Abstract
Human corneal transplantation to date suffers from the shortage of good-quality donor tissue, and in some conditions, allografting is contraindicated. A range of artificial replacements to donor allograft corneas have been developed. These range from keratoprostheses (KPro) that replace basic corneal functions of light transmission and protection to regenerative medicine strategies for regenerating one or more layers of the human cornea. This chapter reviews the advances made in developing artificial corneas or more accurately, artificial alternatives to donor allograft corneas for ocular application.
Similar content being viewed by others
Key words
1 Introduction
The cornea is the transparent front covering of the eye. It serves as a protective barrier against pathogenic attack and is also the main refractive part of the eye that is responsible for 65–75 % of light transmission to the retina, to enable vision [1]. It comprises three cellular layers: an outermost epithelium, middle stroma, and an innermost endothelium [2]. The cornea is highly innervated, and when healthy, it is avascular and immunologically privileged [1]. According to the World Health Organization, corneal blindness is the 4th largest cause of blindness worldwide [3]. In these cases, either loss of transparency or distortion of the refractive surface causes vision loss [1, 2]. Allograft cornea transplantation is the most common treatment.
The supply of high-quality donor cornea worldwide, however, falls well short of the demand. Allografting is contraindicated in a number of conditions such as autoimmune situations, chemical burns, and infections [4]. Allografting presents a very low but real risk of disease transmission, which is mostly circumvented by expensive screening procedures (e.g., processing fees in the USA are between $2,500 and $3,500 per cornea) [5]. These complications are compounded by the growing use of corrective eye surgery, which renders these corneas unsuitable for grafting, further reducing the availability of acceptable allogeneic supplies [6]. Initial success rates over 2 years are high, e.g., 85 % in a developed EU nation like Sweden [7]. The long-term success at 10–15 years, however, falls to 55 % [8], which is even lower than that for kidney transplantation [9]. In a developing country like India, even the short-term rates start out low, e.g., at 69 % in South India [10].
Replacement of allograft tissue has been a topic of interest, and there have been many versions of artificial replacements loosely grouped under “artificial corneas” that have been developed. These range from prostheses, known as keratoprostheses (KPro) to regenerative medicine approaches, to developing implants to promote regeneration of corneal tissues and nerves. Although decellularized corneas are becoming popular, we have not included them as they are not “artificially fabricated corneas.”
This short chapter reviews a few examples taken from the spectrum of artificial corneas ranging from those in clinical use to those under clinical and laboratory investigation, and from prostheses to those designed to promote corneal regeneration.
2 Keratoprostheses in Clinical Use
The concept of an artificial cornea was first proposed by Guillaume Pellier de Quengsy in 1789 [11]. In 1856, Nussbaum implanted the first glass artificial cornea into a patient [12]. Since these early approaches, there have been numerous versions of KPro and today, some are at the research stages and several are under clinical investigation or in clinical use.
Since their first appearance in the 1800s, the core-and-skirt designs for artificial cornea still remain popular. The optical core now commonly comprises a transparent plastic such as poly (methyl methacrylate), while the porous material of the skirt varied. In the Boston KPro, one of the most successful KPros to date, the donor cornea is placed between the front and back plates, and the combination is sutured into the corneal opening of the patient. This construct is successful in restoring visual acuity and can persist in the eye of a patient for years [13]. Retroprosthetic membrane formation and persistent epithelial defects were the most common postoperative complications in 22 and 19 eyes out of 50 examined in a clinical study, respectively [14].
Another well-known KPro that is used clinically is the AlphaCor™. In this KPro, both optic and skirt were fabricated from poly (2-hydroxyethyl methacrylate) (PHEMA). The optic is solid but the skirts comprise interconnecting pores that allow biointegration with surrounding corneal tissue. In a recent study [15], the AlphaCor™ cornea was transplanted in 15 patients. The retention rates of the device after 1, 2, and 3 years were 87 %, 58 %, and 42 %, respectively. Stromal melt was the most significant complication for AlphaCor transplantation (nine cases). One attributable cause was that the PHEMA-based AlphaCor™ presents low permeability to glucose due to its low water content. Water content is a necessary property of the normal human cornea (80 %) to allow diffusion of nutrients to support a healthy corneal epithelium and hence, overall corneal health.
3 Keratoprostheses with Regenerative Capacities
To increase the water content of the artificial cornea, Jacob and coworkers incorporated methacrylic acid monomers into PHEMA together with cell adhesion peptides and various cytokines which permitted the achievement of water content of over 70 % and increased the permeability of the hydrogel [16]. KPro epithelization has been argued to be important for the reduction of postoperative complications (particularly infections) by restoring the natural cellular barrier of eyes [17]. Jacob and coworkers [16] also treated the surface of the artificial construct with laminin and fibronectin, and reported enhancement of corneal epithelial growth in vitro [16], as epithelial cells adhered to these proteins.
To aid bio-integration and encourage the adherence of epithelial cells, more recent work with KPro has included: the mixing of different hydrogel polymers to create copolymers that harness the beneficial properties of each component, tethering of biomolecules to the copolymers [16], and introduction of surface coatings comprising extracellular matrix motifs/molecules onto polyvinyl alcohol hydrogels [18].
One recent KPro was fabricated from a mechanically enhanced hydrogel material called “duoptix” to develop a new “core-and-skirt” model. It consisted of a double (interpenetrating) network of poly (ethylene glycol) and poly (acrylic acid) (PAG/PAA) in its central optic component that is surface modified for the growth of epithelial cells. Surrounding the optic is a microperforated rim designed to promote peripheral tissue integration with the host eye [19]. The team has also used a versatile photochemical surface modification strategy to site-specifically tether cell adhesion-promoting biomolecules to these otherwise non-adhesive hydrogels. A further innovation is the application of photolithographic patterning to the fabrication of the device which provides high level of control over the shape and structure of a hydrogel, and potential over the growth and differentiation of cells. A more recent innovation is the development of a single-piece KPro with their interpenetrating networked hydrogel, complete with photolithographed surface, which at the time of the report, was undergoing evaluation in animal models [20].
Another newer KPro, developed by the research group of Dr. Joachim Storsberg at the Fraunhofer Institute, Germany, comprises a cell-free transparent optic of polymethylmethacrylate and the fibronectin-coated haptic (Fig. 1). Results to date showed good epicorneal fixation and biointegration of device in animals; [21] and this device is now undergoing clinical testing in human subjects.
The Fraunhofer epicorneal keratoprosthesis. This device comprises an anterior optic hydrophilic hydrogel (yellow ), and an outer haptic cum cell-attracting skirt (blue) (photo from Storsberg et al. [21], with copyright permission from the author)
4 Collagen-Based Scaffolds and Templates for Corneal Regeneration
Hydrogels of collagen type I, the predominant biopolymer in the human cornea, are particularly attractive as matrix replacement scaffolds, partly because of their strength at relatively low concentrations, resulting from the virtually rigid rod properties of the collagen type I triple helix [22]. In addition, collagen contains the cell attachment motif arginine–glycine–glutamic acid [23]. Collagen hydrogels are, however, unstable and hence require stabilization, e.g., by chemical cross-linking [24] or plastic compression (see Chapters 9 and 10).
The authors and collaborators have tested a range of collagen-based biomaterials as corneal substitutes. Hybrid biosynthetic hydrogels based on collagen and a poly (N-isopropylacrylamide)-derivative, acrylic acid, and N-acryloxysuccinimide grafted with tyrosine–isoleucin–glycine–serine–arginine (YIGSR) peptide were developed as mimic of the cornea stromal ECM-induced epithelial, stromal, and nerve regeneration when transplanted into the cornea of mini-pigs [25]. These implants had most likely emulated the ECM by allowing for cell–matrix interactions that resulted in the restoration of functional structures including the generation of a basement membrane between the implant and overlying epithelium, and stromal cell and nerve axon ingrowth. The incorporation of YIGSR into both bulk structure of the ethyl (dimethylaminopropyl) carbodiimide (EDC)/N-hydroxysuccinimide (NHS) cross-linked gels and onto the gel surface promoted the adhesion and proliferation of human corneal epithelial cells as well as neurite extension from dorsal root ganglia in vitro [26].
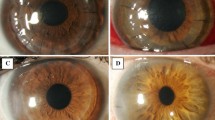
In 2009 and 2010, our group reported the 6-month and 2-year results, respectively, from implantation of EDC and NHS cross-linked recombinant human collagen corneal substitutes (see Chapter 10) in humans in a Phase I clinical study as lamellar grafts in ten patients [27, 28]. At 6 months postoperative, patients showed regeneration of epithelium, and ingrowth of stromal cells that was sufficient to anchor the implants [27]. After 2 years, the implants remained stably retained without the need for immunosuppression beyond the prophylactic use for the first 7 weeks after the surgery. Six of the ten patients had improved vision [28]. All ten showed corneal tissue, nerve and tear film regeneration, meaning that corneal epithelial cells grew over the implant, while stromal cell and nerves grew into the implant (Fig. 2), allowing for a tear film to form over the corneal surface. The tear film formation may have allowed the patients who were not able to tolerate contact lenses prior to the surgery to be able to now wear contact lenses to improve their eyesight.
(a) Cross-linked recombinant collagen-based implant. (b) The implant was trephined to prepare a button for corneal implantation. Damaged host tissue was removed to a similar depth and diameter and replaced by this button. (c) After implantation, the button was retained using overlying mattress sutures (from Fagerholm et al. [28], with the copyright permission from The American Association for the Advancement of Science)
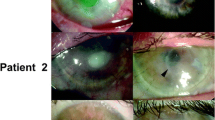
More recent work from our laboratory has shown that the clinical implants, while successfully tested in patients with keratoconus and central scarring, were not sufficiently robust for implantation into rabbit models of severe corneal damage, e.g., alkali burn [29]. A second-generation RHC implant containing an integrated network of 2-methacryloyloxyethyl phosphorylcholine (MPC), a synthetic phosphorylcholine lipid (first used as antifouling coatings in arterial stents), was developed [30]. These optimized RHC-MPC implants are significantly tougher and more resistant to enzymatic degradation or neovascularization. When implanted into alkali-burnt corneas in rabbit models, the RHC-MPC implants were able to repel blood vessels and prevent neovascularization of the implant (Fig. 3), unlike the control allografts or RHC-only implants. These implants were shown to allow regeneration of the different corneal nerve subtypes when implanted as full-thickness grafts in guinea pigs [31].
Typical postoperative appearance of vascularized corneal implants. Serial images of the same corneas are presented. One month postoperatively, neovessels invaded implants, while RHCIII-MPC implants appeared to block vessels (arrow ). By 6 months, vessels reduced in size and number, although central vessels remained in allograft and RHCIII implants while vessels in the RHCIII-MPC implant appeared to skirt the periphery before invading the implant (arrows). A further reduction in vascularization was noted at 9 months, but fine central vessels remained present (arrows) (photo from Hackett et al. [29], Copyright@ Association for Research in Vision and Ophthalmology)
5 Conclusions
There have been significant developments in tissue engineering approaches to replace the partial or full thickness of damaged or diseased corneas. Biomaterials have been developed to assist in these reparative procedures, to restore minimal function, or to regenerate the cornea to different degrees. For regeneration, biomaterials have been developed as interactive scaffolds to promote endogenous stem cell repair and regeneration. These different approaches may soon be able to supplement the supply of postmortem human corneas harvested for transplantation, or they may allow restoration of diseased or damaged corneas that cannot be treated by currently available techniques.
References
National Eye Institute. Facts about the cornea and corneal disease. www.nei.nih.gov/health/cornealdisease/#1
Asbell P, Brocks D (2010) Cornea overview. In Enclyclopedia of the Eye, DA Dartt, JC Besharse, R Dana. Academic Press, San Diego, USA, vol 1, pp. 552–531
WHO (2013) Prevention of blindness and visual impairment. Priority eye diseases. www.who.int/blindness/causes/priority/en/index9.html#
Hicks CR, Fitton JH, Chirila TV, Crawford GJ, Constable IJ (1997) Keratoprostheses: Advancing toward a true artificial cornea. Surv Ophthalmol 42:175–189
Hills K (2012) Challenges create cost increases for eye banks. www.revophth.com/content/d/cornea/c/32346
Mannis MJ, Sugar J (1995) Syphilis, serologic testing, and the setting of standards for eye banks. Am J Ophthalmol 119:93–95
Claesson M, Armitage WJ, Fagerholm P, Stevevi U (2002) Visual outcome in corneal grafts: a preliminary analysis of the Swedish Corneal Transplant Register. Br J Ophthalmol 86:174–180
Williams KA, Esterman AJ, Bartlett C, Holland H, Hornsby NB, Coster DJ (2006) How effective is penetrating corneal transplantation? Factors influencing long-term outcome in multivariate analysis. Transplantation 81:896–901
Wolfe RA (2004) Long-term renal allograft survival: a cup both half-full and half-empty. Am J Transplant 4:1215–1216
Dandona L, Naduvilth TJ, Janarthanan M, Ragu K, Rao GN (1997) Survival analysis and visual outcome in a large series of corneal transplants in India. Br J Ophthalmol 81:726–731
Barnham JJ, Roper-Hall MJ (1983) Keratoprosthesis: a long-term review. Br J Ophthalmol 67:468–474
Chirila TV, Hicks CR, Dalton PD, Vijayasekaran S, Lou X, Hong et al. (1998) Artificial Cornea Prog Polym Sci 23:447–473
Aldave AJ, Kamal KM, Vo RC, Yu F (2009) The Boston type I keratoprosthesis: improving outcomes and expanding indications. Ophthalmology 116:640–651
Aldave AJ, Kamal KM, Vo RC, Yu F (2009) Epithelial debridement and Bowman’s layer polishing for visually significant epithelial irregularity and recurrent corneal erosions. Cornea 28:1085–1090
Jiraskova N, Rozsival P, Burova M, Kalfertova M (2011) AlphaCor artificial cornea: clinical outcome. Eye 25:1138–1146
Jacob JT, Rochefort JR, Bi J, Gebhardt BM (2005) Corneal epithelial cell growth over tethered-protein/peptide surface-modified hydrogels. J Biomed Mater Res B Appl Biomater 72:198–205
Carlsson DJ, Li F, Shimmura S, Griffith M (2003) Bioengineered corneas: how close are we? Curr Opin Ophthalmol 14:192–197
Uchino Y, Shimmura S, Miyashita H, Taguchi T, Kobayashi H, Shimazaki J et al (2007) Amniotic membrane immobilized poly(vinyl alcohol) hybrid polymer as an artificial cornea scaffold that supports a stratified and differentiated corneal epithelium. J Biomed Mater Res B Appl Biomater 81:201–206
Myung D, Koh W, Bakri A, Zhang F, Marshall A, Ko J et al (2007) Design and fabrication of an artificial cornea based on a photolithographically patterned hydrogel construct. Biomed Microdevices 9:911–922
Myung D, Duchamel P-E, Cochran J, Noolandi J, Ta C, Frank C (2008) Development of hydrogel-based keratoprostheses: A materials perspective. Biotechnol Prog 24:735–741
Storsberg J, Kobuch K, Duncker G, Sel S (2011) Künstliche Augenhornhaut: biomaterialentwicklung eines ophthalmologischen Implantats mit biomimetischen Funktionalitaten. Dt Z Klin Forsch Ophthalmologie 5–6:58–61
Amis EJ, Carriere CJ, Ferry JD (1985) Effect of pH on collagen flexibility determined from dilute solution viscoelastic measurements. Int J Biol Macromol 7:130–134
Pierschbacher MD, Ruoslahti E (1987) Influence of stereochemistry of the sequence Arg-Gly-Asp-Xaa on binding specificity in cell adhesion. J Biol Chem 262:17294–17298
Hoffman AS (2002) Hydrogels for biomedical applications. Adv Drug Deliv Rev 54:3–12
Li F, Carlsson D, Lohmann C, Suuronen E, Vascotto S, Kobuch K et al (2003) Cellular and nerve regeneration within a biosynthetic extracellular matrix for corneal transplantation. Proc Natl Acad Sci U S A 100:15346–15351
Duan X, McLaughlin C, Griffith M, Sheardown H (2007) Biofunctionalization of collagen for improved biological response: scaffolds for corneal tissue engineering. Biomaterials 28:78–88
Fagerholm P, Lagali NS, Carlsson DJ, Merrett K, Griffith M (2009) Corneal regeneration following implantation of a biomimetic tissue-engineered substitute. Clin Transl Sci 2:162–164
Fagerholm P, Lagali NS, Merrett K, Jackson WB, Munger R, Liu Y et al (2010) A biosynthetic alternative to human donor tissue for inducing corneal regeneration: 24-month follow-up of a phase 1 clinical study. Sci Transl Med 2:46–61
Hackett JM, Lagali N, Merrett K, Edelhauser H, Sun Y, Gan L et al (2011) Biosynthetic corneal implants for replacement of pathologic corneal tissue: performance in a controlled rabbit alkali burn model. Invest Ophthalmol Vis Sci 52:651–657
Liu W, Deng C, McLaughlin CR, Fagerholm P, Lagali NS, Heyne B et al (2009) Collagen-phosphorylcholine interpenetrating network hydrogels as corneal substitutes. Biomaterials 30:1551–1559
McLaughlin CR, Acosta MC, Luna C, Liu W, Belmonte C, Griffith M et al (2010) Regeneration of functional nerves within full thickness collagen-phosphorylcholine corneal substitute implants in guinea pigs. Biomaterials 31:2770–2778
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media New York
About this protocol
Cite this protocol
Polisetti, N., Islam, M.M., Griffith, M. (2013). The Artificial Cornea. In: Wright, B., Connon, C. (eds) Corneal Regenerative Medicine. Methods in Molecular Biology, vol 1014. Humana Press, Totowa, NJ. https://doi.org/10.1007/978-1-62703-432-6_2
Download citation
DOI: https://doi.org/10.1007/978-1-62703-432-6_2
Published:
Publisher Name: Humana Press, Totowa, NJ
Print ISBN: 978-1-62703-431-9
Online ISBN: 978-1-62703-432-6
eBook Packages: Springer Protocols