Abstract
Background
Increased age, obesity, and American Society of Anesthesiologists (ASA) Physical Status class III and IV have been reported as predictors for mortality and perioperative complications. High-volume institutions rely on central referral services as first contact point for patients. The current study reports on a simple four-step questionnaire to identify patients with ASA-physical status class III and IV to improve referral processes and optimize perioperative work ups.
Materials and methods
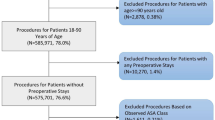
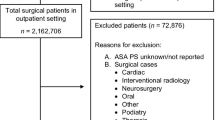
Seven hundred and seventy-five patients who called the physician referral service (PRS) at the author’s institution and subsequently underwent surgery were enrolled in this study. The answers to the initial PRS questionnaire were analyzed. The study cohort consisted of 414 women (53.4%) and 361 men (46.6%) with an average age of 61.4 years (range 44–90 years) at the time of surgery.
Results
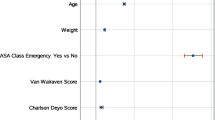
Binary logistic regression revealed hypertension, diabetes mellitus (using medication), using blood thinner (other than Aspirin) and a number of 4–9 prescribed medication, respectively, as predictors for ASA III and IV. Receiver-operating characteristic (ROC) curve analysis identified a sensitivity of 82.4%, a specificity of 82.9%, and an accuracy of 82.8%, when two of these four questions are answered “yes”. The area under the curve for this analysis was 0.876 [95% confidence interval (CI) 0.845–0.908]. Positive and negative likelihood ratios were 4.8 (95% CI 4.0–5.8) and 0.2 (95% CI 0.1–0.3), respectively.
Conclusions
This study revealed a simple four-step questionnaire to identify patients with ASA III or IV before a medical appointment. This helps to balance referrals between multiple providers in high-volume medical groups.


Similar content being viewed by others
References
Vaupel JW (2010) Biodemography of human ageing. Nature 464(7288):536–542. https://doi.org/10.1038/nature08984
Huddleston JI, Wang Y, Uquillas C, Herndon JH, Maloney WJ (2012) Age and obesity are risk factors for adverse events after total hip arthroplasty. Clin Orthop Relat Res 470(2):490–496. https://doi.org/10.1007/s11999-011-1967-y
Ibrahim SA, Stone RA, Han X, Cohen P, Fine MJ, Henderson WG, Khuri SF, Kwoh CK (2005) Racial/ethnic differences in surgical outcomes in veterans following knee or hip arthroplasty. Arthritis Rheum 52(10):3143–3151. https://doi.org/10.1002/art.21304
Mahomed NN, Barrett JA, Katz JN, Phillips CB, Losina E, Lew RA, Guadagnoli E, Harris WH, Poss R, Baron JA (2003) Rates and outcomes of primary and revision total hip replacement in the United States medicare population. J Bone Jt Surg Am 85-a(1):27–32
Parvizi J, Johnson BG, Rowland C, Ereth MH, Lewallen DG (2001) Thirty-day mortality after elective total hip arthroplasty. J Bone Jt Surg Am 83-a(10):1524–1528
Perka C, Arnold U, Buttgereit F (2000) Influencing factors on perioperative morbidity in knee arthroplasty. Clin Orthop Relat Res 378:183–191
Feng B, Lin J, Jin J, Qian WW, Wang W, Weng XS (2017) Thirty-day postoperative complications following primary total knee arthroplasty: a retrospective study of incidence and risk factors at a single center in China. Chin Med J 130(21):2551–2556. https://doi.org/10.4103/0366-6999.213071
Sun K, Li H (2017) Body mass index as a predictor of outcome in total knee replace: a systemic review and meta-analysis. Knee 24(5):917–924. https://doi.org/10.1016/j.knee.2017.05.022
George J, Piuzzi NS, Ng M, Sodhi N, Khlopas AA, Mont MA (2018) Association between body mass index and thirty-day complications after total knee arthroplasty. J Arthroplasty 33(3):865–871. https://doi.org/10.1016/j.arth.2017.09.038
Alvi HM, Mednick RE, Krishnan V, Kwasny MJ, Beal MD, Manning DW (2015) The effect of BMI on 30 day outcomes following total joint arthroplasty. J Arthroplasty 30(7):1113–1117. https://doi.org/10.1016/j.arth.2015.01.049
Saklad MDM (1941) Grading of patients for surgical procedures. Anesthesiology 2(3):281–284
Dripps RD (1963) New classification of physical status. Anesthesiology 24:111
Dripps RD, Lamont A, Eckenhoff JE (1961) The role of anesthesia in surgical mortality. JAMA 178(3):261–266. https://doi.org/10.1001/jama.1961.03040420001001
Hooper GJ, Rothwell AG, Hooper NM, Frampton C (2012) The relationship between the American Society Of Anesthesiologists physical rating and outcome following total hip and knee arthroplasty: an analysis of theNew Zealand Joint Registry. J Bone Jt Surg Am 94(12):1065–1070. https://doi.org/10.2106/jbjs.J.01681
Jolles BM, Zangger P, Leyvraz PF (2002) Factors predisposing to dislocation after primary total hip arthroplasty: a multivariate analysis. J Arthroplasty 17(3):282–288
Ridgeway S, Wilson J, Charlet A, Kafatos G, Pearson A, Coello R (2005) Infection of the surgical site after arthroplasty of the hip. J Bone Jt Surg Br 87(6):844–850. https://doi.org/10.1302/0301-620x.87b6.15121
Clelland C, Worland RL, Jessup DE, East D (1996) Preoperative medical evaluation in patients having joint replacement surgery: added benefits. South Med J 89(10):958–960
Schwarzkopf R, Katz G, Walsh M, Lafferty PM, Slover JD (2011) Medical clearance risk rating as a predictor of perioperative complications after total hip arthroplasty. J Arthroplasty 26(1):36–40. https://doi.org/10.1016/j.arth.2010.03.012
Schaeffer JF, Scott DJ, Godin JA, Attarian DE, Wellman SS, Mather RC (2015) The association of ASA class on total knee and total hip arthroplasty readmission rates in an academic hospital. J Arthroplasty 30(5):723–727. https://doi.org/10.1016/j.arth.2014.12.014
Singh JA, Jensen MR, Harmsen WS, Gabriel SE, Lewallen DG (2011) Cardiac and thromboembolic complications and mortality in patients undergoing total hip and total knee arthroplasty. Ann Rheum Dis 70(12):2082–2088. https://doi.org/10.1136/ard.2010.148726
Farrar JT, Young JP Jr, LaMoreaux L, Werth JL, Poole RM (2001) Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain 94(2):149–158
Jaeschke R, Guyatt GH, Sackett DL (1994) Users’ guides to the medical literature. III. How to use an article about a diagnostic test. B. What are the results and will they help me in caring for my patients? The evidence-based medicine working group. JAMA 271(9):703–707
Inneh IA, Lewis CG, Schutzer SF (2014) Focused risk analysis: regression model based on 5314 total hip and knee arthroplasty patients from a single institution. J Arthroplasty 29(10):2031–2035. https://doi.org/10.1016/j.arth.2014.05.007
Garland A, Rolfson O, Garellick G, Karrholm J, Hailer NP (2015) Early postoperative mortality after simultaneous or staged bilateral primary total hip arthroplasty: an observational register study from the Swedish Hip Arthroplasty Register. BMC Musculoskelet Disord 16:77. https://doi.org/10.1186/s12891-015-0535-0
Husted H, Holm G, Jacobsen S (2008) Predictors of length of stay and patient satisfaction after hip and knee replacement surgery: fast-track experience in 712 patients. Acta Orthop 79(2):168–173. https://doi.org/10.1080/17453670710014941
Parvizi J, Mui A, Purtill JJ, Sharkey PF, Hozack WJ, Rothman RH (2007) Total joint arthroplasty: When do fatal or near-fatal complications occur? J Bone Jt Surg Am 89(1):27–32. https://doi.org/10.2106/jbjs.E.01443
Koh IJ, Kim GH, Kong CG, Park SW, Park TY, In Y (2015) The patient’s age and American Society of anesthesiologists status are reasonable criteria for deciding whether to perform same-day bilateral TKA. J Arthroplasty 30(5):770–775. https://doi.org/10.1016/j.arth.2014.12.004
Dale H, Skramm I, Lower HL, Eriksen HM, Espehaug B, Furnes O, Skjeldestad FE, Havelin LI, Engesaeter LB (2011) Infection after primary hip arthroplasty: a comparison of 3 Norwegian health registers. Acta Orthop 82(6):646–654. https://doi.org/10.3109/17453674.2011.636671
Bieger R, Kappe T, Fraitzl CR, Reichel H (2013) The aetiology of total knee arthroplasty failure influences the improvement in knee function. Arch Orthop Trauma Surg 133(2):237–241. https://doi.org/10.1007/s00402-012-1647-8
Dietrich M, Zingg PO, Egbring M, Kamath AF, Dora C (2015) Pre-hospital medications in total hip arthroplasty: risk factors for poor outcomes. Hip Int 25(3):215–220. https://doi.org/10.5301/hipint.5000227
Schaller G, Black J, Asaad A, Harper N, Webb S, Muirhead-Allwood S (2015) Primary collared uncemented total hip arthroplasties in the elderly: a safe and reliable treatment option. J Arthroplasty 30(3):407–410. https://doi.org/10.1016/j.arth.2014.10.004
Choi HR, Bedair H (2014) Mortality following revision total knee arthroplasty: a matched cohort study of septic versus aseptic revisions. J Arthroplasty 29(6):1216–1218. https://doi.org/10.1016/j.arth.2013.11.026
Mak PH, Campbell RC, Irwin MG (2002) The ASA physical status classification: inter-observer consistency. American Society of anesthesiologists. Anaesth Intensive Care 30(5):633–640
Ranta S, Hynynen M, Tammisto T (1997) A survey of the ASA physical status classification: significant variation in allocation among Finnish anaesthesiologists. Acta Anaesthesiol Scand 41(5):629–632
Rius C, Perez G, Martinez JM, Bares M, Schiaffino A, Gispert R, Fernandez E (2004) An adaptation of Charlson comorbidity index predicted subsequent mortality in a health survey. J Clin Epidemiol 57(4):403–408. https://doi.org/10.1016/j.jclinepi.2003.09.016
Funding
No external funding was received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Boettner has received royalties by Smith and Nephew and Orthodevelopment. Dr. Boettner has also received compensation by Smith and Nephew, Orthodevelopment, and DePuy. All other authors have no conflict of interest.
Research involving human participants and/or animals
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Additional information
Investigation performed at Hospital for Special Surgery, New York, NY
Rights and permissions
About this article
Cite this article
Springer, B., Bechler, U., Kolodny, A. et al. Four questions to identify patients with ASA III or higher. Arch Orthop Trauma Surg 139, 461–466 (2019). https://doi.org/10.1007/s00402-018-3078-7
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-018-3078-7