Abstract
Purpose
A study was conducted to clarify the actual status of nutrition management after gastric cancer surgery in Japan and obtain basic data for optimizing perioperative nutrition management.
Methods
A questionnaire was sent to 354 hospitals with at least 50 cases of gastric cancer surgery per year. Questions included the perioperative nutrition management and length of hospital stay for patients who underwent gastric cancer surgery within three months of the survey.
Results
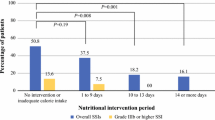
Responses were obtained from 242 hospitals (68%; 20,858 patients). Nutrition management was consistent between laparotomy and laparoscopic surgery for 84% of respondents. The number of postoperative days was the most commonly chosen index for starting oral feeding. The most commonly chosen index for hospital dischargeability was diet composition/amount consumed in 182 hospitals (44%), followed by laboratory data stabilization in 106 hospitals (26%), and the number of postoperative days in 87 hospitals (21%). A positive correlation was found between the mean length of postoperative hospital stay and starting oral feeding (r = 0.23 for distal gastrectomy; r = 0.34 for total gastrectomy). The length of hospital stay tended to be shorter with an earlier start of oral feeding (p < 0.01).
Conclusion
Early postoperative oral feeding may be a factor in reducing the length of hospital stay after gastric cancer surgery.







Similar content being viewed by others
References
Fearon KC, Ljungqvist O, Von Meyenfeldt M, Revhaug A, Dejong CH, Lassen K, et al. Enhanced recovery after surgery: a consensus review of clinical care for patients undergoing colonic resection. Clin Nutr. 2005;24:466–77.
Lassen K, Coolsen MM, Slim K, Carli F, de Aguilar-Nascimento JE, Schäfer M, et al. Guideline for perioperative care for pancreaticoduodenectomy: enhanced recovery after surgery (ERAS®) society recommendations. Clin Nutr. 2012;31:817–30.
Coolsen MM, Wong-Lun-Hing EM, van Dam RM, van der Wilt AA, Slim K, Lassen K, et al. A systematic review of outcomes in patients undergoing liver surgery in an enhanced recovery after surgery pathways. HPB (Oxford). 2013;15:245–51.
Mortensen K, Nilsson M, Slim K, Schäfer M, Mariette C, Braga M, et al. Consensus guideline for enhanced recovery after gastrectomy: enhanced recovery after surgery (ERAS®) society recommendations. Br J Surg. 2014;101:1209–29.
Suehiro T, Matsumata T, Shikada Y, Sugimachi K. Accelerated rehabilitation with early postoperative oral feeding following gastrectomy. Hepatogastroenterology. 2004;51:1852–5.
Hirao M, Tsujinaga T, Takeno A, Fujitani K, Kurata M. Patient-controlled dietary schedule improves clinical outcome after gastrectomy for gastric cancer. World J Surg. 2005;29:853–7.
Yamada T, Hayashi T, Cho H, Yoshikawa T, Taniguchi H, Fukushima R, et al. Usefulness of enhanced recovery after surgery protocol as compared with conventional perioperative care in gastric surgery. Gastric Cancer. 2012;15:34–41.
Sugisawa N, Tokunaga M, Makuuchi R, Miki Y, Tanizawa Y, Bando E, et al. A phase II study of an enhanced recovery after surgery protocol in gastric cancer surgery. Gastric Cancer. 2016;19:961–7.
Ota H, Ikenaga M, Hasegawa J, Murata K, Miyake Y, Mizushima T, et al. Safety and efficacy of an “enhanced recovery after surgery” protocol for patients undergoing colon cancer surgery: a multi-institutional controlled study. Surg Today. 2016;. doi:10.1007/s00595-016-1423-4.
Seo HS, Song KY, Jeon HM, Park CH. The impact of an increased application of critical pathway for gastrectomy on the length of stay and cost. J Gastric Cancer. 2012;12:126–31.
Kreys ED, Koeller JM. Documenting the benefits and cost saving of a large multistate cancer pathway program from a payer’s perspective. J Oncol Pract. 2013;9:e241–7.
Jones DE, Sutcliffe K, Pairman J, Willton K, Newton JL. An integrated care pathway improves quality of life in primary biliary cirrhosis. QJM. 2008;101:535–43.
Association Japanese Gastric Cancer. Gastric cancer treatment guidelines 2014 (ver. 4). Gastric Cancer. 2017;20:1–19.
Kumagai K, Shimizu K, Yokoyama N, Aida S, Arima S, Aikou T, et al. Questionnaire survey regarding the current status and controversial issues concerning reconstruction after gastrectomy in Japan. Surg Today. 2012;42:411–8.
Association Japanese Gastric Cancer. Gastric cancer treatment guidelines 2010 (ver. 3). Gastric Cancer. 2011;14:113–23.
Kurokawa Y, Katai H, Fukuda H, Sasako M, Gastric Cancer Surgical Study Group of the Japan Clinical Oncology Group. Phase II study of laparoscopy-assisted distal gastrectomy with nodal dissection for clinical stage I gastric cancer: Japan Clinical Oncology Group Study JCOG0703. Jpn J Clin Oncol. 2008;38:501–3.
Katai H, Sasako M, Fukuda H, Nakamura K, Hiki N, Saka M, et al. Safety and feasibility of laparoscopy-assisted distal gastrectomy with suprapancreatic nodal dissection for clinical stage I gastric cancer: a multicenter phase II trial (JCOG 0703). Gastric Cancer. 2010;13:238–44.
Laviano A, Meguid MM, Inui A, Muscaritoli M, Rossi-Fanelli F. Therapy insight: cancer anorexia-cachexia syndrome–when all you can eat is yourself. Nat Clin Pract Oncol. 2005;2:158–65.
Liedman B, Andersson H, Bosaeus I, Hugosson I, Lundell L. Changes in body composition after gastrectomy: results of a controlled, prospective clinical trial. World J Surg. 1997;21:416–20.
Davis JL, Selby LV, Chou JF, Schattner M, Ilson DH, Capanu M, et al. Patterns and predictors of weight loss after gastrectomy for cancer. Ann Surg Oncol. 2016;23:1639–45.
Rino Y, Oshima T, Yoshikawa T. Changes in fat-soluble vitamin levels after gastrectomy for gastric cancer. Surg Today. 2017;47:145–50.
Ri M, Miyata H, Aikou S, Seto Y, Akazawa K, Takeuchi M, et al. Effect of body mass index (BMI) on surgical outcomes: a nationwide survey using a Japanese web-based database. Surg Today. 2015;45:1271–9.
Okamura Y, Sugiura T, Ito T, Yamamoto Y, Ashida R, Uesaka K. The optimal cut-off value of the preoperative prognostic nutritional index for the survival differs according to the TNM stage in hepatocellular carcinoma. Surg Today. 2017;. doi:10.1007/s00595-017-1491-0.
Lee HO, Han SR, Choi SI, Lee JJ, Kim SH, Ahn HS, et al. Effects of intensive nutrition education on nutritional status and quality of life among postoperative gastrectomy patients. Ann Surg Treat Res. 2016;90:79–88.
Acknowledgements
The authors thank the medical institutions listed in the Online Resource for their cooperation in the study. This study was conducted on a research contract from EN Otsuka Pharmaceutical Co., Ltd.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors and corresponding authors have no conflicts of interest for EN Otsuka Pharmaceutical Co., Ltd.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Shimizu, N., Hatao, F., Fukatsu, K. et al. Results of a nationwide questionnaire-based survey on nutrition management following gastric cancer resection in Japan. Surg Today 47, 1460–1468 (2017). https://doi.org/10.1007/s00595-017-1552-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-017-1552-4