Abstract
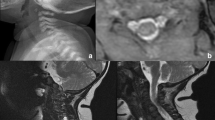
Although relatively rare, post-operative nerve injuries may occur after cervical spine procedures. The most common post-operative neural disorder is C5 nerve palsy. The risk factors for C5 nerve palsy are male gender, OPLL, and posterior cervical approaches. It generally presents with deltoid and/or biceps weakness, and may present immediately or several days after surgery. Treatment is generally conservative due to transient duration of symptoms, but evaluation of residual compression at C4–5 is essential. PTS (Parsonage-Turner syndrome) is an idiopathic plexopathy generally presenting with severe neuropathic pain in the shoulder, neck, and arms, followed by neurological deficits involving the upper brachial plexus. The deficits typically present in a delayed fashion after the onset of pain. Once residual nerve compression is ruled out, initial treatment is based on pain control and physical therapy. Post-operative C8-T1 nerve palsies occur with weakness of the five intrinsic muscles of the hand innervated by the medial nerve, with sensory symptoms in the territory innervated by the ulnar nerve (ulnar two digits of the hand), and also the medial forearm. The risk factors for C8-T1 nerve injuries after surgery are C7 pedicle subtraction osteotomies and posterior fixation of the cervico-thoracic junction, especially in patients with preoperative C7-T1 stenosis. A wide foraminal decompression at C7-T1 region is necessary to minimize risk of this complication. Finally, Horner’s syndrome can occur post-operatively, especially after anterolateral approaches to the middle and lower levels of the cervical spine. It is characterized by ipsilateral papillary miosis, facial anhydrosis, and ptosis secondary to injury of the cervical sympathetic nerves. Avoid using the cautery on the lateral border of the longus colli muscle, where the sympathetic chain lies and place the retractors properly underneath the muscle to decrease the chance of sympathetic injuries. It can also occur from iatrogenic compression or injury to the T1 nerve root, as the sympathetic chain gets some of its fibers from that level. Understanding the most common potential nerve injuries after cervical spine procedures is helpful in prevention, early diagnosis, and appropriate management.
Similar content being viewed by others
Abbreviations
- OPLL:
-
Ossification of the posterior longitudinal ligament
- PTS:
-
Parsonage-Turner syndrome
- EMG:
-
Electroneuromyography
References
Daniels AH, Hart RA, Hilibrand AS, Fish DE, Wang JC, Lord EL et al (2017) Iatrogenic spinal cord injury resulting from cervical spine surgery. Global Spine J 7(1):84S–90S
Than KD, Mummaneni PV, Smith ZA, Hsu WK, Arnold PM, Fehlings MG et al (2017) Brachial plexopathy after cervical spine surgery. Global Spine J 7(1):17S–20S
Thompson SE, Smith ZA, Hsu WK, Nassr A, Mroz TE, Fish DE (2017) C5 palsy after cervical spine surgery: a multicenter retrospective review of 59 cases. Global Spine J 7(1):64S–70S
Traynelis VC, Malone HR, Smith ZA, Hsu WK, Kanter AS, Qureshi SA (2017) Rare complications of cervical spine surgery: Horner’s syndrome. Global Spine J 7(1):103S–108S
Liu G, Reyes R, Riew KD (2017) Why does C5 palsy occur after prophylactic bilateral C4-5 foraminotomy in open-door cervical laminoplasty? A risk factor analysis. Global Spine J 7(7):696–702
Bydon M, Macki M, Kaloostian P et al (2014) Incidence and prognostic factors of c5 palsy: a clinical study of 1001 cases and review of the literature. Neurosurgery 74:595–604
Eskander MS, Balsis SM, Balinger C et al (2014) The association between preoperative spinal cord rotation and postoperative C5 nerve palsy. J Bone Joint Surg Am 94:1605–1609
Hasegawa K, Homma T, Chiba Y (2007) Upper extremity palsy following cervical decompression surgery results from a transient spinal cord lesion. Spine (Phila Pa 1976) 32:E197–E202
Wang T, Wang H, Liu S, Ding WY (2017) Incidence of C5 palsy after cervical surgery: a meta-analysis for last decade. Medicine (Baltimore) 96(45):e8560
Chiba K, Toyama Y, Matsumoto M, Maruiwa M, Watanabe M, Hirabayashi K (2002) Segmental motor paralysis after expansive open-door laminoplasty. Spine (Phila Pa 1976) 27(19):2108–2115
Sakaura H, Hosono N, Mukai Y, Ishii T, Yoshikawa H (2003) C5 palsy after decompression surgery for cervical myelopathy: review of the literature. Spine (Phila Pa 1976) 28(21):2447–2251
Kaneko K, Hashiguchi A, Kato Y, Kojima T, Imajyo Y, Taguchi T (2006) Investigation of motor dominant C5 paralysis after laminoplasty from the results of evoked spinal cord responses. J Spinal Disord Tech 19(5):358–361
Brown JM, Yee A, Ivens RA, Dribben W, Mackinnon SE (2010) Post-cervical decompression parsonage-turner syndrome represents a subset of C5 palsy: six cases and a review of the literature: case report. Neurosurgery 67(6):E1831–E1843
Radhakrishnan K, Litchy WJ, O'Fallon WM, Kurland LT (1994) Epidemiology of cervical radiculopathy. A population-based study from Rochester, Minnesota, 1976 through 1990. Brain 117(Pt 2):325–335
Stoker GE, Kim HJ, Riew KD (2014) Differentiating C8–T1 radiculopathy from ulnar neuropathy: a survey of 24 spine surgeons. Global Spine J 4(1):1–6
Tan LA, Riew KD, Traynelis VC (2017) Cervical spine deformity-part 3: posterior techniques, clinical outcome, and complications. Neurosurgery 81(6):893–898
Ebraheim NA, Lu J, Yang H, Heck BE, Yeasting RA (2000) Vulnerability of the sympathetic trunk during the anterior approach to the lower cervical spine. Spine (Phila Pa 1976) 25:1603–1606
Chacko AG, Joseph M, Turel MK, Prabhu K, Daniel RT, Jacob KS (2012) Multilevel oblique corpectomy for cervical spondylotic myelopathy preserves segmental motion. Eur. Spine J 21:1360–1367
Chibbaro S, Mirone G, Makiese O, George B (2009) Multilevel oblique corpectomy without fusion in managing cervical myelopathy: long-term outcome and stability evaluation in 268 patients. J Neurosurg Spine 10:458–465
Kanagalingam S, Miller NR (2015) Horner syndrome: clinical perspectives. Eye Brain 7:35–46
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Joaquim, A.F., Makhni, M.C. & Riew, K.D. Post-operative nerve injuries after cervical spine surgery. International Orthopaedics (SICOT) 43, 791–795 (2019). https://doi.org/10.1007/s00264-018-4257-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-4257-4