Abstract
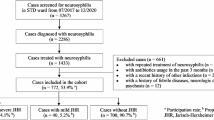
Neurosyphilis (NS) has different clinical manifestations and can appear during any stage of syphilis. We aimed to identify the factors affecting poor outcome in NS patients. Patients with positive cerebrospinal fluid Venereal Disease Research Laboratory test, and positive serological serum treponemal or nontreponemal tests were classified as definite NS. The data of 141 patients with definite NS were submitted from 22 referral centers. Asymptomatic NS, syphilitic meningitis, meningovascular syphilis, tabes dorsalis, general paresis, and taboparesis were detected in 22 (15.6%), 67 (47.5%), 13 (9.2%), 10 (7%), 13 (9.2%), and 16 patients (11.3%), respectively. The number of HIV-positive patients was 43 (30.4%). The most common symptoms were headache (n = 55, 39%), fatigue (n = 52, 36.8%), and altered consciousness (50, 35.4%). Tabetic symptoms were detected in 28 (19.8%), paretic symptoms in 32 (22.6%), and vascular symptoms in 39 patients (27.6%). Eye involvement was detected in 19 of 80 patients (23.7%) who underwent eye examination and ear involvement was detected in eight of 25 patients (32%) who underwent ear examination. Crystallized penicillin was used in 109 (77.3%), procaine penicillin in seven (4.9%), ceftriaxone in 31 (21.9%), and doxycycline in five patients (3.5%). According to multivariate regression analysis, while headache was a protective factor in NS patients, double vision was significantly associated to poor outcome. We concluded that double vision indicated unfavorable outcome among NS patients. A high clinical suspicion is needed for the diagnosis NS. As determined in our study, the presence of headache in syphilitic patients can help in early diagnosis of central nervous system disease.
Similar content being viewed by others
References
Bhai S, Lyons JL (2015) Neurosyphilis update: atypical is the new typical. Curr Infect Dis Rep 17(5):481
Stamm LV (2016) Syphilis: re-emergence of an old foe. Microb Cell 3(9):363–370
Jantzen SU, Ferrea S, Langebner T, Gaebel W, Griese M, Arendt G, Dihne M (2012) Late-stage neurosyphilis presenting with severe neuropsychiatric deficits: diagnosis, therapy, and course of three patients. J Neurol 259(4):720–728
Zhang HL, Lin LR, Liu GL, Zeng YL, Wu JY, Zheng WH, Tong ML, Dong J, Su YH, Liu LL et al (2013) Clinical spectrum of neurosyphilis among HIV-negative patients in the modern era. Dermatology 226(2):148–156
Nyatsanza F, Tipple C (2016) Syphilis: presentations in general medicine. Clin Med (Lond) 16(2):184–188
Brightbill TC, Ihmeidan IH, Post MJ, Berger JR, Katz DA (1995) Neurosyphilis in HIV-positive and HIV-negative patients: neuroimaging findings. AJNR Am J Neuroradiol 16(4):703–711
Hooshmand H, Escobar MR, Kopf SW (1972) Neurosyphilis. A study of 241 patients. JAMA 219(6):726–729
Erdem H, Inan A, Guven E, Hargreaves S, Larsen L, Shehata G, Pernicova E, Khan E, Bastakova L, Namani S et al (2017) The burden and epidemiology of community-acquired central nervous system infections: a multinational study. Eur J Clin Microbiol Infect Dis 36(9):1595–1611
Vanhaecke C, Grange P, Benhaddou N, Blanche P, Salmon D, Parize P, Lortholary O, Caumes E, Pelloux I, Epaulard O et al (2016) Clinical and biological characteristics of 40 patients with neaAurosyphilis and evaluation of Treponema pallidum nested polymerase chain reaction in cerebrospinal fluid samples. Clin Infect Dis 63(9):1180–1186
Drago F, Merlo G, Ciccarese G, Agnoletti AF, Cozzani E, Rebora A, Parodi A (2016) Changes in neurosyphilis presentation: a survey on 286 patients. J Eur Acad Dermatol Venereol 30(11):1886–1900
Control CfD (2014) Prevention: STD surveillance case definitions. Centers for Disease Control and Prevention, Atlanta: http://www.cdc.gov/std/stats/casedefinitions-2014.pdf
Lafond RE, Lukehart SA (2006) Biological basis for syphilis. Clin Microbiol Rev 19(1):29–49
https://www.cdc.gov/std/syphilis/stdfact-syphilis-detailed.htm. Accessed 30 April 2018
Ghanem KG (2010) Review: neurosyphilis: a historical perspective and review. CNS Neurosci Ther 16(5):e157–e168
Wong T, Fonseca K, Chernesky MA, Garceau R, Levett PN, Serhir B (2015) Canadian public health laboratory network laboratory guidelines for the diagnosis of neurosyphilis in Canada. Can J Infect Dis Med Microbiol 26(Suppl A):18A–22A
cdc.gov/std/syphilis/Syphilis-Pocket-Guide-FINAL-508.pdf: Syphilis: a provider’s guide to treatment and prevention. November 30, 2017
Amarenco P CLR, Pessin M (1998) Vertebrobasilar occlusive diseases. In: Barnett HJM, Mohr JP, Stein BM (eds) Stroke Pathophysiology, diagnosis and management, 3rd edn. Churchill Livingstone, pp 513–527
Khamaysi Z, Bergman R, Telman G, Goldsher D (2014) Clinical and imaging findings in patients with neurosyphilis: a study of a cohort and review of the literature. Int J Dermatol 53(7):812–819
Conde-Sendin MA, Amela-Peris R, Aladro-Benito Y, Maroto AA (2004) Current clinical spectrum of neurosyphilis in immunocompetent patients. Eur Neurol 52(1):29–35
Mitsonis CH, Kararizou E, Dimopoulos N, Triantafyllou N, Kapaki E, Mitropoulos P, Sfagos K, Vassilopoulos D (2008) Incidence and clinical presentation of neurosyphilis: a retrospective study of 81 cases. Int J Neurosci 118(9):1251–1257
de Fatima MAMM, Bezerra PC, Guedes DL, Cabral DB, de Barros Miranda-Filho D (2013) Prognostic indicators in bacterial meningitis: a case-control study. Braz J Infect Dis 17(5):538–544
Qu J, Zhou T, Zhong C, Deng R, Lu X (2017) Comparison of clinical features and prognostic factors in HIV-negative adults with cryptococcal meningitis and tuberculous meningitis: a retrospective study. BMC Infect Dis 17(1):51
Dinkin M (2014) Diagnostic approach to diplopia. Continuum (Minneap Minn) 20(4 Neuro-ophthalmology):942–965
Control CD (2015) Prevention: sexually transmitted diseases treatment guidelines, 2015. Ann Emerg Med 66(5):526–528
Shann S, Wilson J (2003) Treatment of neurosyphilis with ceftriaxone. Sex Transm Infect 79(5):415–416
Kang-Birken SL, Castel U, Prichard JG (2010) Oral doxycycline for treatment of neurosyphilis in two patients infected with human immunodeficiency virus. Pharmacotherapy 30(4):119e–122e
Pratas AC, Goldschmidt P, Lebeaux D, Aguilar C, Ermak N, Benesty J, Charlier C, Benveniste E, Merabet L, Sedira N et al (2018) Increase in ocular syphilis cases at ophthalmologic reference center, France, 2012-2015. Emerg Infect Dis 24(2):193–200
Karsan N, Barker R, O'Dwyer JP (2014) Clinical reasoning: the “great imitator”. Neurology 83(22):e188–e196
Funding
We haven’t received support financial for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
We have no competing interests to declare. The neurosyphilis study protocol was approved by Fatih Sultan Mehmet Training and Research Hospital in Istanbul.
Rights and permissions
About this article
Cite this article
Ozturk-Engin, D., Erdem, H., Hasbun, R. et al. Predictors of unfavorable outcome in neurosyphilis: Multicenter ID-IRI Study. Eur J Clin Microbiol Infect Dis 38, 125–134 (2019). https://doi.org/10.1007/s10096-018-3403-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-018-3403-7