Abstract
Background
Food insecurity, or the limited or uncertain access to food resulting from inadequate financial resources, is associated with a higher prevalence of chronic disease in adulthood. Little is known about these relationships specifically in young adulthood, an important time for the development of chronic disease.
Objective
To determine the association between food insecurity and chronic disease including diabetes, hypertension, obesity, and obstructive airway disease in a nationally representative sample of US young adults.
Design
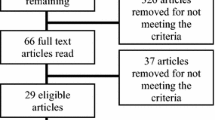
Cross-sectional nationally representative data collected from Wave IV (2008) of the National Longitudinal Study of Adolescent to Adult Health was analyzed using multiple logistic regression models.
Participants
US young adults ages 24–32 years old
Main Measures
Food insecurity and general health; self-reported diabetes, hypertension, hyperlipidemia, “very overweight,” and obstructive airway disease; measured obesity derived from body mass index; and inadequate disease control (hemoglobin A1c ≥ 7.0%, blood pressure ≥ 140/90 mmHg) among those with reported diabetes and hypertension.
Key Results
Of the 14,786 young adults in the sample, 11% were food insecure. Food-insecure young adults had greater odds of self-reported poor health (2.63, 95% confidence interval (CI) 1.63–4.24), diabetes (1.67, 95% CI 1.18–2.37), hypertension (1.40, 95% CI 1.14–1.72), being “very overweight” (1.30, 95% CI 1.08–1.57), and obstructive airway disease (1.48, 95% CI 1.22–1.80) in adjusted models compared with young adults who were food secure. Food insecurity was not associated with inadequate disease control among those with diabetes or hypertension.
Conclusions
Food insecurity is associated with several self-reported chronic diseases and obesity in young adulthood. Health care providers should screen for food insecurity in young adults and provide referrals when appropriate. Future research should evaluate the impact of early interventions to combat food insecurity on the prevention of downstream health effects in later adulthood.
Similar content being viewed by others
INTRODUCTION
Household food insecurity, defined as lacking “sufficient, safe, and nutritious food that meets individuals’ dietary needs and preferences for an active and healthy life,”1 affects nearly 50 million Americans.2 The limited research on food insecurity among young adults (ages 24–32) estimates that food insecurity affects 14% of young women and 9% of young men in the USA.3 Young adulthood represents an important developmental period that is distinct from adolescence and older adulthood.4 Young adults have a higher prevalence of chronic diseases and are less likely to eat breakfast, exercise, and get regular medical and dental checkups than adolescents.4 By age 32, fewer than 16% of young adults maintain optimal cardiovascular health, defined as normal blood pressure, glucose, and cholesterol without cardiovascular disease.5, 6 Young adulthood is also a time of educational and economic transitions, which may increase risk for food insecurity.7
Food insecurity is associated with a number of adverse child and adult health outcomes. Among children and youth, food insecurity is associated with 1.4–2.6 times higher odds of having asthma, a type of obstructive airway disease.8 Among adults, food insecurity is associated with diabetes, hypertension, and hyperlipidemia.9, 10 Young adulthood represents a period during which individuals begin to develop these cardiometabolic disease risk factors;11, 12 however, there is a paucity of research examining relationships between food insecurity and these chronic diseases in young adulthood. One of the few studies specifically in young adults found that food insecurity is associated with increased body mass index in young adult women.3 However, the association between food insecurity and other cardiometabolic outcomes (diabetes, hypertension, and hyperlipidemia) in young adulthood remains unknown. Furthermore, to our knowledge, there are no data on associations between food insecurity and obstructive airway disease, such as asthma, beyond the childhood period.8
The objective of this study is to determine the association between food insecurity and the prevalence of chronic diseases, specifically diabetes, hypertension, hyperlipidemia, obesity, and obstructive airway disease, after adjusting for potential confounders including socio-economic status and health behaviors, using a nationally representative sample of young adult men and women in the USA. We hypothesize that food insecurity will be associated with greater prevalence of each of these chronic disease outcomes. Determining the association between food insecurity and chronic disease outcomes net of other risk factors may have relevance for public health and clinical practice as reducing food insecurity may be a specific target for interventions to reduce chronic disease.
METHODS
Study Population
This study uses cross-sectional data from the National Longitudinal Study of Adolescent to Adult Health (Add Health).13 For this particular study, we used the nationally representative restricted-use cross-sectional sample from Wave IV of Add Health, collected in 2008 when participants were young adults (24–32 years). Wave IV was the only wave that collected information on food insecurity. The University of North Carolina Institutional Review Board approved all Add Health study procedures.
MEASURES
Primary Predictor Variable
Food insecurity: Food insecurity was based on self-report. Participants were asked, “In the past 12 months, was there a time when (you/your household were/was) worried whether food would run out before you would get money to buy more?” Response options were yes/no, with a 99.9% response rate. This single item has a 93% sensitivity and 85% specificity for detecting food insecurity as measured by the gold standard 18-item US Household Food Security Scale, and is considered the most inclusive question of the scale.3, 14, 15 Negative impacts on chronic disease outcomes have been shown along the gradient of food insecurity including at “marginal” levels, which would be consistent with answering affirmatively to this question even if not to the questions on restricted intakes.16 For the purposes of this study, we will refer to those with an affirmative response as “food insecure.”17, 18
Outcome Variables
Poor health status: Self-reported poor health status was based on a response of “poor” to the interview question, “In general, how is your health?” Response options included “excellent,” “very good,” “good,” “fair,” or “poor.”
Diabetes: Self-reported diabetes was based on an affirmative response to the interview question, “Has a doctor, nurse or other health care provider ever told you that you have or had: high blood sugar or diabetes (if female add, when you were not pregnant)?” Inadequate diabetes control was based on a measured hemoglobin A1c ≥ 7.0% among those with self-reported diabetes.9, 19
Hypertension: Self-reported hypertension was based on an affirmative response to the interview question, “Has a doctor, nurse or other health care provider ever told you that you have or had: high blood pressure or hypertension (if female add, when you were not pregnant)?” Inadequate hypertension control was based on measured systolic blood pressure ≥ 140 mmHg or a measured diastolic blood pressure ≥ 90 mmHg9, 20 using the average of two measurements 30 s apart from a factory-calibrated Microlife BP3MC1-PC-IB oscillometric blood pressure monitor (MicroLife USA, Inc.; Dunedin, FL) among those with self-reported hypertension.
Hyperlipidemia: Self-reported hyperlipidemia was based on an affirmative response to the interview question, “Has a doctor, nurse or other health care provider ever told you that you have or had: high blood cholesterol or triglycerides or lipids?”
“Very overweight”: Self-report was based on a response of “very overweight” to the interview question, “How do you think of yourself in terms of weight?” Response options included “very underweight,” “slightly underweight,” “about the right weight,” “slightly overweight,” and “very overweight.”
Obesity: Obesity was based on measured weight and height by the interviewer. Body mass index (BMI) was calculated using the standard formula weight (kilograms) divided by height (meters) squared (BMI = weight/height2). Young adults with BMI ≥ 30 were classified as obese in accordance with guidelines from the US Centers for Disease Control and Prevention (CDC).21
Obstructive airway disease: Self-reported obstructive airway disease was based on an affirmative response to the interview question, “Has a doctor, nurse or other health care provider ever told you that you have or had: asthma, chronic bronchitis or emphysema?”
Covariates
Age, sex, and race/ethnicity were recorded based on self-report.13 The highest level of education was based on self-report and categorized into less than high school (8th grade or less or some high school), high school graduate, some college (some college or vocational/technical training beyond high school), and college graduate (completed college, some graduate school, or a masters or doctoral degree).3 Household income was based on participant self-report. Participants were asked, “Thinking about your income and the income of everyone who lives in your household and contributes to the household budget, what was the total household income before taxes and deductions? Include all sources of income, including non-legal sources.” Gaussian normal regression imputation method was used to impute household income for the 835 participants who either refused to answer the income question or stated they did not know. Household income was transformed to a measure expressed as a ratio of household income relative to the poverty level in 2008 based on number of household members reported by the participant using a similar approach as previous studies.3, 17, 18 Presence of children in the household was based on participant report of any children currently living in the household. Physical activity was defined as the number of physical activity episodes for each of 49 possible activities from a pre-specified list reported in the past 7 days.3 Physical activity duration and intensity data were not collected. Smokers were identified as those currently smoking tobacco more than 10 days in the prior 30 days.3 Alcohol users were identified as those currently consuming alcohol on one or more days a week in the prior 30 days.3 All prescription medications taken in the last 4 weeks were recorded and classified into therapeutic classifications,22 including for diabetes23 and hypertension24 which have been described previously.
Statistical Analysis
Data analysis was performed in 2018 using STATA 15.0. Add Health’s pre-constructed sample weights were used for all analyses to yield nationally representative estimates. Further details about the Add Health sampling strategy and application of sampling weights are described in detail elsewhere.25, 26 Previous literature has shown that men and women have differential associations between food insecurity and BMI,3 though most studies examining food insecurity and other chronic disease outcomes did not stratify by sex.9, 10, 27 We therefore tested for an interaction between food insecurity and sex for each of the outcome variables. We did not find significant interactions between food insecurity and sex for any of the outcomes except for obesity. Consequently, our final models are not sex stratified other than for obesity. Multiple logistic regression analyses were used to identify associations with health outcomes (poor health status, diabetes, hypertension, hyperlipidemia, “very overweight,” obesity, and obstructive airway disease) as the dependent variables, and food insecurity as the independent variable, adjusting for race/ethnicity, age, education, household income relative to the poverty threshold, children in household, smoking, alcohol, and physical activity. Multiple logistic regression analyses were used to identify associations with inadequate disease control among participants with chronic disease (hemoglobin A1c ≥ 7.0% among participants with self-reported diagnosis of diabetes and blood pressure ≥ 140/90 mmHg for participants with self-reported diagnosis of hypertension) as the dependent variable, and food insecurity as the independent variable, adjusting for chronic disease–specific medications, race/ethnicity, age, education, household income relative to the poverty threshold, children in household, smoking, alcohol, and physical activity. P < 0.05 was considered statistically significant.
RESULTS
Of the 14,786 young adults (ages 24–32) included in Wave IV of Add Health, 11% were food insecure. The demographic and health characteristics of participants who were food secure versus food insecure are reported in Table 1 by sex. A greater proportion of young adults reporting food insecurity had poor health status, diabetes, hypertension, being “very overweight,” obesity, and obstructive airway disease compared with young adults who reported being food secure.
Logistic regression analyses with food insecurity as the independent variable and self-reported health outcomes as the dependent variables are presented in Table 2. Food-insecure young adults had greater odds of self-reported poor health status (2.63, 95% confidence interval (CI) 1.63–4.24), diabetes (1.67, 95% CI 1.18–2.37), hypertension (1.40, 95% CI 1.14–1.72), “very overweight” (1.30, 95% CI 1.08–1.57), and obstructive airway disease (1.48, 95% CI 1.22–1.80) but not hyperlipidemia (1.09, 95% CI 0.85–1.40) compared with young adults reporting food security.
Although food insecurity was significantly associated with measured obesity by BMI in unadjusted models (1.35, 95% CI 1.18–1.55), this association was no longer statistically significant in fully adjusted models (1.12, 95% CI 0.97–1.29). Given a significant interaction between food insecurity and sex (1.54, 95% CI 1.08–2.19), we further stratified obesity analyses by sex. Food insecurity was associated with 1.12 (0.93–1.43) odds of obesity in females and 1.00 (0.78–1.28) odds in males, but neither association was statistically significant.
Among participants with self-reported chronic diseases, food insecurity was not associated with inadequate disease control measures among participants with diabetes and hypertension, even when controlling for potential confounders (Table 3).
DISCUSSION
This study finds that food insecurity is associated with poor health and multiple chronic diseases in a nationally representative sample of US young adults. We report an 11% prevalence of food insecurity among young adults, similar to the national average of 12% in the general US adult population28 but lower than the 35–59% prevalence reported among young adult university students.29, 30 Young adulthood is an important yet understudied time period when cardiometabolic disease risk factors begin to develop.5, 6 We find that food insecurity is associated with self-reported poor health, diabetes, hypertension, being “very overweight,” and obstructive airway disease in young adults.
Prior evidence has shown that food insecurity is associated with cardiometabolic disease such as diabetes, hypertension, and hyperlipidemia in the general adult population.9, 10, 31 To our knowledge, this is the first study to investigate these associations with young adults using a nationally representative sample. Our findings in young adults confirm prior findings among the general adult population in terms of associations between food insecurity and diabetes and hypertension prevalence.9, 10 Studies in the general adult population examining the relationship between food insecurity and hyperlipidemia have shown mixed findings;9, 32,31,34 we did not find a significant association between food insecurity and hyperlipidemia. Food insecurity has also been linked to poorer general self-rated health in the general adult population,27 and we confirm this finding in young adults.
Three mechanisms may explain the association between food insecurity and cardiometabolic disease. First, food insecurity has been linked to the consumption of cheaper, calorie-dense but nutrient poor foods that include increased fats and carbohydrates10, 35, 36 and less consumption of fruits and vegetables. Second, the cyclic nature of food insecurity, reflective of monthly paychecks and food assistance, may promote insulin resistance due to alternating periods of food access and food shortage.37, 38 Furthermore, alternating episodes of food availability and scarcity promotes binge eating behaviors and subsequent obesity.39 Third, chronic stress and anxiety from food insecurity may contribute to insulin resistance, adiposity, and high blood pressure.10, 40 Stress triggered by food insecurity can activate the hypothalamic-pituitary-adrenal axis and stimulate the release of glucocorticoids, which can alter metabolism, lead to increased visceral fat accumulation and storage, and amplify binge eating behaviors.41, 42 Increased cortisol levels due to stress, in turn, increase blood glucose and insulin resistance, which play critical roles in the development of type 2 diabetes.42, 43
Chronic diseases may also contribute to food insecurity. Chronic diseases such as diabetes and hypertension may require medications and more frequent health care visits which can result in greater health care costs.44 As individuals develop more severe chronic conditions, they may be less able to work and generate income.45 Furthermore, dietary counseling and health education at health care visits may increase awareness of diet recommendations but also inability to afford healthy foods, which lead to an increased perception of food insecurity.9
Among participants with self-reported diabetes and hypertension, food insecurity was not associated with measures of inadequate disease control. Although prior studies among low-income adults found that food insecurity was associated with poor diabetes control as measured by hemoglobin A1c,46, 47 we did not find a significant association. However, the same study did not find an association between food insecurity and hypertension disease control, similar to our findings.9
To our knowledge, our study is the first to demonstrate an association between food insecurity and obstructive airway disease in adults, specifically young adults. One study found that multiple hunger episodes were associated with asthma in children and youth.8 Stress may lead to greater inflammation,48 which is involved in the pathophysiology of asthma, and more frequent asthma exacerbations.49 Food insecurity and malnutrition may lead to increased susceptibility to infections;50 recurrent respiratory infections may increase risk for asthma and bronchitis. Asthma is related to food allergies and persons living with food insecurity may have less control over avoiding allergens including foods that exacerbate allergies.51 Obstructive airway disease may decrease ability to work and health care costs associated with obstructive airway disease may exacerbate food insecurity.45 It is also possible there are confounders related to poverty such as air pollution and household allergens we were not able to fully measure in analyzing the relationship between food insecurity and obstructive airway disease.
Our study has several limitations. First, the cross-sectional nature of the study precludes causal inferences. The predictor and most outcome measures were based on self-report, which may be subject to response bias. Food insecurity was assessed by a single-item food security measure, the first item of both the full 18-item US Household Food Security Scale and the validated 6-item short form.15 Future research in young adults could assess food insecurity using the full US Household Food Security Scale. The clinical measures as ascertained in Add Health were not sufficient for a medical diagnosis; thus, we only assessed disease control. For instance, hypertension is based on measurements from the day of the interview in Add Health whereas repeated measures on three occasions would be required for a formal medical diagnosis.20 Furthermore, we were unable to assess disease control in hyperlipidemia given limitations in the total cholesterol measure available in Add Health (reliability of 0.40, corresponding to a 17 mg/dl minimal detectable difference in total cholesterol between two independent samples).52 The obstructive airway disease question combined asthma, chronic bronchitis, and emphysema into one category, so we are unable to determine the association of food insecurity with these specific diseases. We were not able to assess disease control for obstructive airway disease as there was no measurement such as peak flow or forced expiratory volume. Although we controlled for a number of potential confounders including age, race/ethnicity, education, household income adjusted relative to the poverty threshold, children in household, smoking, alcohol, physical activity, and medication use, there is the possibility for unmeasured confounders. Nonetheless, the limitations were offset by strengths, including a large, nationally representative sample size of an understudied population of young adults.
Food insecurity is now recognized as an important social determinant of health 53. Health care providers should ask patients about food insecurity, and short two-question screening tools are available.14 Patients with food insecurity should be referred to appropriate social services and provided additional information on choosing healthy foods from these programs. Given the association between food insecurity and several chronic diseases net of other factors, it is plausible that interventions to reduce food insecurity may contribute to the reduction of chronic diseases and this is an area for future study in longitudinal or interventions research. The Supplemental Nutrition Assistance Program (SNAP, formerly the Food Stamp Program) has a well-established infrastructure to reduce rates of food insecurity in the USA.10, 54, 55 Future interventions to promote food security, healthy nutrition using programs like the SNAP,54 and cardiometabolic health in young adults could be integrated. Future research could also assess food insecurity longitudinally from adolescence through the transition to adulthood to better determine causal inferences between food insecurity and health outcomes during this important time period in the life course.
CONCLUSION
Food insecurity is associated with several self-reported chronic diseases including diabetes, hypertension, and obstructive airway disease in a nationally representative sample of US young adults. Young adulthood may be an important time to screen for and address food security given the development of many of these chronic health conditions during this time period. Future research should examine the association between food insecurity and chronic disease longitudinally and integrate interventions to combat both food insecurity and chronic disease development in young adulthood.
References
United Nations Food and Agriculture Organization. Trade reforms and food security. Rome, Italy: Food and Agriculture Organization; 2003.
Coleman-Jensen A, Rabbitt MP, Gregory C, Singh A. Household food security in the united states in 2015. Vol ERR-215. United States Department of Agriculture, Economic Research Service; 2016.
Gooding HC, Walls CE, Richmond TK. Food insecurity and increased BMI in young adult women. Obesity (Silver Spring). 2012;20(9):1896–1901.
Stroud C, Walker LR, Davis M, Irwin CE,Jr. Investing in the health and well-being of young adults. J Adolesc Health. 2015;56(2):127–129.
Benjamin EJ, Blaha MJ, Chiuve SE, et al. Heart disease and stroke statistics-2017 update: A report from the american heart association. Circulation. 2017;135(10):e603.
Gooding HC, Milliren C, Shay CM, Richmond TK, Field AE, Gillman MW. Achieving cardiovascular health in young adulthood-which adolescent factors matter? J Adolesc Health. 2016;58(1):119–121.
Vespa J. The changing economics and demographics of young adulthood: 1975-2016. US Census Bureau. 2017:20. https://www.census.gov/library/publications/2017/demo/p20-579.html. Accessed Dec 7, 2018.
Kirkpatrick SI, McIntyre L, Potestio ML. Child hunger and long-term adverse consequences for health. Arch Pediatr Adolesc Med. 2010;164(8):754–762. Accessed Nov 14, 2018. doi: https://doi.org/10.1001/archpediatrics.2010.117.
Seligman HK, Laraia BA, Kushel MB. Food insecurity is associated with chronic disease among low-income NHANES participants. J Nutr. 2010;140(2):304–310. Accessed Nov 14, 2018. doi: https://doi.org/10.3945/jn.109.112573.
Seligman HK, Bindman AB, Vittinghoff E, Kanaya AM, Kushel MB. Food insecurity is associated with diabetes mellitus: Results from the national health examination and nutrition examination survey (NHANES) 1999-2002. J Gen Intern Med. 2007;22(7):1018–1023. Accessed Nov 13, 2018. doi: https://doi.org/10.1007/s11606-007-0192-6.
Skinner AC, Perrin EM, Moss LA, Skelton JA. Cardiometabolic risks and severity of obesity in children and young adults. N Engl J Med. 2015;373(14):1307–1317.
May AL, Kuklina EV, Yoon PW. Prevalence of cardiovascular disease risk factors among US adolescents, 1999-2008. Pediatrics. 2012;129(6):1035–1041. doi: https://doi.org/10.1542/peds.2011-1082.
Harris KM, Halpern CT, Whitsel E, et al. The national longitudinal study of adolescent to adult health: Research design. https://www.cpc.unc.edu/projects/addhealth/design/researchdesign_3618_regular.pdf. Updated 2017.
Hager ER, Quigg AM, Black MM, et al. Development and validity of a 2-item screen to identify families at risk for food insecurity. Pediatrics. 2010;126(1):26.
Bickel G, Nord M, Price C, Hamilton W, Cook J. Guide to measuring household food security. Alexandria, VA: USDA, Food and Nutrition Service; 2000.
Gregory CA, Coleman-Jensen A. Food insecurity, chronic disease, and health among working-age adults. Economic Research Report. 2017. https://nopren.org/wp-content/uploads/2017/08/ERS-Report-Food-Insecurity-Chronic-Disease-and-Health-Among-Working-Age-Adults.pdf. Accessed Dec 7, 2018.
Nagata JM, Weiser SD, Gooding HC, Garber AK, Bibbins-Domingo K, Palar K. Association Between Food Insecurity and Migraine Among US Young Adults. JAMA Neurol. 2019 Jun 24. https://doi.org/10.1001/jamaneurol.2019.1663.
Nagata JM, Palar K, Gooding HC, Garber AK, Whittle HJ, Bibbins-Domingo K, Weiser SD. Food Insecurity is Associated with Poorer Mental Health and Sleep Outcomes in Young Adults. J Adolesc Health. In Press.
American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2014;37 Suppl 1:81.
Chobanian AV, Bakris GL, Black HR, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: The JNC 7 report. JAMA. 2003;289(19):2560–2572.
Centers for Disease Control. Defining adult overweight and obesity. . 2012.
Tabor J, Whitsel EA. Add health wave IV documentation: Prescription medication use. University of North Carolina, Chapel Hill. 2010.
Whitsel EA, Tabor JW, Nguyen QC, et al. Add health wave IV documentation: Measures of glucose homeostasis. ; 2012. https://www.cpc.unc.edu/projects/addhealth/documentation/guides/Glucose_HbA1c.pdf. Accessed December 17, 2018.
Gooding HC, McGinty S, Richmond TK, Gillman MW, Field AE. Hypertension awareness and control among young adults in the national longitudinal study of adolescent health. J Gen Intern Med. 2014;29(8):1098–1104. Accessed Dec 17, 2018. doi: https://doi.org/10.1007/s11606-014-2809-x.
Harris KM. The add health study: Design and accomplishments. Carolina Population Center, University of North Carolina at Chapel Hill; 2013. http://www.cpc.unc.edu/projects/addhealth/documentation/guides/DesignPaperWIIV.pdf. Accessed 25 August 2019.
Chen P.Appropriate analysis in add health: Correcting for design effects & selecting weights. Carolina Population Center, University of North Carolina at Chapel Hill; 2014. http://www.cpc.unc.edu/projects/addhealth/events/2014-add-health-users-conference-appropriate-analysis-ping-chen. Accessed 25 August 2019.
Stuff JE, Casey PH, Szeto KL, et al. Household food insecurity is associated with adult health status. J Nutr. 2004;134(9):2330–2335. Accessed Nov 14, 2018. doi: https://doi.org/10.1093/jn/134.9.2330.
Coleman-Jensen A, Rabbitt MP, Gregory CA, Singh A. Household food security in the united states in 2017, ERR-256. . 2018.
Morris LM, Smith S, Davis J, Null DB. The prevalence of food security and insecurity among illinois university students. J Nutr Educ Behav. 2016;48(6):382.e1. Accessed Dec 7, 2018. doi: https://doi.org/10.1016/j.jneb.2016.03.013.
Patton-López MM, López-Cevallos DF, Cancel-Tirado DI, Vazquez L. Prevalence and correlates of food insecurity among students attending a midsize rural university in oregon. J Nutr Educ Behav. 2014;46(3):209–214. Accessed Dec 7, 2018. doi: https://doi.org/10.1016/j.jneb.2013.10.007.
Vosoris N, Tarasuk V. Household food insufficiency is associated with poorer health. J Nutr. 2003;133(1):120.
Shin J, Bautista LE, Walsh MC, Malecki KC, Nieto FJ. Food insecurity and dyslipidemia in a representative population-based sample in the US. Prev Med. 2015;77:186–190. Accessed Dec 14, 2018. doi: https://doi.org/10.1016/j.ypmed.2015.05.009.
Weigel MM, Armijos RX. Food insecurity, cardiometabolic health, and health care in U.S.-mexico border immigrant adults: An exploratory study. J Immigr Minor Health. 2018. Accessed Dec 14, 2018. doi: https://doi.org/10.1007/s10903-018-0817-3.
Tayie FA, Zizza CA. Concerns about the secondary data analysis of the association between food insecurity and hyperlipidemia in low-income NHANES participants. J Nutr. 2010;140(8):1535; author reply 1536. Accessed Dec 14, 2018. doi: https://doi.org/10.3945/jn.110.123281.
Lee JS, Frongillo EA. Nutritional and health consequences are associated with food insecurity among U.S. elderly persons. J Nutr. 2001;131(5):1503–1509. Accessed Nov 14, 2018. doi: https://doi.org/10.1093/jn/131.5.1503.
Kendall A, Olson CM, Frongillo EA. Relationship of hunger and food insecurity to food availability and consumption. J Am Diet Assoc. 1996;96(10):1026. Accessed Nov 14, 2018. doi: https://doi.org/10.1016/S0002-8223(96)00271-4.
Urbszat D, Herman CP, Polivy J. Eat, drink, and be merry, for tomorrow we diet: Effects of anticipated deprivation on food intake in restrained and unrestrained eaters. J Abnorm Psychol. 2002;111(2):396–401. Accessed Nov 14, 2018.
Duska F, Andel M, Kubena A, Macdonald IA. Effects of acute starvation on insulin resistance in obese patients with and without type 2 diabetes mellitus. Clin Nutr. 2005;24(6):1056–1064. Accessed Nov 14, 2018. doi: https://doi.org/10.1016/j.clnu.2005.08.008.
Becker CB, Middlemass K, Taylor B, Johnson C, Gomez F. Food insecurity and eating disorder pathology. Int J Eat Disord. 2017;50(9):1031–1040. Accessed Nov 27, 2018. doi: https://doi.org/10.1002/eat.22735.
Pryor L, Lioret S, van der Waerden J, Fombonne É, Falissard B, Melchior M. Food insecurity and mental health problems among a community sample of young adults. Soc Psychiatry Psychiatr Epidemiol. 2016;51(8):1073–1081. Accessed Nov 14, 2018. doi: https://doi.org/10.1007/s00127-016-1249-9.
Razzoli M, Pearson C, Crow S, Bartolomucci A. Stress, overeating, and obesity: Insights from human studies and preclinical models. Neurosci Biobehav Rev. 2017;76(Pt A):154–162. Accessed Nov 27, 2018. doi: https://doi.org/10.1016/j.neubiorev.2017.01.026.
de Kloet AD, Herman JP. Fat-brain connections: Adipocyte glucocorticoid control of stress and metabolism. Front Neuroendocrinol. 2018;48:50–57. Accessed Nov 27, 2018. doi: https://doi.org/10.1016/j.yfrne.2017.10.005.
Joseph JJ, Golden SH. Cortisol dysregulation: The bidirectional link between stress, depression, and type 2 diabetes mellitus. Ann N Y Acad Sci. 2017;1391(1):20–34. Accessed Nov 27, 2018. doi: https://doi.org/10.1111/nyas.13217.
Bernard DM, Banthin JS, Encinosa WE. Health care expenditure burdens among adults with diabetes in 2001. Med Care. 2006;44(3):210–215. Accessed Nov 14, 2018. doi: https://doi.org/10.1097/01.mlr.0000199729.25503.60.
Jetha A, Chen C, Mustard C, et al. Longitudinal examination of temporality in the association between chronic disease diagnosis and changes in work status and hours worked. Occup Environ Med. 2017;74(3):184–191. Accessed Nov 26, 2018. doi: https://doi.org/10.1136/oemed-2016-103569.
Heerman WJ, Wallston KA, Osborn CY, Bian A, Schlundt DG, Barto SD, Rothman RL. Food insecurity is associated with diabetes self-care behaviours and glycaemic control. Diabetic Medicine. 2016; 33(6):844-850.
Mayer VL, McDonough K, Seligman H, Mitra N, Long JA. Food insecurity, coping strategies and glucose control in low-income patients with diabetes. Public Health Nutrition. 2016;19(6):1103-1111.
Powell ND, Sloan EK, Bailey MT, et al. Social stress up-regulates inflammatory gene expression in the leukocyte transcriptome via β-adrenergic induction of myelopoiesis. PNAS. 2013;110(41):16574–16579. Accessed Nov 26, 2018.
Theoharides TC, Enakuaa S, Sismanopoulos N, et al. Contribution of stress to asthma worsening through mast cell activation. Ann Allergy Asthma Immunol. 2012;109(1):14–19. Accessed Nov 14, 2018. doi: https://doi.org/10.1016/j.anai.2012.03.003.
Lartey A. Maternal and child nutrition in sub-saharan africa: Challenges and interventions. Proc Nutr Soc. 2008;67(1):105.
Zhou H, Dai C, Pan J. Pediatric asthma and food allergy. Indian J Pediatr. 2017;84(8):585–590. Accessed Nov 27, 2018. doi: https://doi.org/10.1007/s12098-017-2326-0.
Whitsel EA, Cuthbertson CC, Tabor JW, et al. Add health wave IV documentation: Lipids. ; 2013. https://www.cpc.unc.edu/projects/addhealth/documentation/guides/Wave_IV_Lipids_documentation.pdf. Accessed November 27, 2018.
Nagata JM, Magerenge RO, Young SL, Oguta JO, Weiser SD, Cohen CR. Social determinants, lived experiences, and consequences of household food insecurity among persons living with HIV/AIDS on the shore of Lake Victoria, Kenya. AIDS Care. 2012;24 (6):728-736.
Collins AM, Klerman JA. Improving nutrition by increasing supplemental nutrition assistance program benefits. Am J Prev Med. 2017;52(2S2):S185. Accessed Nov 14, 2018. doi: https://doi.org/10.1016/j.amepre.2016.08.032.
Berkowitz SA, Seligman HK, Rigdon J, Meigs JB, Basu S. Supplemental nutrition assistance program (SNAP) participation and health care expenditures among low-income adults. JAMA Intern Med. 2017;177(11):1642–1649. Accessed Nov 14, 2018. doi: https://doi.org/10.1001/jamainternmed.2017.4841.
Acknowledgments
Contributers: This research uses data from Add Health, a program project directed by Kathleen Mullan Harris and designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris at the University of North Carolina at Chapel Hill, and funded by grant P01-HD31921 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, with cooperative funding from 23 other federal agencies and foundations. Special acknowledgment is due Ronald R. Rindfuss and Barbara Entwisle for assistance in the original design. Information on how to obtain the Add Health data files is available on the Add Health website (http://www.cpc.unc.edu/addhealth). No direct support was received from grant P01-HD31921 for this analysis.
Funding
Jason Nagata is a Fellow in the Pediatric Scientist Development Program (K12HD000850-33). This project was supported by grants from the University of California Global Food Initiative Fellowship, the American Heart Association (CDA34760281), the American Academy of Pediatrics (AAP), the American Pediatric Society (APS), and the Norman Schlossberger Research Fund and the Mt. Zion Health Fund from the University of California, San Francisco. Kartika Palar is supported by NIH K01 DK 107335. Andrea Garber is supported by NIH 5R01HD082166-02. Holly Gooding is supported by NIH K23 HL122361. Sheri Weiser is supported by NIH K24AI134326.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The University of North Carolina Institutional Review Board approved all Add Health study procedures.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nagata, J.M., Palar, K., Gooding, H.C. et al. Food Insecurity and Chronic Disease in US Young Adults: Findings from the National Longitudinal Study of Adolescent to Adult Health. J GEN INTERN MED 34, 2756–2762 (2019). https://doi.org/10.1007/s11606-019-05317-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-019-05317-8