Abstract
Background
It remains controversial if metastatic cervical lymph nodes in patients with intrathoracic esophageal cancer signify distant metastases and are therefore incurable or if they should be regarded as regional spread with a potential for cure.
Material and Methods
Patients with intrathoracic esophageal squamous cell carcinoma managed from 1995 to 2007, in whom metastatic cervical lymph node spread was confirmed by fine needle aspiration cytology, were studied. Treatment strategies and outcome were reviewed.
Results
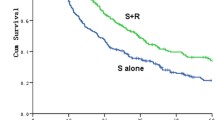
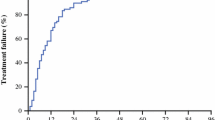
There were 109 patients, of whom 98 were men. Median age was 62 years (range, 34–88). Excluding those who underwent primarily palliative treatments, there were two main groups: 22 who had upfront chemoradiation therapy and subsequent esophagectomy ± cervical lymphadenectomy and 46 who had chemoradiation only. Significant downstaging occurred in 29 of the 68 patients (42.6%), of whom eight (11.8%) had complete pathological/clinical response. There was no mortality after esophagectomy. Median survival of patients with chemoradiation plus esophagectomy was 34.8 months compared to those with no surgery at 9.9 months, (p < 0.001). Patients with stage IV disease at presentation by virtue of nodal disease survived longer than those with the same stage because of systemic organ metastases: 9.3 vs. 3 months, (p < 0.001).
Conclusions
Prognosis of patients with metastatic cervical nodes was not uniformly dismal. Up to 20% had reasonable survival after chemoradiation and surgical resection. Stage IV disease should be revised to segregate those with nodal and systemic metastases.




Similar content being viewed by others
References
American Joint Committe on Cancer. Esophagus. In Greene FL, ed. AJCC cancer staging manual/American Joint Committee on Cancer. New York: Springer, 2002, pp 91–95.
Ries LAGMD, Krapcho M, Mariotto A, Miller BA, Feuer EJ, Clegg L, et al. In Edwards BK, ed. SEER Cancer Statistics Review, 1975–2004. National Cancer Institute, 2007.
Lerut T, Nafteux P, Moons J, et al. Three-field lymphadenectomy for carcinoma of the esophagus and gastroesophageal junction in 174 R0 resections: impact on staging, disease-free survival, and outcome: a plea for adaptation of TNM classification in upper-half esophageal carcinoma. Ann Surg 2004;240(6):962–972. (discussion 972–974). doi:10.1097/01.sla.0000145925.70409.d7.
Altorki N. En-bloc esophagectomy—the three-field dissection. Surg Clin North Am 2005;85(3):611–619. xi. doi:10.1016/j.suc.2005.01.005.
Shimada H, Shiratori T, Okazumi S, et al. Surgical outcome of patients with thoracic esophageal cancer positive for cervical lymph nodes. Hepatogastroenterology 2007;54(73):100–103.
Gebski VBB, Smithers BM, Foo K, Zalcberg J, Simes J, Australasian Gastro-Intestinal Trials Group. Survival benefits from neoadjuvant chemoradiotherapy or chemotherapy in oesophageal carcinoma: a meta-analysis. Lancet Oncol 2007;8(3):226–234. doi:10.1016/S1470-2045(07)70039-6.
Kesler KA, Helft PR, Werner EA, et al. A retrospective analysis of locally advanced esophageal cancer patients treated with neoadjuvant chemoradiation therapy followed by surgery or surgery alone. Ann Thorac Surg 2005;79(4):1116–1121. doi:10.1016/j.athoracsur.2004.08.042.
Giuli R, Gignoux M. Treatment of carcinoma of the esophagus. Retrospective study of 2,400 patients. Ann Surg 1980;192(1):44–52. doi:10.1097/00000658-198007000-00008.
Law SWJ. Therapeutic options for esophageal cancer. J Gastroenterol Hepatol 2004;19(4):4–12. doi:10.1111/j.1440-1746.2004.03154.x.
Akiyama H, Tsurumaru M, Udagawa H, Kajiyama Y. Radical lymph node dissection for cancer of the thoracic esophagus. Ann Surg 1994;220(3):364–372. (discussion 372–373). doi:10.1097/00000658-199409000-00012.
Nishihira T, Hirayama K, Mori S. A prospective randomized trial of extended cervical and superior mediastinal lymphadenectomy for carcinoma of the thoracic esophagus. Am J Surg 1998;175(1):47–51. doi:10.1016/S0002-9610(97)00227-4.
Kato H, Watanabe H, Tachimori Y, Iizuka T. Evaluation of neck lymph node dissection for thoracic esophageal carcinoma. Ann Thorac Surg 1991;51(6):931–935.
Altorki N, Kent M, Ferrara C, Port J. Three-field lymph node dissection for squamous cell and adenocarcinoma of the esophagus. Ann Surg 2002;236(2):177–183. doi:10.1097/00000658-200208000-00005.
Law SY, Fok M, Wong J. Pattern of recurrence after oesophageal resection for cancer: clinical implications. Br J Surg 1996;83(1):107–111. doi:10.1002/bjs.1800830134.
Mariette C, Balon JM, Piessen G, et al. Pattern of recurrence following complete resection of esophageal carcinoma and factors predictive of recurrent disease. Cancer 2003;97(7):1616–1623. doi:10.1002/cncr.11228.
Dresner SM, Wayman J, Shenfine J, et al. Pattern of recurrence following subtotal oesophagectomy with two field lymphadenectomy. Br J Surg 2000;87(3):362–373. doi:10.1046/j.1365-2168.2000.01383-5.x.
Kitajima M, Kitagawa Y. Surgical treatment of esophageal cancer—the advent of the era of individualization. N Engl J Med 2002;347(21):1705–1709. doi:10.1056/NEJMe020130.
Author information
Authors and Affiliations
Corresponding author
Additional information
Discussion
Dr. Marco G. Patti (Chicago, Illinois): This is another great study that comes from one of the best centers in the world for the treatment of esophageal cancer, and over the years, data from the group of Professor Tong and Dr. Simon Law have had tremendous impact on the way this disease is treated.
Dr. Tong and his colleagues studied patients with intrathoracic squamous cell carcinoma and vert cervical node metastases considered a stage IVa. They hypothesize that, with multimodality treatment, chemoradiation therapy, followed by surgery, the prognosis of these patients could be improved. The patients had a high complication rate, but there were no deaths and the median survival was almost 35 months. In summary, I think that these results suggest that, in selected patients, the combination of chemoradiation therapy with salvage esophagectomy can result in a reasonable long-term survival.
I have the following questions for the authors.
Should we treat all patients with cervical lymph node metastases in this way or just the patients who respond to neoadjuvant therapy?
Second, considering that, in the Western world, most patients have an adenocarcinoma of the distal esophagus, should we extrapolate your data and treat in a similar way patients who have celiac or para-aortic nodule involvement?
And finally, how would you modify the staging system?
Again, congratulations on this very nice study and on your presentation.
Dr. Daniel K. Tong (Hong Kong, China): For your first question, patients with cervical nodal metastasis are a heterogeneous group, comprising those with or without systemic (organ) metastases and also those with locally resectable or unresectable disease. Patients with systemic metastases should be given palliative treatment only and surgical resection is not indicated. For those without systemic metastases, responders to neoadjuvant therapy will often convert locally unresectable or borderline resectable to potentially “curative” resections. In selected non-responders, potentially “curative” resections, i.e., gross tumor clearance achieved, can still be carried out. Our policy is therefore to resect whenever potentially “curative” resections can be performed. If residual disease is too advanced, such as invading to adjacent structures like the carotid artery, surgery is not indicated. Decision should be individualized.
For your second question: In our patient population of only squamous cell cancers, patients with lower third tumors and cervical nodal metastases were also included. There was no apparent difference in outcome between these patients and those with more proximally located cancers. We in Asia do not really have a significant number of patients with Barrett’s adenocarcinoma of the distal esophagus. But for our possibility with distal squamous cell cancers and obvious celiac nodal metastases, our policy is also to treat upfront with chemoradiation and then consider surgical resection afterwards. There are two caveats to this: first, the diagnosis of celiac node is sometimes not certain; “celiac nodes” often turn out to be “left gastric or paragastric” in location, and the disease stage would be different. And second, similar to the situation in the neck, a celiac node can be a 1-cm node that can be easily removed vs. a massive celiac node that has enveloped the whole celiac axis where a curative resection is not possible. So again decision to operate has to be individualized.
For the modification of the staging system, we believe that cervical nodes should be classified as regional disease. The trend in other gastrointestinal cancers is to stage N disease according to the number of nodes involved; we think it would be the same for esophageal cancer.
Rights and permissions
About this article
Cite this article
Tong, D.KH., Kwong, D.L.W., Law, S. et al. Cervical Nodal Metastasis from Intrathoracic Esophageal Squamous Cell Carcinoma is not Necessarily an Incurable Disease. J Gastrointest Surg 12, 1638–1645 (2008). https://doi.org/10.1007/s11605-008-0654-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-008-0654-0