Abstract
Background
Reexcision following breast-conserving surgery (BCS) in women with ductal carcinoma in situ (DCIS) results in adjuvant treatment delays, higher health care costs, and undesirable cosmetic outcomes. The purpose of this study is to determine patient, imaging, pathological, and surgical predictors of reexcision following BCS for DCIS.
Patients and Methods
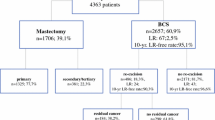
A retrospective review of women with DCIS who had BCS from 2007 to 2016 was conducted. Patient, imaging, pathological, and surgical features, in addition to surgical outcomes, were collected from medical records. Standard statistical tests were used to compare features between patients who did and did not undergo at least one reexcision. A multivariable logistic regression model was fit to assess features associated with reexcision.
Results
A total of 547 women (mean age 59 years; range 30–88 years) diagnosed with DCIS at core needle biopsy underwent BCS. Of all women, 31.6% (173/547) had at least one reexcision. With multivariable analysis, features associated with reexcision included younger patient age (adjusted odds ratio [aOR] 0.98, 95% confidence interval [CI] 0.97–1.0, p = 0.049), African-American race (aOR 2.66, 95% CI 1.13–6.26, p = 0.03), biopsy modality of ultrasound (aOR 2.35, 95% CI 1.22–4.53, p = 0.01), and earlier year of surgery (aOR 0.92, 95% CI 0.86–0.98, p = 0.01). No pathological features of DCIS were associated with reexcision risk.
Conclusions
In our cohort of nearly 550 women with DCIS who underwent BCS, 31.6% had at least one reexcision. Features associated with reexcision include younger patient age, African-American race, biopsy modality of ultrasound, and earlier year of surgery.
Similar content being viewed by others
References
American Cancer Society. How common is breast cancer? https://www.cancer.org/cancer/breast-cancer/about/how-common-is-breast-cancer.html. Accessed 1 June 2020.
Shehata M, Grimm L, Ballantyne N, et al. Ductal carcinoma in situ: current concepts in biology, imaging, and treatment. J Breast Imaging 2019;1(3):166–176. https://doi.org/10.1093/jbi/wbz039
Chen PH, Ghosh ET, Slanetz PJ, Eisenberg RL. Segmental breast calcifications. AJR Am J Roentgenol 2012;199(5):W532–542. https://doi.org/10.2214/ajr.11.8198
Gradishar WJ, Anderson BO, Balassanian R, et al. Breast Cancer, Version 4.2017, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw 2018;16(3):310–320. https://doi.org/10.6004/jnccn.2018.0012
Solin LJ, Fourquet A, Vicini FA, et al. Mammographically detected ductal carcinoma in situ of the breast treated with breast-conserving surgery and definitive breast irradiation: long-term outcome and prognostic significance of patient age and margin status. Int J Radiat Oncol Biol Phys 2001;50(4):991–1002. https://doi.org/10.1016/s0360-3016(01)01517-6
Pilewskie M, Morrow M. Margins in breast cancer: How much is enough? Cancer 2018;124(7):1335–1341. https://doi.org/10.1002/cncr.31221
Decker MR, Trentham-Dietz A, Loconte NK, et al. The role of intraoperative pathologic assessment in the surgical management of ductal carcinoma in situ. Ann Surg Oncol 2016;23(9):2788–2794. https://doi.org/10.1245/s10434-016-5192-5
Lange M, Reimer T, Hartmann S, Glass A, Stachs A. The role of specimen radiography in breast-conserving therapy of ductal carcinoma in situ. Breast 2016;26:73–79. https://doi.org/10.1016/j.breast.2015.12.014
Heelan Gladden AA, Sams S, Gleisner A, et al. Re-excision rates after breast conserving surgery following the 2014 SSO-ASTRO guidelines. Am J Surg 2017;214(6):1104–1109. https://doi.org/10.1016/j.amjsurg.2017.08.023
Langhans L, Jensen MB, Talman MM, Vejborg I, Kroman N, Tvedskov TF. Reoperation rates in ductal carcinoma in situ vs invasive breast cancer after wire-guided breast-conserving surgery. JAMA Surg 2017;152(4):378–384. https://doi.org/10.1001/jamasurg.2016.4751
Layfield DM, See H, Stahnke M, Hayward L, Cutress RI, Oeppen RS. Radiopathological features predictive of involved margins in ductal carcinoma in situ. Ann R Coll Surg Engl 2017;99(2):137–144. https://doi.org/10.1308/rcsann.2016.0299
Murphy BL, Boughey JC, Keeney MG, et al. Factors associated with positive margins in women undergoing breast conservation surgery. Mayo Clin Proc 2018;93(4):429–435. https://doi.org/10.1016/j.mayocp.2017.11.023
Philpott A, Wong J, Elder K, Gorelik A, Mann GB, Skandarajah A. Factors influencing reoperation following breast-conserving surgery. ANZ J Surg 2018;88(9):922–927. https://doi.org/10.1111/ans.14467
Houvenaeghel G, Lambaudie E, Bannier M, et al. Positive or close margins: reoperation rate and second conservative resection or total mastectomy? Cancer Manag Res 2019;11:2507–2516. https://doi.org/10.2147/cmar.s190852
Jeevan R, Cromwell DA, Trivella M, et al. Reoperation rates after breast conserving surgery for breast cancer among women in England: retrospective study of hospital episode statistics. BMJ 2012;345:e4505. https://doi.org/10.1136/bmj.e4505
Jung W, Kang E, Kim SM, et al. Factors associated with re-excision after breast-conserving surgery for early-stage breast cancer. J Breast Cancer 2012;15(4):412–419. https://doi.org/10.4048/jbc.2012.15.4.412
Wolf JH, Wen Y, Axelrod D, et al. Higher volume at time of breast conserving surgery reduces re-excision in DCIS. Int J Surg Oncol 2011;2011:785803. https://doi.org/10.1155/2011/785803
Joste M, Mendes V, Tixier S, et al. Non-menopausal status, high nuclear grade, tumor size > 30 mm and positive resection margins are predictors of residual tumor after lumpectomy for ductal carcinoma in situ of the breast. Anticancer Res 2015;35(6):3471–3477.
So A, De La Cruz LM, Williams AD, et al. The impact of preoperative magnetic resonance imaging and lumpectomy cavity shavings on re-excision rate in pure ductal carcinoma in situ-A single institution’s experience. J Surg Oncol 2018;117(4):558–566. https://doi.org/10.1002/jso.24890
Unzeitig A, Kobbermann A, Xie XJ, et al. Influence of surgical technique on mastectomy and reexcision rates in breast-conserving therapy for cancer. Int J Surg Oncol 2012;2012:725121. https://doi.org/10.1155/2012/725121
Ballal H, Taylor DB, Bourke AG, Latham B, Saunders CM. Predictors of re-excision in wire-guided wide local excision for early breast cancer: a Western Australian multi-centre experience. ANZ J Surg 2015;85(7–8):540–545. https://doi.org/10.1111/ans.13067
Rath MG, Uhlmann L, Heil J, et al. Predictors of residual tumor in breast-conserving therapy. Ann Surg Oncol 2015;22 Suppl 3:S451–458. https://doi.org/10.1245/s10434-015-4736-4
Morrow M, Van Zee KJ, Solin LJ, et al. Society of Surgical Oncology-American Society for Radiation Oncology-American Society of Clinical Oncology consensus guideline on margins for breast-conserving surgery with whole-breast irradiation in ductal carcinoma in situ. J Clin Oncol 2016;34(33):4040–4046. https://doi.org/10.1200/jco.2016.68.3573
American College of Radiology. Testing overview: breast MRI. https://accreditationsupport.acr.org/support/solutions/articles/11000068086-testing-overview-breast-mri-revised-12-12-19-. Accessed 1 June 2020.
Sickles EA, D’Orsi CJ, Bassett LW, et al. ACR BI-RADS Mammography. In: ACR BI-RADS Atlas, Breast Imaging Reporting and Data System. Reston, VA: American College of Radiology; 2013.
Clough KB, Gouveia PF, Benyahi D, et al. Positive margins after oncoplastic surgery for breast cancer. Ann Surg Oncol 2015;22(13):4247–4253. https://doi.org/10.1245/s10434-015-4514-3
DeSnyder SM, Hunt KK, Dong W, et al. American Society of Breast Surgeons’ practice patterns after publication of the SSO-ASTRO-ASCO DCIS consensus guideline on margins for breast-conserving surgery with whole-breast irradiation. Ann Surg Oncol 2018;25(10):2965–2974. https://doi.org/10.1245/s10434-018-6580-9
Sabel MS, Rogers K, Griffith K, et al. Residual disease after re-excision lumpectomy for close margins. J Surg Oncol 2009;99(2):99–103. https://doi.org/10.1002/jso.21215
Wang J, Kollias J, Boult M, et al. Patterns of surgical treatment for women with breast cancer in relation to age. Breast J 2010;16(1):60–65. https://doi.org/10.1111/j.1524-4741.2009.00828.x
Narod SA, Iqbal J, Giannakeas V, Sopik V, Sun P. Breast cancer mortality after a diagnosis of ductal carcinoma in situ. JAMA Oncol 2015;1(7):888–896. https://doi.org/10.1001/jamaoncol.2015.2510
Dillon MF, Mc Dermott EW, O’Doherty A, Quinn CM, Hill AD, O’Higgins N. Factors affecting successful breast conservation for ductal carcinoma in situ. Ann Surg Oncol 2007;14(5):1618–1628. https://doi.org/10.1245/s10434-006-9246-y
Acknowledgment
This work was supported by the Agfa HealthCare/Radiological Society of North America (RSNA) Research Scholar Grant (PI: Dr. Manisha Bahl) and the Electronic Space Systems Corporation (ESSCO)-MGH Breast Cancer Research Fund (PI: Dr. Manisha Bahl and Dr. Tawakalitu O. Oseni).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lamb, L.R., Mercaldo, S., Oseni, T.O. et al. Predictors of Reexcision following Breast-Conserving Surgery for Ductal Carcinoma In Situ. Ann Surg Oncol 28, 1390–1397 (2021). https://doi.org/10.1245/s10434-020-09101-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-020-09101-5