Abstract
Summary
We evaluated the influence of baseline age, bone mineral density (BMD), and serum levels of vitamin D on the response to risedronate treatment. Risedronate consistently increased BMD, but our results suggest vitamin D supplementation may be necessary to achieve optimal treatment effect. Furthermore, early intervention may help prevent bone fractures.
Introduction
We aimed to investigate the influence of baseline age, BMD, and vitamin D insufficiency on the response to risedronate treatment.
Methods
Data regarding 1447 patients was obtained from the registries of three phase III clinical trials of risedronate. The response to treatment was expressed in terms of BMD increase and occurrence of new vertebral fractures. The patients were stratified by baseline values for age (<65, 65–72, and ≥72 years), lumbar spine BMD T-score (osteoporotic, <−2.5; and non-osteoporotic, ≥− 2.5), and serum levels of 25-hydroxyvitamin D (deficient, <21 ng/mL; and non-deficient, ≥21 ng/mL).
Results
Risedronate consistently increased lumbar spine BMD in all the groups, with similar percentage and absolute increments in all the age tertiles. The percentage, but not absolute, increment in BMD was significantly higher (p = 0.0003) in the osteoporotic than that in the non-osteoporotic patients (baseline). Of the 1330 patients whose baseline serum levels of 25-hydroxyvitamin D were available, 44.7% had vitamin D deficiency (<20 ng/mL), while 89.2% had insufficiency (<30 ng/mL). The percentage and absolute increments in BMD were lower (p < 0.05 and p < 0.01, respectively) in the vitamin D-deficient than those in the non-deficient patients. New vertebral fractures occurred in 1.5 and 0.8% of the osteoporotic and non-osteoporotic patients, respectively (end of the treatment).
Conclusions
Therapeutic response in elderly patients is consistent, but early initiation of risedronate treatment may help prevent fractures. Risedronate-induced increase in BMD is lower in patients with vitamin D deficiency, suggesting that vitamin D supplementation is important to achieve optimal treatment response.
Similar content being viewed by others
Introduction
Bisphosphonates are widely used to treat osteoporosis, and the treatment is effective in most osteoporosis patients, although there are some patients known as “non-responders” [1, 2]. Previous reports have indicated that factors involved in insufficient response include secondary osteoporosis [2–6], advanced age [7, 8], vitamin D deficiency [2, 4–6, 9–12], and poor compliance [2–5].
While some studies [7, 8, 13] have examined the relationship between age and fracture reduction in the context of risedronate treatment, there is little information on whether risedronate-induced increase in bone mineral density (BMD) is consistent in elderly patients.
Furthermore, while it was shown that the percentage increase in BMD is related to the baseline BMD [14], absolute increments in BMD have not been described. Finally, although it was shown that vitamin D levels are correlated with the response to treatment for postmenopausal osteoporosis in terms of BMD changes and fracture rates [15], this relationship has not been fully described.
Risedronate is a third-generation bisphosphonate containing a pyridinyl group. Risedronate has already been shown to benefit postmenopausal women with established osteoporosis [13, 16–21]. Similar efficacy has been reported in Japanese clinical trials for oral administration of daily, weekly, or monthly single doses (2.5, 17.5, and 75 mg, respectively) [19, 20, 22, 23]. Risedronate was approved for use in clinical practice in Japan following a series of phase III trials during which vitamin D was not supplemented in order to ensure consistency with previous trials [24]. Therefore, by analyzing the data collected during these trials, it is possible to explore the influence of vitamin D insufficiency and deficiency on the response to risedronate treatment.
The aim of the present study was to investigate the relationship between baseline characteristics (age, BMD, and serum levels of vitamin D) and therapeutic effects (change in BMD and incidence of new vertebral fractures) of risedronate treatment for osteoporosis by analyzing data from three phase III clinical trials in Japanese populations.
Methods
Study design
The present study analyzed combined data from three randomized, double-blind, clinical phase III trials for risedronate, namely CCT-003 [19], CCT-101 [22], and CCT-301 [23]. These trials were carried out as multicenter studies in Japan between March 1999 and August 2011. The primary efficacy endpoint was the percent change in mean lumbar spine BMD (LS-BMD), and the results were similar between CCT-003 and CCT-101, and between CCT-003 and CCT-301 [19, 22, 23].
Trial CCT-003 consisted of 48 weeks of treatment, whereby eligible patients were randomly assigned to receive either a daily oral dose of risedronate (2.5 mg) or an intermittent cyclical dosage regimen of etidronate (each cycle consisted of a 2-week period of treatment with 200 mg/day and a 10-week medication-free period). Trial CCT-101 also consisted of 48 weeks of treatment, but eligible patients were randomly assigned to receive either a weekly (17.5 mg) or a daily (2.5 mg) oral dose of risedronate. Finally, trial CCT-301 consisted of 12 months of treatment, whereby eligible patients were randomly assigned to receive either a monthly (75 mg) or a daily (2.5 mg) oral dose of risedronate. In all the trials, blinding to the study drug was maintained by a double-dummy technique using active drugs and corresponding placebo tablets.
All the patients were treated in an ambulatory regime and supplemented with calcium lactate (1.54 g/day, corresponding to 200 mg of calcium per day) throughout the study period. However, vitamin D was not supplemented in order to ensure consistency with previous clinical trials [24]. Throughout the study period, concomitant use of any drugs known to affect bone metabolism was prohibited. The study protocols were approved by the Institutional Review Board of each institution prior to initiation of the study, and all the patients gave written informed consent before registration. The trials were conducted according to the Good Clinical Practice guidelines and in accordance with the Helsinki declaration. Details of the study design, patients involved, and protocols of these trials have been described elsewhere [19, 22, 23].
Selection of patients
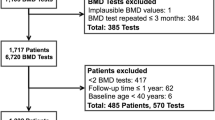
The present study consists of a post-hoc analysis of data from 1447 osteoporosis patients who received treatment with risedronate within one of the risedronate trials described above. Ambulatory patients of either sex, aged 40–75 years (trial CCT-003) or ≥50 years (trials CCT-101 and CCT-301), with involutional osteoporosis were eligible if they met the diagnostic criteria for primary osteoporosis established by the Japanese Society for Bone and Mineral Research (JSBMR) [25, 26]. Exclusion criteria included the following: secondary osteoporosis or other diseases known to cause reduced bone mass; radiographic findings that might affect the LS-BMD; recent use of drugs known to affect bone metabolism; gastrointestinal diseases; hypocalcemia; hypercalcemia; serious renal, hepatic, or cardiac diseases; malignant tumors under treatment with antitumor agents; drug hypersensitivity; and history of radiotherapy to the lumbar spine or pelvis (Fig. 1).
Clinical examinations
The effect of risedronate treatment was evaluated in terms of LS-BMD and the incidence of new, non-traumatic vertebral fractures (including worsening of pre-existing fractures) throughout the duration of treatment.
The LS-BMD (L2–L4) was determined at baseline and at designated time points via dual-energy X-ray absorptiometry, using QDR type instruments (trial CCT 301) or QDR type, XR type, or DPX type instruments (trials CCT-003 and CCT-101). These LS-BMD results were assessed by a specialized central review committee blinded to patient information.
Chest and lumbar spine X-rays were taken at baseline and at the end of the trial. A specialized central review committee decided whether there were pre-existing and new fractures, or if worsening of pre-existing fractures occurred. Vertebral fractures were judged based on the JSBMR diagnostic criteria for primary osteoporosis [25, 26]. An incident vertebral fracture was considered to have occurred if: the ratio of the central to anterior vertebral height (C/A) was <0.8; the ratio of central to posterior vertebral body height (C/P) was <0.8; the ratio of anterior to posterior vertebral height (A/P) was <0.75; or A, C, or P decreased by at least 20% from their baseline values. In trials CCT-003 and CCT-101, a pre-existing vertebral fracture was considered to have worsened if C/A, C/P, or A/P decreased by 20% or more from their baseline values [27]. In trial CCT-301, a semi quantitative assessment method was used to detect worsening of an existing fracture based on whether A, C, or P had decreased by at least 20% (or 4 mm) from their baseline values, in which case the condition was labeled to have progressed by one grade or more [28]. In addition, serum levels of 25-hydroxyvitamin D (further referred to as vitamin D) were measured at baseline by the radioimmunoassay method.
Statistical analyses
In order to examine the influence of baseline characteristics including age and BMD, the patients were stratified in groups according to age tertiles at baseline (<65, 65–72, and ≥72 years) and to LS-BMD T-score at baseline (osteoporotic, <−2.5; non-osteoporotic, ≥−2.5). To determine the most appropriate cutoff level of serum levels of vitamin D relevant for achieving optimal increase in BMD in response to risedronate treatment, the Akaike’s information criterion (AIC) was employed [29]. A smaller AIC value indicated a more reliable model for predicting the outcome, and the serum levels of vitamin D for the smallest AIC value were used as the cutoff.
One-way ANOVA was used for comparing the percentage and absolute increments in LS-BMD between patient groups defined according to age. Two-tailed Student’s t tests were conducted comparing the percentage and absolute changes in LS-BMD between the two groups defined based on baseline LS-BMD T-score. Chi-square tests were conducted for comparing the incidence of new vertebral fractures between the patient groups defined based on endpoint LS-BMD T-score. All analyses were performed using SAS version 9.2 (SAS Institute Inc., Cary, NC, USA).
Results
Out of the 1466 randomized patients (118 from the CCT-003 trial, 496 from the CCT-101 trial, and 852 from the CCT-301 trial), we assessed 1447 patients whose LS-BMD was measured at baseline (Fig. 1). The baseline characteristics of all the patients included in our analysis are shown in Table 1. X-ray examinations at baseline exhibited fragility fractures in 335 out of 1406 patients for whom X-ray examinations were available. Baseline serum levels of vitamin D were <20 ng/mL for 595 patients (44.7%), and <30 ng/mL for 1187 patients (89.2%), out of the 1330 patients for whom these data were available (Fig. 2).
Following treatment with risedronate, LS-BMD increased significantly compared to baseline (5.62 ± 4.33%, p < 0.0001). There were no statistically significant differences among the age groups in terms of percentage (p = 0.1720) or absolute (g/cm2) increments (p = 0.3524) in LS-BMD (<65 years, n = 487, 5.40 ± 4.44%, 0.0350 ± 0.0284 g/cm2; 65–72 years, n = 489, 5.91 ± 4.20%, 0.0374 ± 0.0264 g/cm2; ≥72 years, n = 393, 5.54 ± 4.33%, 0.0354 ± 0.0272 g/cm2) (Fig. 3a, b). Results were similar when the patients were stratified into age groups using different cutoffs (<75, 75–80, and ≥80 years) rather than into tertiles (data not shown).
Relationship between baseline characteristics and the increase in LS-BMD. Patients were divided into age tertiles based on the age at baseline. Percentage (a) and absolute (b) increments in LS-BMD from baseline are shown. The patients were stratified into two cohorts by LS-BMD (given by T-score) at baseline. Percentage (c) and absolute (d) increments in LS-BMD are shown. The patients were stratified into two cohorts by serum levels of 25-hydroxyvitamin D at baseline. Percentage (e) and absolute (f) BMD increments in LS-BMD from baseline are shown. Error bars represent standard deviation
The percentage increment in LS-BMD was a significantly higher (p = 0.0003) in the osteoporotic than that in the non-osteoporotic patients (respectively: n = 1171, 5.80 ± 4.37%; n = 198, 4.59 ± 3.93%), while no significant difference (p = 0.7524) was observed regarding the absolute BMD increments (0.0361 ± 0.0267 and 0.0354 ± 0.0308 g/cm2, respectively) (Fig. 3c, d).
The cutoff for serum levels of vitamin D was calculated as 21 ng/mL, according to the AIC. For the patients with baseline serum levels of vitamin D of ≥21 ng/mL, both percentage and absolute (g/cm2) increments of LS-BMD were significantly higher (p = 0.0138 and p = 0.0078, respectively) than those in the patients with baseline serum levels of vitamin D of <21 ng/mL (respectively: n = 626, 5.99 ± 4.17%, 0.0383 ± 0.0264 g/cm2; n = 635, 5.39 ± 4.42%, 0.0343 ± 0.0277 g/cm2) (Fig. 3e, f).
There was no statistically significant difference between the patients with endpoint LS-BMD T-score <−2.5 (n = 871, 13 cases, 1.5%) and those with endpoint LS-BMD T-score ≥−2.5 (n = 481, 4 cases, 0.8%) regarding the incidence of new vertebral fractures, but there was a trend for lower incidence in the group with higher BMD (Fig. 4). A similar trend was observed for the patients with baseline LS-BMD T-score <−2.5 (n = 1159), as those with endpoint LS-BMD T-score <−2.5 had a relatively lower incidence of new fracture (n = 869, 13 cases, 1.5%) than did the patients with endpoint LS-BMD T-score ≥−2.5 (n = 290, 2 cases, 0.7%) (Fig. 5); this difference did not reach statistical significance either.
Discussion
In our post-hoc analysis of data from a large-scale, strictly controlled, phase III clinical trial conducted in Japan, we found that risedronate consistently increased LS-BMD regardless of the baseline age, BMD, or vitamin D deficiency. The influence of such factors on the efficacy of osteoporotic treatment has been previously studied, with conflicting conclusions.
Specifically, the study by McClung et al. [16] included 5445 osteoporotic women aged 70–79 years and 3886 women aged ≥80 years. The study participants, each of whom had at least one clinical risk factor for hip fracture, received treatment with oral risedronate or placebo for 3 years. It was found that BMD response in the older patients was similar to that observed in the younger cohort, and the effect on hip fracture risk was apparent in the older patients whose baseline BMD was measured and was consistent with osteoporosis. Boonen et al. [7] also reported that risedronate consistently reduced the risk for vertebral fracture both in subjects younger than 80 years (hazard ratio, 0.61; p < 0.001) and in those aged 80 years or older (hazard ratio, 0.56; p = 0.003); nevertheless, the reduction in risk for nonvertebral fractures was statistically significant only in patients younger than 80 years, and no treatment effect was seen in patients aged 80 years or older. The authors speculated that the reduced treatment effect in terms of risk for nonvertebral fractures in the patients aged 80 years or older may reflect the age-related increase of the influence of nonskeletal risk factors (e.g., falling) for these types of fractures. Adami et al. [8] conducted a longitudinal study regarding the incidence of inadequate treatment response in osteoporosis patients, and concluded that those with inadequate clinical response to treatment with antiresorptive agents (alendronate, risedronate, and raloxifene) were significantly older (p = 0.032) and more frequently had multiple vertebral deformities (p = 0.013). Watts et al. [13] collected data on 3684 postmenopausal women involved in the Vertebral Efficacy with Risedronate Therapy trial. It was reported that the incidence of new fractures decreased to a similar extent in patients treated with risedronate and in those treated with placebos, and the effect was observed both in patients aged <70 years and in those aged ≥70 years. With respect to alendronate therapy, Ensrud et al. [30] performed post-hoc analyses of data from the Fracture Intervention trial, and reported that the alendronate-induced reduction in risk for fractures was similar for patients aged <75 years and for those aged ≥75 years. Hochberg et al. [31] analyzed data on 3658 postmenopausal women with osteoporosis enrolled in the same Fracture Intervention trial, and showed that alendronate is effective in reducing the risk of symptomatic osteoporotic fractures across a spectrum of ages (55–80 years). In our study on the effect of risedronate therapy, both percentage increments and absolute increments in LS-BMD were similar across the age tertiles, which is in agreement with the previous reports on the effect of alendronate therapy [30, 31].
Regarding the influence of baseline BMD, Gordon et al. [14] performed a linear regression analysis of the relationship between baseline BMD and BMD percentage increase in the lumbar spine and femoral neck, and found a statistically significant negative correlation; however, the sample size in their study was modest (n = 44), and absolute BMD increments were not described. Ensrud et al. [30] also examined the consistency of the effect of alendronate in preventing fractures within groups of patients defined according to baseline BMD of the femoral neck (FN-BMD); with respect to reducing the risk of new vertebral fractures, the treatment appeared to be as effective in women with FN-BMD <0.59 g/cm2 as in those with FN-BMD ≥0.59 g/cm2. The authors concluded that alendronate effectively reduces fracture risk in postmenopausal women with vertebral fracture and low BMD, and the effect is stronger in women at highest risk because of advanced age or severe osteoporosis. Our results have shown that BMD percentage increments are 1.21% higher in the subjects who were osteoporotic at baseline (T-score <−2.5) than those in the non-osteoporotic subjects, while absolute increments did not differ. On the other hand, as shown in Figs. 4 and 5, the incidence of new vertebral fractures seems dependent on the endpoint BMD, suggesting that risedronate therapy consistently increases the absolute value of LS-BMD, but early intervention may be important to ensure optimal reduction in fracture risk.
Vitamin D plays an essential role in the maintenance of bone strength and muscle function. Vitamin D repletion is pre-requisite inclusion criteria, and vitamin D is usually supplemented in most of the current clinical trials of osteoporosis treatments, though that is not always the case in routine clinical practice. Therefore, the role of vitamin D in bisphosphonate therapy is an important clinical question. Adami et al. [15] studied data on 1515 women with postmenopausal osteoporosis undergoing treatment with antiresorptive agents including alendronate, risedronate, and raloxifene for over 13 months; they reported that vitamin D-deficient and -repleted subjects differed significantly with respect to annual changes in spine and hip BMD; the adjusted odds ratio measuring the risk for incident fractures in vitamin D-deficient women relative to that in vitamin D-repleted women was 1.77 (95% confidence interval, 1.20–2.59; p = 0.004). In our present study, 595 out of the 1330 patients (44.7%) had serum levels of vitamin D <20 ng/mL, while 1187 out of the 1330 patients (89.2%) had serum levels of vitamin D <30 ng/mL (Fig. 2). According to the guidelines of the American Society of Endocrinology [32], vitamin D deficiency and insufficiency are defined when the serum levels of vitamin D are <20 and 21–29 ng/mL, respectively, suggesting that 90% of the patients in our cohort had vitamin D deficiency or insufficiency. These results are almost consistent with those of Ishijima et al., who reported that vitamin D levels were <30 ng/mL in 82% of Japanese postmenopausal osteoporosis patients (n = 52) undergoing a 6-month trial of alendronate therapy [33]. Okazaki et al. reported even higher percentage of vitamin D deficiency: <20 ng/mL in 75.7% of the Japanese population [34].
On the other hand, Peris et al. reported that 30% of Spanish postmenopausal osteoporotic women (n = 120) receiving alendronate or risedronate showed inadequate response to treatment, with significantly lower levels of vitamin D (22.4 ± 1.3 vs. 26.6 ± 0.3 ng/mL, p = 0.01) and higher incidence of vitamin D levels <30 ng/mL (91 vs. 69%, p = 0.019). Patients with values of vitamin D >30 ng/mL had a greater increase in LS-BMD than patients with values of vitamin D <30 ng/mL (3.6 vs. 0.8%, p < 0.05) [10].
Ishijima et al. administered alendronate to 52 Japanese postmenopausal women for 6 months; serum levels of vitamin D of ≥25 ng/mL were determined to be the minimum levels necessary to achieve an adequate effect of alendronate treatment. The increase in LS-BMD after a 6-month alendronate treatment was significantly lower in patients with serum vitamin D levels <25 ng/mL (3.3%; 95% confidence interval, 1.7–5.0%) than in those with serum vitamin D levels ≥25 ng/mL (6.8%; 95% confidence interval, 3.8–9.4%) [33].
In accordance with those reports, both of the percent and absolute increments in LS-BMD after risedronate treatment were significantly higher for patients with serum levels of vitamin D ≥21 ng/mL when compared to the those seen in patients with serum levels of vitamin D <21 ng/mL (respectively; 5.99 ± 4.17%, 0.0383 ± 0.0264 g/cm2; and 5.39 ± 4.42%, 0.0343 ± 0.0277 g/cm2; respectively, p = 0.0138 and p = 0.0079), suggesting the importance of vitamin D repletion in osteoporosis treatment.
The current study is limited by its post-hoc design. Another limitation of this study is that no placebo groups were available for comparison in the trials considered, and therefore, the effectiveness of risedronate on reducing fracture risk could not be compared between younger and older patients. Furthermore, other confounding factors remain to be investigated. We believe that a further prospective study is necessary to elucidate whether taking natural vitamin D supplements or alfacalcidol is able to increase the therapeutic effects of bisphosphonates against osteoporosis.
In conclusion, the results of this study suggest that risedronate administration consistently increases the absolute value of LS-BMD, regardless of age or baseline BMD. However, early start of the treatment seems to be important in order to prevent new fractures. Vitamin D deficiency and insufficiency are common conditions, and the BMD change in response to risedronate treatment seems to be smaller in the patients with serum levels of vitamin D <21 ng/mL when compared to the change seen in the patients with serum levels of vitamin D ≥21 ng/mL. This suggests that vitamin D supplementation may be important to achieve optimal LS-BMD response to risedronate treatment.
References
Lewiecki EM, Watts NB (2008) Assessing response to osteoporosis therapy. Osteoporos Int 19:1363–1368
Lewiecki EM (2003) Nonresponders to osteoporosis therapy. J Clin Densitom 6:307–314
del Puente A, Scognamiglio A, Itto E, Ferrara G, Oriente P (2000) Intramuscular clodronate in nonresponders to oral alendronate therapy for osteoporosis. J Rheumatol 27:1980–1983
Sawka AM, Adachi JD, Ioannidis G, Olszynski WP, Brown JP, Hanley DA, Murray T, Josse R, Sebaldt RJ, Petrie A, Tenenhouse A, Papaioannou A, Goldsmith CH (2003) What predicts early fracture or bone loss on bisphosphonate therapy? J Clin Densitom 6:315–322
Adami S, Isaia G, Luisetto G, Minisola S, Sinigaglia L, Gentilella R, Agnusdei D, Iori N, Nuti R, ICARO Study Group (2006) Fracture incidence and characterization in patients on osteoporosis treatment: the ICARO study. J Bone Miner Res 21:1565–1570
Prieto-Alhambra D, Pagès-Castellà A, Wallace G, Javaid MK, Judge A, Nogués X, Arden NK, Cooper C, Diez-Perez A (2014) Predictors of fracture while on treatment with oral bisphosphonates: a population-based cohort study. J Bone Miner Res 29:268–274
Boonen S, McClung MR, Eastell R, Fuleiban GEH, Barton IP, Delmas P (2004) Safety and efficacy of risedronate in reducing fracture risk in osteoporotic women aged 80 and older: implications for the use of antiresorptive agents in the old and oldest old. JAGS 52:1832–1839
Adami S, Isaia G, Luisetto G, Minisola S, Sinigaglia L, Silvestri S, Agnusdei D, Gentilella R, Nuti R (2008) Osteoporosis treatment and fracture incidence: the ICARO longitudinal study. Osteoporos Int 19:1219–1223
Heckman GA, Papaioannou A, Sebaldt RJ, Ioannidis G, Petrie A, Goldsmith C, Adachi JD (2002) Effect of vitamin D on bone mineral density of elderly patients with osteoporosis responding poorly to bisphosphonates. BMC Musculoskelet Disord 3:6
Peris P, Martínez-Ferrer A, Monegal A, Martínez de Osaba MJ, Muxi A, Guañabens N (2012) 25 hydroxyvitamin D serum levels influence adequate response to bisphosphonate treatment in postmenopausal osteoporosis. Bone 51:54–58
Díez-Pérez A, Olmos JM, Nogués X, Sosa M, Díaz-Curiel M, Pérez-Castrillón JL, Pérez-Cano R, Muñoz-Torres M, Torrijos A, Jodar E, Del Rio L, Caeiro-Rey JR, Farrerons J, Vila J, Arnaud C, González-Macías J (2012) Risk factors for prediction of inadequate response to antiresorptives. J Bone Miner Res 27:817–824
Carmel AS, Shieh A, Bang H, Bockman RS (2012) The 25(OH)D level needed to maintain a favorable bisphosphonate response is ≥33 ng/ml. Osteoporos Int 23:2479–2487
Watts NB, Josse RG, Hamdy RC, Hughes RA, Manhart MD, Barton I, Calligeros D, Felsenberg D (2003) Risedronate prevents new vertebral fractures in postmenopausal women at high risk. J Clin Endocrinol Metab 88:542–549
Gordon MS, Gordon MB (2002) Response of bone mineral density to once-weekly administration of risedronate. Endocr Pract 8:202–207
Adami S, Giannini S, Bianchi G, Sinigaglia L, Di Munno O, Fiore CE, Minisola S, Rossini M (2009) Vitamin D status and response to treatment in post-menopausal osteoporosis. Osteoporos Int 20:239–244
McClung MR, Geusens P, Miller PD, Zippel H, Bensen WG, Roux C, Adami S, Fogelman I, Diamond T, Eastell R, Meunier PJ, Reginster JY, Hip Intervention Program Study Group (2001) Effect of risedronate on the risk of hip fracture in elderly women. N Engl J Med 344:333–340
Harris ST, Watts NB, Genant HK, McKeever CD, Hangartner T, Keller M, Chesnut CH III, Brown J, Eriksen EF, Hoseyni MS, Axelrod DW, Miller PD, Vertebral Efficacy With Risedronate Therapy (VERT) Study Group (1999) Effects of risedronate treatment on vertebral and nonvertebral fractures in women with postmenopausal osteoporosis: a randomized controlled trial. JAMA 282:1344–1352
Reginster JY, Minne HW, Sorensen OH, Hooper M, Roux C, Brandi ML, Lund B, Ethgen D, Pack S, Roumagnac I, Eastell R, Vertebral Efficacy with Risedronate Therapy (VERT) Study Group (2000) Randomized trial of the effects of risedronate on vertebral fractures in women with established postmenopausal osteoporosis. Osteoporos Int 11:83–91
Fukunaga M, Kushida K, Kishimoto H, Shiraki M, Taketani Y, Minaguchi H, Inoue T, Morita R, Morii H, Yamamoto K, Ohashi Y, Orimo H, Risedronate Phase III Research Group (2002) A comparison of the effect of risedronate and etidronate on lumbar bone mineral density in Japanese patients with osteoporosis: a randomized controlled trial. Osteoporos Int 13:971–979
Kushida K, Fukunaga M, Kishimoto H, Shiraki M, Itabashi A, Inoue T, Kaneda K, Morii H, Nawata H, Yamamoto K, Ohashi Y, Orimo H, Risedronate Phase III Research Group (2004) A comparison of incidences of vertebral fracture in Japanese patients with involutional osteoporosis treated with risedronate and etidronate: a randomized, double-masked trial. J Bone Miner Metab 22:469–478
Sorensen OH, Crawford GM, Mulder H, Hosking DJ, Gennari C, Mellstrom D, Pack S, Wenderoth D, Cooper C, Reginster JY (2003) Long-term efficacy of risedronate: a 5-year placebo-controlled clinical experience. Bone 32:120–126
Kishimoto H, Fukunaga M, Kushida K, Shiraki M, Itabashi A, Nawata H, Nakamura T, Ohta H, Takaoka K, Ohashi Y, Risedronate Phase III Research Group (2006) Efficacy and tolerability of once-weekly administration of 17.5 mg risedronate in Japanese patients with involutional osteoporosis: a comparison with 2.5-mg once-daily dosage regimen. J Bone Miner Metab 24:405–413
Hagino H, Kishimoto H, Ohishi H, Horii S, Nakamura T (2014) Efficacy, tolerability and safety of once-monthly administration of 75mg risedronate in Japanese patients with involutional osteoporosis: a comparison with a 2.5mg once-daily dosage regimen. Bone 59:44–52
Fujita T, Orimo H, Inoue T, Kaneda K, Sakurai M, Morita R, Morii H, Yamamoto K, Sugioka Y, Inoue A, Hoshino Y, Kawaguchi H, Yamamoto I, Fukase M, Takaoka K (1993) Double-blind mulitcenter comparative study with alphacalcidol of etidronate disodium(EHDP) in involutional osteoporosis. Clin Eval 21:261–302
Orimo H, Sugioka Y, Fukunaga M, Muto Y, Hotokebuchi T, Gorai I, Nakamura T, Kushida K, Tanaka H, Ikai T, Oh-hashi Y (1998) Diagnostic criteria of primary osteoporosis. J Bone Miner Metab 16:139–150
Orimo H, Hayashi Y, Fukunaga M, Sone T, Fujiwara S, Shiraki M, Kushida K, Miyamoto S, Soen S, Nishimura J, Oh-hashi Y, Hosoi T, Gorai I, Tanaka H, Igai T, Kishimoto H, Osteoporosis Diagnostic Criteria Review Committee: Japanese Society for Bone and Mineral Research (2001) Diagnostic criteria for primary osteoporosis: year 2000 revision. J Bone Miner Metab 19:331–337
Division of Metabolism and Endocrine Drug Products of the United States Food and Drug Administration (1994) Guidelines for preclinical and clinical evaluation of agents used in the prevention or treatment of postmenopausal osteoporosis. US Food and Drug Administration
Genant HK, Wu CY, van Kuijk C, Nevitt MC (1993) Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 8:1137–1148
Akaike H (1974) A new look at the statistical model identification. IEEE Trans Autom Control 19:716–723
Ensrud KE, Black DM, Palermo L, Bauer DC, Barrett-Connor E, Quandt SA, Thompson DE, Karpf DB (1997) Treatment with alendronate prevents fractures in women at highest risk: results from the Fracture Intervention Trial. Arch Intern Med 157:2617–2624
Hochberg MC, Thompson DE, Black DM, Quandt SA, Cauley J, Geusens P, Ross PD, Baran D, FIT Research Group (2005) Effect of alendronate on the age-specific incidence of symptomatic osteoporotic fractures. J Bone Miner Res 20:971–976
Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, Murad MH, Weaver CM, Endocrine Society (2011) Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 96:1911–1930
Ishijima M, Sakamoto Y, Yamanaka M, Tokita A, Kitahara K, Kaneko H, Kurosawa H (2009) Minimum required vitamin D level for optimal increase in bone mineral density with alendronate treatment in osteoporotic women. Calcif Tissue Int 85:398–404
Okazaki R, Sugimoto T, Kaji H, Fujii Y, Shiraki M, Inoue D, Endo I, Okano T, Hirota T, Kurahashi I, Matsumoto T (2011) Vitamin D insufficiency defined by serum 25-hydroxyvitamin D and parathyroid hormone before and after oral vitamin D3 load in Japanese subjects. J Bone Miner Metab 29:103–110
Acknowledgements
This work was partially supported by a Grant-in-Aid from the Japan Society for the Promotion of Science KAKENHI (Grant No. 24592269 and Grant No. 15K10480), and by the Joint Development Program of EA Pharma Co., Ltd. and Takeda Pharmaceutical Co., Ltd.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Dr. Mawatari and Dr. Iwamoto have no conflict of interest to declare with respect to the work described herein.
Mr. Muraoka discloses an employment relationship with EA Pharma Co., Ltd., Tokyo, Japan.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Mawatari, T., Muraoka, R. & Iwamoto, Y. Relationship between baseline characteristics and response to risedronate treatment for osteoporosis: data from three Japanese phase III trials. Osteoporos Int 28, 1279–1286 (2017). https://doi.org/10.1007/s00198-016-3848-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-016-3848-4