Abstract
Purpose
Immune thrombocytopenic purpura (ITP) and autoimmune hemolytic anemia (AIHA) are associated in the definition of Evans syndrome (ES). The occurrence of neurological involvement in this population is poorly described and suggests an underlying primary immunodeficiency (PID). We aimed to describe the clinical manifestations, evolution, and PID profiles of these patients.
Methods
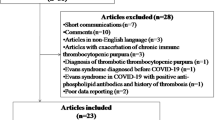
OBS’CEREVANCE is a French, nationwide prospective cohort that includes children with chronic ITP, AIHA, and ES. Patients with a neurological involvement were described. Centralized radiological and pathological reviews and genetic analyses were performed.
Results
On October 2016, eight patients (7/181 ES, 1/371 AIHA, and 0/615 ITP) were identified, all male, with a median age (range) at cytopenia onset of 11.5 years (1.6–15.8). Neurological symptoms appeared with a median delay of 6 years (2.5–18) after cytopenia and were polymorphic: seizures (n = 4), cranial nerve palsy (n = 2), Brown-Sequard syndrome (n = 2), intracranial pressure (n = 2), vertigo (n = 1), and/or sensory neuropathy (n = 1). Magnetic resonance imaging (MRI) showed inflammatory lesions, confirmed by pathology for five patients with macrophagic or lymphoplasmocytic infiltrates. All patients had other relevant immunopathological manifestations: pulmonary nodules (n = 6), lymphoproliferation (n = 4), abnormal immunophenotype (n = 8), and hypogammaglobulinemia (n = 7). Treatment consisted of steroids that improved symptomatology and MRI. Five patients relapsed and three had an asymptomatic radiological progression. A PID was identified in 3/8 patients: 22q11.2 microdeletion (n = 1) and CTLA deficiency (n = 2).
Conclusion
Neurological involvement is a rare and severe late event in the course of childhood ES, which can reveal an underlying PID. Imaging and pathology examination highlight a causative immune dysregulation that may guide targeted therapeutic strategies.




Similar content being viewed by others
References
Terrell DR, Beebe LA, Vesely SK, Neas BR, Segal JB, George JN. The incidence of immune thrombocytopenic purpura in children and adults: a critical review of published reports. Am J Hematol. 2010;85(3):174–80.
Moulis G, Palmaro A, Montastruc J-L, Godeau B, Lapeyre-Mestre M, Sailler L. Epidemiology of incident immune thrombocytopenia: a nationwide population-based study in France. Blood. 2014;124(22):3308–15.
Aladjidi N, Fernandes H, Leblanc T, Vareliette A, Rieux-Laucat F, Bertrand Y, et al. Evans syndrome in children: long-term outcome in a prospective French national observational cohort. Front Pediatr. 2015;3:79.
Aladjidi N, Jutand M-A, Beaubois C, Fernandes H, Jeanpetit J, Coureau G, et al. Reliable assessment of the incidence of childhood autoimmune hemolytic anemia. Pediatr Blood Cancer. 2017; 64(12).
Seif AE, Manno CS, Sheen C, Grupp SA, Teachey DT. Identifying autoimmune lymphoproliferative syndrome in children with Evans syndrome: a multi-institutional study. Blood. 2010;115(11):2142–5.
Zuelzer WW, Mastrangelo R, Stulberg CS, Poulik MD, Page RH, Thompson RI. Autoimmune hemolytic anemia. Natural history and viral-immunologic interactions in childhood. Am J Med. 1970;49(1):80–93.
Savaşan S, Warrier I, Buck S, Kaplan J, Ravindranath Y. Increased lymphocyte Fas expression and high incidence of common variable immunodeficiency disorder in childhood Evans’ syndrome. Clin Immunol. 2007;125(3):224–9.
Michel M, Chanet V, Galicier L, Ruivard M, Levy Y, Hermine O, et al. Autoimmune thrombocytopenic purpura and common variable immunodeficiency: analysis of 21 cases and review of the literature. Medicine (Baltimore). 2004;83(4):254–63.
Heeney MM, Zimmerman SA, Ware RE. Childhood autoimmune cytopenia secondary to unsuspected common variable immunodeficiency. J Pediatr. 2003;143(5):662–5.
Fischer A, Provot J, Jais J-P, Alcais A, Mahlaoui N. Autoimmune and inflammatory manifestations occur frequently in patients with primary immunodeficiencies. J Allergy Clin Immunol. 2017;140(5):1388–1393.e8.
Parvaneh N, Casanova J-L, Notarangelo LD, Conley ME. Primary immunodeficiencies: a rapidly evolving story. J Allergy Clin Immunol. 2013;131(2):314–23.
Seidel MG. Autoimmune and other cytopenias in primary immunodeficiencies: pathomechanisms, novel differential diagnoses, and treatment. Blood. 2014;124(15):2337–44.
Bousfiha A, Jeddane L, Picard C, Ailal F, Gaspar HB, Al-Herz W, et al. The 2017 IUIS phenotypic classification for primary immunodeficiencies. J Clin Immunol. 2018;38(1):129–43.
Lo B, Fritz JM, Su HC, Uzel G, Jordan MB, Lenardo MJ. CHAI and LATAIE: new genetic diseases of CTLA-4 checkpoint insufficiency. Blood. 2016;128(8):1037–42.
Elgizouli M, Lowe DM, Speckmann C, Schubert D, Hülsdünker J, Eskandarian Z, et al. Activating PI3Kδ mutations in a cohort of 669 patients with primary immunodeficiency. Clin Exp Immunol. 2016;183(2):221–9.
Aladjidi N, Leverger G, Leblanc T, Picat MQ, Michel G, Bertrand Y, et al. New insights into childhood autoimmune hemolytic anemia: a French national observational study of 265 children. Haematologica. 2011 May 1;96(5):655–63.
Buchanan GR, Adix L. Grading of hemorrhage in children with idiopathic thrombocytopenic purpura. J Pediatr. 2002;141(5):683–8.
Benjamin DJ, Berger JO, Johannesson M, Nosek BA, Wagenmakers E-J, Berk R, et al. Redefine statistical significance. Nat Hum Behav. 2018;2(1):6–10.
Park JH, Levinson AI. Granulomatous-lymphocytic interstitial lung disease (GLILD) in common variable immunodeficiency (CVID). Clin Immunol. 2010;134(2):97–103.
Simon OJ, Kuhlmann T, Bittner S, Müller-Tidow C, Weigt J, Wiendl H, et al. Evans syndrome associated with sterile inflammation of the central nervous system: a case report. J Med Case Rep. 2013;7:262.
Stübgen J-P. Central nervous system inflammatory demyelination after rituximab therapy for idiopathic thrombocytopenic purpura. J Neurol Sci. 2010;288(1–2):178–81.
Matsui H, Udaka F, Tamura A, Oda M, Kubori T, Nishinaka K, et al. Multiple sclerosis following splenectomy as a treatment for idiopathic thrombocytopenic purpura. Intern Med Tokyo Jpn. 2005;44(7):747–9.
Mizuno H, Sato S, Ohnishi Y, Takahashi T, Nakashima I, Fujihara K, et al. A case of myelitis with anti-aquaporin 4 antibody concomitant with immune thrombocytopenic purpura. Rinshō Shinkeigaku Clin Neurol. 2014;54(3):195–9.
Guez T, Smadja D, Mas JL, Sicard D. Chronic inflammatory demyelinating polyradiculoneuropathy associated with Evans’ syndrome. Eur J Med. 1992;1(6):374–6.
Knecht H, Baumberger M, Tobòn A, Steck A. Sustained remission of CIDP associated with Evans syndrome. Neurology. 2004;63(4):730–2.
Savaşan S, Warrier I, Ravindranath Y. The spectrum of Evans’ syndrome. Arch Dis Child. 1997;77(3):245–8.
Sipurzynski J, Fahrner B, Kerbl R, Crazzolara R, Jones N, Ebetsberger G, et al. Management of chronic immune thrombocytopenia in children and adolescents: lessons from an Austrian national cross-sectional study of 81 patients. Semin Hematol. 2016;53(Suppl 1):S43–7.
Miano M, Scalzone M, Perri K, Palmisani E, Caviglia I, Micalizzi C, et al. Mycophenolate mofetil and Sirolimus as second or further line treatment in children with chronic refractory primitive or secondary autoimmune Cytopenias: a single Centre experience. Br J Haematol. 2015;171(2):247–53.
Bride KL, Vincent T, Smith-Whitley K, Lambert MP, Bleesing JJ, Seif AE, et al. Sirolimus is effective in relapsed/refractory autoimmune cytopenias: results of a prospective multi-institutional trial. Blood. 2016;127(1):17–28.
Miano M, Ramenghi U, Russo G, Rubert L, Barone A, Tucci F, et al. Mycophenolate mofetil for the treatment of children with immune thrombocytopenia and Evans syndrome. A retrospective data review from the Italian association of paediatric haematology/oncology. Br J Haematol. 2016;175(3):490–5.
Jasinski S, Weinblatt ME, Glasser CL. Sirolimus as an effective agent in the treatment of immune thrombocytopenia (itp) and Evans syndrome (es): a single institution’s experience. J Pediatr Hematol Oncol. 2017;39(6):420–4.
Androdias G, Maillet D, Marignier R, Pinède L, Confavreux C, Broussolle C, et al. Mycophenolate mofetil may be effective in CNS sarcoidosis but not in sarcoid myopathy. Neurology. 2011;76(13):1168–72.
Garssen MPJ, van Koningsveld R, van Doorn PA, Merkies ISJ, Scheltens-de Boer M, van Leusden JA, et al. Treatment of Guillain-Barré syndrome with mycophenolate mofetil: a pilot study. J Neurol Neurosurg Psychiatry. 2007;78(9):1012–3.
Xiao Y, Huang J, Luo H, Wang J. Mycophenolate mofetil for relapsing-remitting multiple sclerosis. Cochrane Database Syst Rev. 2014;2:CD010242.
Bagherpour B, Salehi M, Jafari R, Bagheri A, Kiani-Esfahani A, Edalati M, et al. Promising effect of rapamycin on multiple sclerosis. Mult Scler Relat Disord. 2018;26:40–5.
Besnard C, Levy E, Aladjidi N, Stolzenberg M-C, Magerus-Chatinet A, Alibeu O, et al. Pediatric-onset Evans syndrome: heterogeneous presentation and high frequency of monogenic disorders including LRBA and CTLA4 mutations. Clin Immunol Orlando Fla. 2018;188:52–7.
Brignier AC, Mahlaoui N, Reimann C, Picard C, Kracker S, de Vergnes N, et al. Early-onset hypogammaglobulinemia: a survey of 44 patients. J Allergy Clin Immunol. 2015;136(4):1097–1099.e2.
Tison BE, Nicholas SK, Abramson SL, Hanson IC, Paul ME, Seeborg FO, et al. Autoimmunity in a cohort of 130 pediatric patients with partial DiGeorge syndrome. J Allergy Clin Immunol. 2011;128(5):1115–1117.e3.
Colarusso G, Gambineri E, Lapi E, Casini T, Tucci F, Lippi F, et al. Evans syndrome and antibody deficiency: an atypical presentation of chromosome 22q11.2 deletion syndrome. Pediatr Rep. 2010;2(2):e13.
Kratz CP, Niehues T, Lyding S, Heusch A, Janssen G, Göbel U. Evans syndrome in a patient with chromosome 22q11.2 deletion syndrome: a case report. Pediatr Hematol Oncol. 2003;20(2):167–72.
Kuehn HS, Ouyang W, Lo B, Deenick EK, Niemela JE, Avery DT, et al. Immune dysregulation in human subjects with heterozygous germline mutations in CTLA4. Science. 2014;345(6204):1623–7.
Schubert D, Bode C, Kenefeck R, Hou TZ, Wing JB, Kennedy A, et al. Autosomal dominant immune dysregulation syndrome in humans with CTLA4 mutations. Nat Med. 2014;20(12):1410–6.
Lo B, Zhang K, Lu W, Zheng L, Zhang Q, Kanellopoulou C, et al. Patients with LRBA deficiency show CTLA4 loss and immune dysregulation responsive to abatacept therapy. Science. 2015 Jul 24;349(6246):436–40.
Lopez-Herrera G, Tampella G, Pan-Hammarström Q, Herholz P, Trujillo-Vargas CM, Phadwal K, et al. Deleterious mutations in LRBA are associated with a syndrome of immune deficiency and autoimmunity. Am J Hum Genet. 2012;90(6):986–1001.
Alangari A, Alsultan A, Adly N, Massaad MJ, Kiani IS, Aljebreen A, et al. LPS-responsive beige-like anchor (LRBA) gene mutation in a family with inflammatory bowel disease and combined immunodeficiency. J Allergy Clin Immunol. 2012;130(2):481–488.e2.
Burns SO, Zenner HL, Plagnol V, Curtis J, Mok K, Eisenhut M, et al. LRBA gene deletion in a patient presenting with autoimmunity without hypogammaglobulinemia. J Allergy Clin Immunol. 2012 Dec;130(6):1428–32.
Seidel MG, Hirschmugl T, Gamez-Diaz L, Schwinger W, Serwas N, Deutschmann A, et al. Long-term remission after allogeneic hematopoietic stem cell transplantation in LPS-responsive beige-like anchor (LRBA) deficiency. J Allergy Clin Immunol. 2015;135(5):1384–1390.e1–8.
Charbonnier L-M, Janssen E, Chou J, Ohsumi TK, Keles S, Hsu JT, et al. Regulatory T-cell deficiency and immune dysregulation, polyendocrinopathy, enteropathy, X-linked-like disorder caused by loss-of-function mutations in LRBA. J Allergy Clin Immunol. 2015;135(1):217–27.
Hayakawa S, Okada S, Tsumura M, Sakata S, Ueno Y, Imai K, et al. A patient with CTLA-4 haploinsufficiency presenting gastric cancer. J Clin Immunol. 2016;36(1):28–32.
Gámez-Díaz L, August D, Stepensky P, Revel-Vilk S, Seidel MG, Noriko M, et al. The extended phenotype of LPS-responsive beige-like anchor protein (LRBA) deficiency. J Allergy Clin Immunol. 2016;137(1):223–30.
Schwab C, Gabrysch A, Olbrich P, Patiño V, Warnatz K, Wolff D, et al. Phenotype, penetrance, and treatment of 133 CTLA-4-insufficient individuals. J Allergy Clin Immunol. 2018;142(6):1932–1946.
Notarangelo LD, Fleisher TA. Targeted strategies directed at the molecular defect: toward precision medicine for select primary immunodeficiency disorders. J Allergy Clin Immunol. 2017 Mar;139(3):715–23.
Lee S, Moon JS, Lee C-R, Kim H-E, Baek S-M, Hwang S, et al. Abatacept alleviates severe autoimmune symptoms in a patient carrying a de novo variant in CTLA-4. J Allergy Clin Immunol. 2016 Jan;137(1):327–30.
van Leeuwen EM, Cuadrado E, Gerrits AM, Witteveen E, de Bree GJ. Treatment of intracerebral lesions with Abatacept in a CTLA4-Haploinsufficient patient. J Clin Immunol. 2018;38(4):464–467.
Authorship contributions.
TP, BN, JLP, FRL, and NA designed the research, analyzed the data, and participated in writing the paper. HDLP reviewed the MRI. PV and AG reviewed the pathology samples. HF was the data manager and performed the statistical analyses. FRL performed the biology molecular analyses. BN, JLP, NA, GL, TL, HC, GM, MP, FM, OH, AM, MHu, HZ, MHa, JMD, and YP were in charge of the patients and participated in data and blood sample collection. All authors critically read the manuscript, approved the final version, and agreed to be accountable for all aspects of the work.
Funding
The clinical database OBS’CEREVANCE was funded by the GIS-Institut des Maladies Rares (INSERM); the French Ministry of Health (Rare Disease Plan, PHRC 2005); the Association Bordelaise pour l’Avancement des Sciences Pédiatriques (ABASP) research charity; the Association pour la Recherche et les Maladies Hématologiques de l’Enfant (RMHE) research charity; and the AFSE and O-CYTO patient associations.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure of Conflicts of Interest
TP has received a funding support from LFB biomedicaments to attend the 2017 European Hematology Association Annual Meeting. The authors declare that they have no other conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Figure S1
Radiological evolution of the lesions. Each patient’s ID is the upper number and the MRI sequence is the lower statement (T1 gado: T1-weighted sequence post gadolinium injection, FLAIR: T2-weighted sequence fluid-attenuated inversion recovery). The delay after manifestation’s onset is under each figure. (PDF 2642 kb)
Table S1
Complementary exams at neurological involvement (XLSX 305 kb)
Table S2
Pathology findings (XLSX 9 kb)
Table S3
Non-neurological organ involvement (XLSX 12 kb)
Table S4
Immunobiology (XLSX 491 kb)
Rights and permissions
About this article
Cite this article
Pincez, T., Neven, B., Le Pointe, H.D. et al. Neurological Involvement in Childhood Evans Syndrome. J Clin Immunol 39, 171–181 (2019). https://doi.org/10.1007/s10875-019-0594-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10875-019-0594-3