Abstract
Purpose
Postoperative pneumonia affects the length of stay and mortality after surgery in elderly patients with colorectal cancer (CRC). We aimed to determine the risk factors of postoperative pneumonia in elderly patients with CRC, and to evaluate the impact of laparoscopic surgery on elderly patients with CRC.
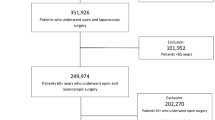
Methods
We retrospectively investigated 1473 patients ≥ 80 years of age who underwent surgery for stage 0–III CRC between 2003 and 2007. Using a multivariate analysis, we determined the risk factors for pneumonia occurrence from each baseline characteristic.
Results
Among all included patients, 26 (1.8%) experienced postoperative pneumonia, and restrictive respiratory impairment, obstructive respiratory impairment, history of cerebrovascular events, and open surgery were determined as risk factors (odds ratio [95% confidence interval], 2.78 [1.22–6.20], 2.71 [1.22–6.30], 3.60 [1.37–8.55], and 3.57 [1.22–15.2], respectively). Furthermore, postoperative pneumonia was more frequently accompanied by increasing cumulative numbers of these risk factors (area under the receiver operating characteristic curve = 0.763).
Conclusions
Laparoscopic surgery may be safely performed in elderly CRC patients, even those with respiratory impairment and a history of cerebrovascular events.




Similar content being viewed by others
References
Balducci L, Beghe C. Cancer and age in the USA. Crit Rev Oncol Hematol. 2001;37(2):137–45.
Repetto L, Balducci L. A case for geriatric oncology. Lancet Oncol. 2002;3(5):289–97.
Anisimov VN, Sikora E, Pawelec G. Relationships between cancer and aging: a multilevel approach. Biogerontology. 2009;10(4):323–38. https://doi.org/10.1007/s10522-008-9209-8.
Japan Statistical Yearbook 2016. Statistics Bureau, Ministry of Internal Affairs and Communications, Japan; 2016.
Cancer Statistics in Japan 2014. Foundation for Promotion of Cancer Research (FPCR). National Cancer Center, The Editorial Board of the Cancer Statistics in Japan; 2015.
Simmonds PD, Best L, George S, Baughan C, Buchanan R, Davis C, et al. Colorectal Cancer Collaborative Group. Surgery for colorectal cancer in elderly patients: a systematic review. Lancet. 2000;356(9234):968–74.
Gurlich R, Maruna P, Kalvach Z, Peskova M, Cermak J, Frasko R. Colon resection in elderly patients: comparison of data of a single surgical department with collective data from the Czech Republic. Arch Gerontol Geriatr. 2005;41(2):183–90. https://doi.org/10.1016/j.archger.2005.02.001.
Marusch F, Koch A, Schmidt U, Steinert R, Ueberrueck T, Bittner R, et al. The impact of the risk factor “age” on the early postoperative results of surgery for colorectal carcinoma and its significance for perioperative management. World J Surg. 2005;29(8):1013–21. https://doi.org/10.1007/s00268-005-7711-6. (discussion 1021–1012).
Turrentine FE, Wang H, Simpson VB, Jones RS. Surgical risk factors, morbidity, and mortality in elderly patients. J Am Coll Surg. 2006;203(6):865–77. https://doi.org/10.1016/j.jamcollsurg.2006.08.026.
Lee L, Jannapureddy M, Albo D, Awad SS, Farrow B, Bellows CC, et al. Outcomes of Veterans Affairs patients older than age 80 after surgical procedures for colon malignancies. Am J Surg. 2007;194(5):646–51. https://doi.org/10.1016/j.amjsurg.2007.08.003.
Rutten HJ, den Dulk M, Lemmens VE, van de Velde CJ, Marijnen CA. Controversies of total mesorectal excision for rectal cancer in elderly patients. Lancet Oncol. 2008;9(5):494–501. https://doi.org/10.1016/s1470-2045(08)70129-3.
Al-Refaie WB, Parsons HM, Habermann EB, Kwaan M, Spencer MP, Henderson WG, et al. Operative outcomes beyond 30-day mortality: colorectal cancer surgery in oldest old. Ann Surg. 2011;253(5):947–52. https://doi.org/10.1097/SLA.0b013e318216f56e.
Panis Y, Maggiori L, Caranhac G, Bretagnol F, Vicaut E. Mortality after colorectal cancer surgery: a French survey of more than 84,000 patients. Ann Surg. 2011;254(5):738–43. https://doi.org/10.1097/SLA.0b013e31823604ac. (discussion 743–734).
Bagshaw PF, Allardyce RA, Frampton CM, Frizelle FA, Hewett PJ, McMurrick PJ, et al. Long-term outcomes of the australasian randomized clinical trial comparing laparoscopic and conventional open surgical treatments for colon cancer: the Australasian Laparoscopic Colon Cancer Study trial. Ann Surg. 2012;256(6):915–9. https://doi.org/10.1097/SLA.0b013e3182765ff8.
Kang SB, Park JW, Jeong SY, Nam BH, Choi HS, Kim DW, et al. Open versus laparoscopic surgery for mid or low rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): short-term outcomes of an open-label randomised controlled trial. Lancet Oncol. 2010;11(7):637–45. https://doi.org/10.1016/s1470-2045(10)70131-5.
Buunen M, Veldkamp R, Hop WC, Kuhry E, Jeekel J, Haglind E, et al. Survival after laparoscopic surgery versus open surgery for colon cancer: long-term outcome of a randomised clinical trial. Lancet Oncol. 2009;10(1):44–52. https://doi.org/10.1016/s1470-2045(08)70310-3.
Lacy AM, Delgado S, Castells A, Prins HA, Arroyo V, Ibarzabal A, et al. The long-term results of a randomized clinical trial of laparoscopy-assisted versus open surgery for colon cancer. Ann Surg. 2008;248(1):1–7. https://doi.org/10.1097/SLA.0b013e31816a9d65.
Jayne DG, Guillou PJ, Thorpe H, Quirke P, Copeland J, Smith AM, et al. Randomized trial of laparoscopic-assisted resection of colorectal carcinoma: 3-year results of the UK MRC CLASICC Trial Group. J Clin Oncol. 2007;25(21):3061–8. https://doi.org/10.1200/jco.2006.09.7758.
Fleshman J, Sargent DJ, Green E, Anvari M, Stryker SJ, Beart RW Jr, et al. Laparoscopic colectomy for cancer is not inferior to open surgery based on 5-year data from the COST Study Group trial. Ann Surg. 2007;246(4):655–62. https://doi.org/10.1097/SLA.0b013e318155a762. (discussion 662–654).
Veldkamp R, Kuhry E, Hop WC, Jeekel J, Kazemier G, Bonjer HJ, et al. Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol. 2005;6(7):477–84. https://doi.org/10.1016/s1470-2045(05)70221-7.
Guillou PJ, Quirke P, Thorpe H, Walker J, Jayne DG, Smith AM, et al. Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet. 2005;365(9472):1718–26. https://doi.org/10.1016/s0140-6736(05)66545-2.
Leung KL, Kwok SP, Lam SC, Lee JF, Yiu RY, Ng SS, et al. Laparoscopic resection of rectosigmoid carcinoma: prospective randomised trial. Lancet. 2004;363(9416):1187–92. https://doi.org/10.1016/s0140-6736(04)15947-3.
Group COoSTS. A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med. 2004;350(20):2050–9. https://doi.org/10.1056/NEJMoa032651.
Lacy AM, Garcia-Valdecasas JC, Delgado S, Castells A, Taura P, Pique JM, et al. Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: a randomised trial. Lancet. 2002;359(9325):2224–9. https://doi.org/10.1016/s0140-6736(02)09290-5.
Stocchi L, Nelson H, Young-Fadok TM, Larson DR, Ilstrup DM. Safety and advantages of laparoscopic vs. open colectomy in the elderly: matched-control study. Dis Colon Rectum. 2000;43(3):326–32.
Sklow B, Read T, Birnbaum E, Fry R, Fleshman J. Age and type of procedure influence the choice of patients for laparoscopic colectomy. Surg Endosc. 2003;17(6):923–9. https://doi.org/10.1007/s00464-002-8949-9.
Frasson M, Braga M, Vignali A, Zuliani W, Di Carlo V. Benefits of laparoscopic colorectal resection are more pronounced in elderly patients. Dis Colon Rectum. 2008;51(3):296–300. https://doi.org/10.1007/s10350-007-9124-0.
Hemandas AK, Abdelrahman T, Flashman KG, Skull AJ, Senapati A, O’Leary DP, et al. Laparoscopic colorectal surgery produces better outcomes for high risk cancer patients compared to open surgery. Ann Surg. 2010;252(1):84–9. https://doi.org/10.1097/SLA.0b013e3181e45b66.
Hinoi T, Kawaguchi Y, Hattori M, Okajima M, Ohdan H, Yamamoto S, et al. Laparoscopic versus open surgery for colorectal cancer in elderly patients: a multicenter matched case-control study. Ann Surg Oncol. 2014. https://doi.org/10.1245/s10434-014-4172-x.
Seymour DG, Vaz FG. A prospective study of elderly general surgical patients: II. Post-operative complications. Age Ageing. 1989;18(5):316–26.
Hall RE, Ash AS, Ghali WA, Moskowitz MA. Hospital cost of complications associated with coronary artery bypass graft surgery. Am J Cardiol. 1997;79(12):1680–2.
Dimick JB, Chen SL, Taheri PA, Henderson WG, Khuri SF, Campbell DA Jr. Hospital costs associated with surgical complications: a report from the private-sector National Surgical Quality Improvement Program. J Am Coll Surg. 2004;199(4):531–7. https://doi.org/10.1016/j.jamcollsurg.2004.05.276.
Qaseem A, Snow V, Fitterman N, Hornbake ER, Lawrence VA, Smetana GW, et al. Risk assessment for and strategies to reduce perioperative pulmonary complications for patients undergoing noncardiothoracic surgery: a guideline from the American College of Physicians. Ann Intern Med. 2006;144(8):575–80.
Smetana GW. Postoperative pulmonary complications: an update on risk assessment and reduction. Clevel Clin J Med. 2009;76(Suppl 4):S60–65. https://doi.org/10.3949/ccjm.76.s4.10.
Sobin LHGM, Wittekind C. TNM classification of malignant tumors. 7th ed. Oxford: Wiley-Blackwell; 2009.
Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982;5(6):649–55.
Niitsu H, Hinoi T, Kawaguchi Y, Ohdan H, Hasegawa H, Suzuka I, et al. Laparoscopic surgery for colorectal cancer is safe and has survival outcomes similar to those of open surgery in elderly patients with a poor performance status: subanalysis of a large multicenter case-control study in Japan. J Gastroenterol. 2015. https://doi.org/10.1007/s00535-015-1083-y.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13.
Acknowledgements
We appreciate the support with the statistical analyses provided by Minoru Hattori, Advanced Medical Skills Training Center, Hiroshima University, and we owe our deepest gratitude to the following members of the Japan Society of Laparoscopic Colorectal Surgery for their cooperation: Eiji Kanehira, Kunihisa Shiozawa, Ageo Central General Hospital; Daisuke Yamamoto, Ishikawa Prefectural Central Hospital; Seigo Kitano, Tomonori Akagi, Oita University; Junji Okuda, Keitaro Tanaka, Osaka Medical College; Masayoshi Yasui, Osaka National Hospital; Kosei Hirakawa, Kiyoshi Maeda, Osaka City University; Akiyoshi Kanazawa, Osaka Red Cross Hospital; Junichi Hasegawa, Junichi Nishimura, Osaka Rosai Hospital; Ichio Suzuka, Kagawa Prefectural Central Hospital; Shintaro Akamoto, Kagawa University; Masashi Ueno, Yosuke Fukunaga, Hiroya Kuroyanagi, Cancer Institute Hospital; Masaki Naito, Kitasato University; Hiroyuki Bando, Ishikawa Prefectural Central Hospital; Takashi Yamaguchi, Kyoto Medical Center; Yoshiharu Sakai, Koya Hida, Yousuke Kinjo, Kyoto University; Masayoshi Nakanishi, Yukihito Kokuba, Kyoto Prefectural University; Hirotoshi Hasegawa, Keio University; Madoka Hamada, Kochi Health Sciences Center; Norio Saito, National Cancer Hospital East; Seiichiro Yamamoto, National Cancer Center Hospital; Tomohisa Furuhata, Kenji Okita, Sapporo Medical University; Shuji Saito, Shizuoka Cancer Center; Hisanaga Horie, Jichi Medical University; Kazuhiro Sakamoto, Michitoshi Goto, Juntendo University; Junichi Tanaka, Shungo Endo, Showa University Northern Yokohama Hospital; Yoshihito Ide, Kohei Murata, Suita Municipal Hospital; Nobuyoshi Miyajima, Tadashi Suda, Tsukasa Shimamura, St. Marianna University; Yoshihisa Saida, Toshiyuki Enomoto, Toho University Ohashi Medical Center; Takeshi Naito, Tohoku University; Yasuhiro Munakata, Ken Hayashi, Soichi Tagami, Nagano Municipal Hospital; Yasukimi Takii, Satoshi Maruyama, Niigata Cancer Center Hospital; Takao Ichihara, Nishinomiya Municipal Central Hospital; Hitoshi Idani, Yohei Kurose, Fukuyama City Hospital; Yasuhiro Miyake, Minoh City Hospital; Shoichi Hazama, Yamaguchi University; Kazuteru Watanabe, Shoich Fujii, Shigeru Yamagishi, Yokohama City University Medical Center; Yasuo Kawaguchi, Hiroshima University; Masazumi Okajima, Hiroshima City Hiroshima Citizens Hospital; and Kenichi Sugihara, Tokyo Medical and Dental University Graduate School. This study was supported by the Japanese Society for Cancer of the Colon and Rectum.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
Masaaki Ito declares stock ownership in A-traction, Inc. (300 shares.) All other authors have no conflicts of interest to declare.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kochi, M., Hinoi, T., Niitsu, H. et al. Risk factors for postoperative pneumonia in elderly patients with colorectal cancer: a sub-analysis of a large, multicenter, case-control study in Japan. Surg Today 48, 756–764 (2018). https://doi.org/10.1007/s00595-018-1653-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-018-1653-8