Abstract
Purpose
To prevent perinatal morbidity and mortality of high-order multiple pregnancy (HOMP), multifetal pregnancy reduction (MPR) is offered to some patients. In this study, we investigated whether twin pregnancies derived from MPRs carry a higher adverse obstetrical outcome compared to non-reduced control group of twins.
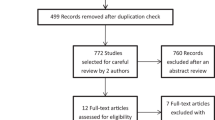
Methods
We retrospectively analyzed the data from HOMPs on which transvaginal ER (n = 153) at a mean gestational age of 7.6 weeks or transabdominal FR (n = 59) at a mean gestational age of 12.4 weeks was performed between December 2006 and January 2018. The risk of each procedure was evaluated by comparing obstetrical outcome with that of a control population of 157 non-reduced twins conceived by infertility treatment.
Results
The mean gestational ages at delivery were 35.2 weeks in the ER group, 35.7 weeks in the FR group, and 34.1 weeks in the control group (P = NS). Compared with those in the control group, the ER group had higher miscarriage (1.3% vs. 6.5%; P = 0.047; OR 0.21; 95% CI 0.45–0.898) and higher overall fetal loss (3.8% vs. 14.4%; P = 0.003; OR 0.24; 95% CI 0.09–0.60) rates. Differently compared with those in the control group, the FR group had no statistical difference in miscarriage (2.5% vs. 1.7%; P=NS) and overall fetal loss (3.8% vs. 6.8%; P=NS) rates.
Conclusions
Compared with the control group, ER in twins had a higher miscarriage and fetal loss rate, whereas FR in twins was similar to the control group. So, the FR procedure is overall a better and safer approach of MPR in reducing morbidity and mortality in HOMPs.



Similar content being viewed by others
References
No Committee Opinion, 719 (2017) Multifetal pregnancy reduction. Obstet Gynecol 130(3):e158–e163. https://doi.org/10.1097/aog.0000000000002302
Garg P, Abdel-Latif ME, Bolisetty S, Bajuk B, Vincent T, Lui K (2010) Perinatal characteristics and outcome of preterm singleton, twin and triplet infants in NSW and the ACT, Australia (1994–2005). Arch Dis Child Fetal Neonatal Ed 95(1):F20–24. https://doi.org/10.1136/adc.2009.157701
Qin JB, Sheng XQ, Wang H, Chen GC, Yang J, Yu H, Yang TB (2017) Worldwide prevalence of adverse pregnancy outcomes associated with in vitro fertilization/intracytoplasmic sperm injection among multiple births: a systematic review and meta-analysis based on cohort studies. Arch Gynecol Obstet 295(3):577–597. https://doi.org/10.1007/s00404-017-4291-2
Zipori Y, Haas J, Berger H, Barzilay E (2017) Multifetal pregnancy reduction of triplets to twins compared with non-reduced triplets: a meta-analysis. Reprod Biomed Online 35(3):296–304. https://doi.org/10.1016/j.rbmo.2017.05.012
Kim MS, Choi DH, Kwon H, Ahn E, Cho HY, Baek MJ, Shin JE, Moon MJ (2018) Procedural and obstetrical outcomes after embryo reduction or fetal reduction in multifetal pregnancies: a retrospective study. Ultrasound Obstet Gynecol. https://doi.org/10.1002/uog.19024
Dodd J, Crowther C (2004) Multifetal pregnancy reduction of triplet and higher-order multiple pregnancies to twins. Fertil Steril 81(5):1420–1422. https://doi.org/10.1016/j.fertnstert.2003.11.028
Egbe TO, Sandjon G, Ourtchingh C, Simo A, Priso EB, Benifla JL (2016) In-vitro fertilization and spontaneous pregnancies: matching outcomes in Douala Cameroon. Fertil Res Pract 2:1. https://doi.org/10.1186/s40738-015-0013-2
Chung K, Coutifaris C, Chalian R, Lin K, Ratcliffe SJ, Castelbaum AJ, Freedman MF, Barnhart KT (2006) Factors influencing adverse perinatal outcomes in pregnancies achieved through use of in vitro fertilization. Fertil Steril 86(6):1634–1641. https://doi.org/10.1016/j.fertnstert.2006.04.038
Hansen M, Colvin L, Petterson B, Kurinczuk JJ, de Klerk N, Bower C (2009) Twins born following assisted reproductive technology: perinatal outcome and admission to hospital. Hum Reprod 24(9):2321–2331. https://doi.org/10.1093/humrep/dep173
Salomon LJ, Alfirevic Z, Bilardo CM, Chalouhi GE, Ghi T, Kagan KO, Lau TK, Papageorghiou AT, Raine-Fenning NJ, Stirnemann J, Suresh S, Tabor A, Timor-Tritsch IE, Toi A, Yeo G (2013) ISUOG practice guidelines: performance of first-trimester fetal ultrasound scan. Ultrasound Obstet Gynecol 41(1):102–113. https://doi.org/10.1002/uog.12342
Evans MI, Berkowitz RL, Wapner RJ, Carpenter RJ, Goldberg JD, Ayoub MA, Horenstein J, Dommergues M, Brambati B, Nicolaides KH, Holzgreve W, Timor-Tritsch IE (2001) Improvement in outcomes of multifetal pregnancy reduction with increased experience. Am J Obstet Gynecol 184(2):97–103. https://doi.org/10.1067/mob.2001.108074
Stone J, Ferrara L, Kamrath J, Getrajdman J, Berkowitz R, Moshier E, Eddleman K (2008) Contemporary outcomes with the latest 1000 cases of multifetal pregnancy reduction (MPR). Am J Obstet Gynecol 199 (4):406 e401–404. https://doi.org/10.1016/j.ajog.2008.06.017
Hershko-Klement A, Lipitz S, Wiser A, Berkovitz A (2013) Reduced versus nonreduced twin pregnancies: obstetric performance in a cohort of interventional conceptions. Fertil Steril 99(1):163–167. https://doi.org/10.1016/j.fertnstert.2012.09.005
Evans MI, Ciorica D, Britt DW, Fletcher JC (2005) Update on selective reduction. Prenat Diagn 25(9):807–813. https://doi.org/10.1002/pd.1261
Timor-Tritsch IE, Bashiri A, Monteagudo A, Rebarber A, Arslan AA (2004) Two hundred ninety consecutive cases of multifetal pregnancy reduction: comparison of the transabdominal versus the transvaginal approach. Am J Obstet Gynecol 191(6):2085–2089. https://doi.org/10.1016/j.ajog.2004.05.024
Coffler MS, Kol S, Drugan A, Itskovitz-Eldor J (1999) Early transvaginal embryo aspiration: a safer method for selective reduction in high order multiple gestations. Hum Reprod 14(7):1875–1878
Haas J, Barzilay E, Hourvitz A, Dor J, Lipitz S, Yinon Y, Shlomi M, Shulman A (2016) Outcome of early versus late multifetal pregnancy reduction. Reprod Biomed Online 33(5):629–634. https://doi.org/10.1016/j.rbmo.2016.08.015
Sun L, Jiang LX, Chen HZ (2017) Obstetric outcome of vanishing twins syndrome: a systematic review and meta-analysis. Arch Gynecol Obstet 295(3):559–567. https://doi.org/10.1007/s00404-017-4289-9
Bhandari S, Ganguly I, Agrawal P, Bhandari S, Singh A, Gupta N (2016) Comparative analysis of perinatal outcome of spontaneous pregnancy reduction and multifetal pregnancy reduction in triplet pregnancies conceived after assisted reproductive technique. J Hum Reprod Sci 9(3):173–178. https://doi.org/10.4103/0974-1208.192058
Dickey RP, Taylor SN, Lu PY, Sartor BM, Storment JM, Rye PH, Pelletier WD, Zender JL, Matulich EM (2002) Spontaneous reduction of multiple pregnancy: incidence and effect on outcome. Am J Obstet Gynecol 186(1):77–83
Zhang YL, Wang XY, Wang F, Su YC, Sun YP (2015) Clinical analysis of spontaneous pregnancy reduction in the patients with multiple pregnancies undergoing in vitro fertilization/intracytoplasmic sperm injection-embryo transfer. Int J Clin Exp Med 8(3):4575–4580
Mansour RT, Aboulghar MA, Serour GI, Sattar MA, Kamal A, Amin YM (1999) Multifetal pregnancy reduction: modification of the technique and analysis of the outcome. Fertil Steril 71(2):380–384
Haas J, Hourvitz A, Dor J, Elizur S, Yinon Y, Barzilay E, Shulman A (2014) Perinatal outcome of twin pregnancies after early transvaginal multifetal pregnancy reduction. Fertil Steril 101(5):1344–1348. https://doi.org/10.1016/j.fertnstert.2014.01.032
Stone J, Belogolovkin V, Matho A, Berkowitz RL, Moshier E, Eddleman K (2007) Evolving trends in 2000 cases of multifetal pregnancy reduction: a single-center experience. Am J Obstet Gynecol 197 (4):394 e391–394. https://doi.org/10.1016/j.ajog.2007.06.056
Cheang CU, Huang LS, Lee TH, Liu CH, Shih YT, Lee MS (2007) A comparison of the outcomes between twin and reduced twin pregnancies produced through assisted reproduction. Fertil Steril 88(1):47–52. https://doi.org/10.1016/j.fertnstert.2006.11.084
Antsaklis AJ, Drakakis P, Vlazakis GP, Michalas S (1999) Reduction of multifetal pregnancies to twins does not increase obstetric or perinatal risks. Hum Reprod 14(5):1338–1340
Hwang JL, Pan HS, Huang LW, Lee CY, Tsai YL (2002) Comparison of the outcomes of primary twin pregnancies and twin pregnancies following fetal reduction. Arch Gynecol Obstet 267(2):60–63. https://doi.org/10.1007/s00404-001-0279-y
Selam B, Lembet A, Stone J, Lapinski R, Berkowitz RL (1999) Pregnancy complications and neonatal outcomes in multifetal pregnancies reduced to twins compared with nonreduced twin pregnancies. Am J Perinatol 16(2):65–71. https://doi.org/10.1055/s-2007-993838
Lipitz S, Uval J, Achiron R, Schiff E, Lusky A, Reichman B (1996) Outcome of twin pregnancies reduced from triplets compared with nonreduced twin gestations. Obstet Gynecol 87(4):511–514. https://doi.org/10.1016/0029-7844(95)00469-6
Funding
None.
Author information
Authors and Affiliations
Contributions
MSK: Manuscript writing, SK: Protocol/project development, data management, EDN: Manuscript writing/editing, JI: Data collection, EA: Data analysis, JES: Data collection, MJM: Protocol/project development.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kim, M.S., Kang, S., Na, E.D. et al. Obstetrical outcomes of embryo reduction and fetal reduction compared to non-reduced twin pregnancies. Arch Gynecol Obstet 299, 953–960 (2019). https://doi.org/10.1007/s00404-019-05089-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-019-05089-w