncardiac Surgery. Anesthesiology. 2015;123(2):307–19.
Bergum D, Nordseth T, Mjølstad OC, Skogvoll E, Haugen BO. Causes of in-hospital cardiac arrest—incidences and rate of recognition. Resuscitation. 2015;87:1–6.
Donnino MW, Salciccioli JD, Howell MD, et al. Time to administration of epinephrine and outcome after in-hospital cardiac arrest with non-shockable rhythms: retrospective analysis of large in-hospital data registry. BMJ. 2014;348:g3028.
Desbiens NA. Simplifying the management of pulseless electrical activity in adults: a qualitative review. Crit Care Med. 2008;36(2):391–6.
Link MS, Berkow LC, Kudenchuk PJ, et al. Part 7: adult advanced cardiovascular life support: 2015 American heart association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132:S444–64.
Neumar RW, Otto CW, Link MS, et al. Part 8: adult advanced cardiovascular life support: 2010 American heart association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2010;122(18):S729–67.
Nuttall G, Burckhardt J, Hadley A, et al. Surgical and patient risk factors for severe arterial line complications in adults. Anesthesiology. 2016;124(3):590–7.
Gershengorn HB, Garland A, Kramer A, et al. Variation of arterial and central venous catheter use in the United States intensive care units. Anesthesiology. 2014;120(3):650–64.
Truhlář A, et al. European resuscitation council guidelines for resuscitation 2015: section 4. Cardiac arrest in special circumstances. Resuscitation. 2015;95:148–201.
Brearley S, Shearman CP, Simms MH. Peripheral pulse palpation: an unreliable physical sign. Ann R Coll Surg Engl. 1992;74(3):169–71.
Paradis NA, Martin GB, Goetting MG, et al. Aortic pressure during human cardiac arrest, identification of pseudo-electromechanical dissociation. Chest. 1992;101(1):123–8.
Meaney PA, Bobrow BJ, Mancini ME, et al. Cardiopulmonary resuscitation quality: [corrected] improving cardiac resuscitation outcomes both inside and outside the hospital: a consensus statement from the American heart association. Circulation. 2013;128(4):417–35.
Acknowledgements
We are extremely grateful for the contributions of Gary Chan for his assistance with data collection as well as Michael Durda for helping with manuscript preparation. Also thanks to Scott Winfield and the Clinical Skills Education and Assessment Center at the OSU College of Medicine for their technical assistance without which this study would not be possible.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have any academic or financial conflicts of interest with respect to this study. Dr. Levine receives royalties from Springer Publishing, an honorarium from the American Society of Anesthesiology, and serves on the advisory board for GTX Surgery.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional review board and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
As stated above informed consent was obtained from all individual participants included in the study.
Appendices
Appendix
1.1 Supporting files
-
1.
Patient’s preoperative assessment
-
2.
Pertinent Laboratory data
1.2 Roles
-
1.
Anesthesiologist
-
2.
Surgeon
-
3.
Scrub
1.3 Monitors available to participant (control)
-
Noninvasive blood pressure cuff
-
Five-lead electrocardiogram
-
Pulse-oximetry
-
Temperature probe
-
End-tidal CO2 monitor
1.4 Other equipment required
-
Airway equipment including Macintosh 3 and Miller 2 blades, endotracheal tube 7.5 with stylette and empty 10 mL syringe.
-
1000 mL intravenous fluid bags on a 18 G IV line.
-
Pharmacologic agents available upon request: propofol, etomidate, ketamine, succinylcholine, vecuronium, midazolam, fentanyl, atropine, ephedrine, esmolol, phenylephrine, epinephrine (in syringe and prepared in 100 mL saline bag), norepinephrine (in syringe and prepared in 100 mL saline bag), vasopressin, code dose epinephrine (1:10,000 in 10 ml).
-
Yankauer suction.
-
Self-inflating resuscitation bag for venitlation.
1.5 Time duration
-
Setup: 5 min
-
Preparation: 5 min
-
Simulation: 15 min
-
Debriefing: 10 min
Case stem
Our simulated patient is a 75 year-old male who presented to the ED 3 h ago for severe abdominal pain. An abdominal x-ray shows free abdominal air, and he is scheduled for an emergent exploratory laparotomy. His past medical history is significant for CAD with DES × 2 8 months prior at an outside hospital. He used to be on ASA and plavix, but stopped taking these several weeks ago. He is currently taking carvedilol 6.25 mg twice daily, a statin, and lasix 20 mg daily both of which he took this morning. He has a history of CHF, but there is no echocardiogram available. He also has a history of OSA. He has been NPO for 24 h.
Upon participant arrival to the PACU, the patient has an 18 G IV in his left arm, and he is lying in bed complaining of severe abdominal pain.
2.1 Background and briefing information for facilitator/coordinator’s eyes only
The objective of this simulation is for the participant to identify PEA after induction and effectively manage the situation with chest compressions and initiation of ACLS. The simulation scenario will be followed by a standardized debriefing session.
2.1.1 Control group
In this simulation, the patient is lying on the OR table with a noninvasive BP cuff, pulse-oximeter, and ECG monitoring when the participant arrives. The ECG will display sinus rhythm with a rate of 75. The patient is complaining of severe abdominal pain. Immediately following induction of general anesthesia, the patient’s heart rate will increase to the mid 90’s, and blood pressure will become 85/42. The blood pressure cuff will be set to cycle once every 3 min. During laryngoscopy, tachycardia will occur to 117 with transient hypertension (157/107). Following intubation, over 180 s, ST segment changes will occur in the leads II and V5 leading to eventual PEA manifesting as a drop in end tidal carbon dioxide (ETCO2) from 40 to 8, a loss of pulse-oximetry, and a loss of palpable pulses (SBP < 50 mmHg). This sequence of events will occur regardless of the drugs chosen for induction or any subsequent intervention. Cycling the blood pressure cuff at this point will not result in a blood pressure measurement. Once both chest compressions have been initiated and the patient has been given epinephrine, the scenario will end.
2.1.2 Intervention group
In this simulation, the patient is lying on the OR table with a invasive arterial line BP reading, pulse-oximeter, and ECG monitoring when the participant arrives. The ECG will display sinus rhythm with a rate of 75. The patient is complaining of severe abdominal pain. Immediately following induction of general anesthesia, the patient’s heart rate will increase to the mid 90’s, and blood pressure will become 85/42. During laryngoscopy, tachycardia will occur to 117 with transient hypertension (157/107). Following intubation, over 180 s, ST segment changes will occur in leads II and V5 leading to eventual PEA manifesting as a drop in end tidal carbon dioxide (ETCO2) from 40 to 8, a loss of pulse-oximetry, and a loss of palpable pulses (SBP < 50 mmHg). This sequence of events will occur regardless of the drugs chosen for induction or any subsequent intervention. Administration of vasopressors during this time period without initiation of chest compressions willl lead to only transient increases in blood pressure but no return of spontaneous pulses. Once both chest compressions have been initiated and the patient has been given 1 mg epinephrine, the scenario will end.
Patient data background and baseline status
3.1 Patient history
Bert Cooper is a 75-year-old male with a history of CAD with DES × 2 8 months prior. He has a history of diverticulosis and presented to the emergency department several hours ago with severe abdominal pain. His medications include plavix and ASA both of which he states he stopped taking 2 weeks ago because is scripts ran out. He also has a history of OSA and CHF for which he takes lasix 20 mg and carvedilol 6.25 mg twice daily. He took both of these medications today. His surgical history is significant for an uncomplicated hemicolectomy 10 years ago. At baseline patient can walk up one flight of stairs and do light housework. He is limited by hp and knee pain related to osteoarthritis. He last ate 10 h ago.
3.2 Review of systems
-
CNS: WNL
-
Cardiovascular: CAD, no recent CP, SOB
-
Pulmonary: no SOB, DOE, orthopnea
-
Abdominal: Severe, diffuse abdoinal pain
-
Renal: No problems.
-
Psychiatric: No symptoms of anxiety or depression.
3.3 Current medications and allergies
-
Plavix (discontinued ×2 weeks)
-
Carvedilol (6.25 mg BID)
-
Lasix 20 mg daily
-
Aspirin 81 (discontinued ×2 weeks)
-
Pravastatin
-
The patient has no known drug allergies (NKDA)
3.4 Physical examination
-
General: Visible discomfort
-
Weight: 120 kg
-
Height: 68 inches
-
Vital Signs: BP: 157/88, HR: 75, Respiratory rate: 25, Temperature: 37.3 °C, SpO2: 98 %
-
Airway: MP II, adequate TMD, opening
-
Lungs: bilateral breath sounds, no wheezing, rales or rhonchi
-
Heart: NSR, no murmurs, rubs, or gallops
-
Abdomen: tender to palpation with rebound and guarding
3.5 Laboratory, radiology, and other relevant studies
-
Coagulation studies WNL
-
HCT: 29 Chem7: WNL
-
Type and Screen: done
Patient data background and baseline status
-
History of Present Illness: 1 day of severe abdominal pain
-
Past Medical History: CAD with DES ×2, CHF, OSA
-
Past Surgical History: hemicolectomy (10 years ago)
-
Family History: none
-
Review of Systems: CAD
-
Medications and Allergies: plavix (d/c’d × 2 week), carvedilol (took this morning), aspirin (d/d’d × 2 weeks), statin, lasix
-
NPO status: 10 h ago
-
Current Physical Examination: In apparent distress
-
Laboratory, Radiology, and Other Relevant Studies: HCT 29
SCRIPT:
Patient
“Doc I’m really nervous for surgery.”
Patient answers questions whose answers are directly stated in history
If the resident asks for an arterial line in the NIBP group, they will be informed that a pressure bag is not immediately available and surgery cannot be delayed at this time.
Upon induction, regardless of medications given, initiate HPS induction sequence.
Upon laryngoscopy initiate HPS intubation sequence.
Once ETT placed and patient on ventilator initiate MI sequence
Once ETT is secured surgeon will put up drapes and proceed with Time Out:
Surgeon:
“I’m Dr. B with surgery. Before proceeding we will do a time out. This patient is Bert Cooper, he’s a 75 year old male here for an emergency exploratory laparatomy. He will be in the supine position. He’s not allergic no any medications. He should receive 2 g of ancef. He will go to the PACU after surgery. Are there any questions or concerns?
If the resident does not express any concerns during the scenario the surgeon should continue to work. In the NIBP group the confederate should disconnect the pulse-ox and BP cuff at the first loss of pulse-ox waveform on the anesthesia monitor.
If the resident asks the surgeon to stop operating or take down the drapes he/she should do so.
If the resident asks the surgeon or scrub to start chest compressions he/she should do so.
The scenario ends once the participant has both given epinephrine and chest compressions have started.
Rights and permissions
About this article
Cite this article
Lipps, J., Goldberg, A., DeMaria, S. et al. Presence of an arterial line improves response to simulated hypotension and pulseless electrical activity. J Clin Monit Comput 31, 911–918 (2017). https://doi.org/10.1007/s10877-016-9919-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-016-9919-4