Abstract
For half a century, controlled hypotension has been used to reduce bleeding and the need for blood transfusions, and provide a satisfactory bloodless surgical field. It has been indicated in oromaxillofacial surgery (mandibular osteotomy, facial repair), endoscopic sinus or middle ear microsurgery, spinal surgery and other neurosurgery (aneurysm), major orthopaedic surgery (hip or knee replacement, spinal), prostatectomy, cardiovascular surgery and liver transplant surgery.
Controlled hypotension is defined as a reduction of the systolic blood pressure to 80–90mm Hg, a reduction of mean arterial pressure (MAP) to 50–65mm Hg or a 30% reduction of baseline MAP.
Pharmacological agents used for controlled hypotension include those agents that can be used successfully alone and those that are used adjunctively to limit dosage requirements and, therefore, the adverse effects of the other agents. Agents used successfully alone include inhalation anaesthetics, sodium nitroprusside, nitroglycerin, trimethaphan camsilate, alprostadil (prostaglandin E1), adenosine, remifentanil, and agents used in spinal anaesthesia. Agents that can be used alone or in combination include calcium channel antagonists (e.g. nicardipine), β-adrenoceptor antagonists (β-blockers) [e.g. propranolol, esmolol] and fenoldopam. Agents that are mainly used adjunctively include ACE inhibitors and clonidine.
New agents and techniques have been recently evaluated for their ability to induce effective hypotension without impairing the perfusion of vital organs. This development has been aided by new knowledge on the physiology of peripheral microcirculatory regulation. Apart from the adverse effects of major hypotension on the perfusion of vital organs, potent hypotensive agents have their own adverse effects depending on their concentration, which can be reduced by adjuvant treatment. Care with use limits the major risks of these agents in controlled hypotension; risks that are generally less important than those of transfusion or alternatives to transfusion.
New hypotensive drugs, such as fenoldopam, adenosine and alprostadil, are currently being evaluated; however, they have disadvantages and a high treatment cost that limits their development in this indication.
New techniques of controlled hypotension subscribe to the use of the natural hypotensive effect of the anaesthetic drug with regard to the definition of the ideal hypotensive agent. It must be easy to administer, have a short onset time, an effect that disappears quickly when administration is discontinued, a rapid elimination without toxic metabolites, negligible effects on vital organs, and a predictable and dose-dependent effect. Inhalation agents (isoflurane, sevoflurane) provide the benefit of being hypnotic and hypotensive agents at clinical concentrations, and are used alone or in combination with adjuvant agents to limit tachycardia and rebound hypertension, for example, inhibitors of the autonomic nervous system (clonidine, β-blockers) or ACE inhibitors. When they are used alone, inhalation anaesthetics require high concentrations for a significant reduction in bleeding that can lead to hepatic or renal injury.
The greatest efficacy and ease-of-use to toxicity ratio is for techniques of anaesthesia that associate analgesia and hypotension at clinical concentrations without the need for potent hypotensive agents. The first and oldest technique is epidural anaesthesia, but depending on the surgery, it is not always appropriate. The most recent satisfactory technique is a combination treatment of remifentanil with either propofol or an inhalation agent (isoflurane, desflurane or sevoflurane) at clinical concentrations. In light of the current literature, and because of their safety and ease of use, these two techniques are preferred.










Similar content being viewed by others
References
Leigh JM. The history of controlled hypotension. Br J Anaesth 1975; 47 (7): 745–9
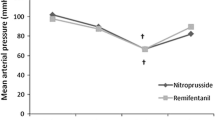
Degoute CS, Ray MJ, Manchon M, et al. Remifentanil and controlled hypotension; comparison with sodium nitroprusside or esmolol during tympanoplasty. Can J Anesth 2001 Jan; 48 (1): 20–7
Thompson GE, Miller RD, Stevens WC, et al. Hypotensive anesthesia for total hip arthroplasty: a study of blood loss and organ function (brain, heart, liver, and kidney). Anesthesiology 1978; 48: 91–6
Miller JM, Ren TY, Nuttal AL. Studies of inner ear blood flow in animals and human beings. Otolaryngol Head Neck Surg 1995; 112: 101–13
Boezaart AP, van der Merwe J, Coetzee A. Comparison of sodium sodium nitroprusside-and esmolol-induced controlled hypotension for functional endoscopic sinus surgery. Can J Anaesth 1995; 42: 373–6
Schindler I, Andel H, Leber J, et al. Moderate induced hypotension provides satisfactory operating conditions in maxillofacial surgery. Acta Anaesthesiol Scand 1994; 38: 384–7
Pilli G, Guzeldemir ME, Bayhan N. Esmolol for hypotensive anesthesia in middle ear surgery. Acta Anaesthesiol Belg 1996; 47: 85–91
Marchai JM, Gomez-Luque A, Martos-Crespo F, et al. Clonidine decreases intraoperative bleeding in middle ear microsurgery. Acta Anaesthesiol Scand 2001; 45: 627–33
Degoute CS, Ray MJ, Gueugniaud PY, et al. Remifentanil induces consistent and sustained controlled hypotension in children during middle ear surgery. Can J Anesth 2003; 50 (3): 270–6
Dal D, Celiker V, Ozer E, et al. Induced hypotension for tympanoplasty: a comparison of desflurane, isoflurane and sevoflurane. Eur J Anaesthesiol 2004; 21 (11): 902–6
Eckenhoff JE, Rich JC. Clinical experiences with deliberate hypotension. Anesth Analg 1966; 45: 21–8
Enlund M, Andersson J, Hartvig P, et al. Cerebral normoxia in the rhesus monkey during isoflurane-or propofol-induced hypotension and hypocapnia, despite disparate blood-flow patterns: a positron emission tomography study. Acta Anaesthesiol Scand 1997; 41: 1002–10
Hersey SL, O’Dell NE, Lowe S, et al. Nicardipine versus sodium nitroprusside for controlled hypotension during spinal surgery in adolescents. Anesth Analg 1997; 84: 1239–44
Juelsgaard P, Larsen UT, Sorensen JV, et al. Hypotensive epidural anesthesia in total knee replacement without tourni-quet: reduced blood loss and transfusion. Reg Anesth Pain Med 2001;26: 105–10
Yukioka H, Asada K, Fujimori M, et al. Prostaglandin El as a hypotensive drug during general anesthesia for total hip re-placement. J Clin Anesth 1993; 5: 310–4
Sharrock NE, Mineo R, Urquhart B, et al. The effect of two levels of hypotension on intraoperative blood loss during total hip arthroplasty performed under lumbar epidural anesthesia. Anesth Analg 1993; 76: 580–4
Karakaya D, Ustun E, Tur A, et al. Acute normovolemic hemodilution and nitroglycerin-induced hypotension: comparative effects on tissue oxygenation and allogeneic blood transfusion requirement in total hip arthroplasty. J Clin Anesth 1999; 11: 368–74
Niemi TT, Pitkanen M, Syrjala M, et al. Comparison of hypotensive epidural anaesthesia and spinal anaesthesia on blood loss and coagulation during and after total hip arthroplasty. Acta Anaesthesiol Scand 2000; 44: 457–64
Boldt J, Weber A, Mailer K, et al. Acute normovolaemic haemodilution vs controlled hypotension for reducing the use of allogeneic blood in patients undergoing radical prostatectomy. Br J Anaesth 1999; 82: 170–4
Suttner SW, Piper SN, Lang K, et al. Cerebral effects and blood sparing efficiency of sodium sodium nitroprusside-induced hypotension alone and in combination with acute normovolaemic haemodilution. Br J Anaesth 2001; 87: 699–705
Kerr AR. Anaesthesia with profound hypotension for middle ear surgery. Br J Anaesth 1977; 49: 447–52
Sharrock NE, Mineo R, Urquhart B. Haemodynamic effects and outcome analysis of hypotensive anaesthesia in controlled hypertensive patients undergoing total hip arthroplasty. Br J Anaesth 1991; 67: 17–25
Schreiber GB, Busch MP, Kleinman SH, et al. The risk of transfusion-transmitted viral infections. The Retrovirus Epidemiology Donor Study. N Engl J Med 1996; 334: 1685–90
Kasper SM, Baumann M, Radbruch L, et al. A pilot study of continuous ambulatory electrocardiography in patients donating blood for autologous use in elective coronary artery bypass grafting. Transfusion 1997; 37: 829–35
Hardy JF, Bélisle S, Décary F. Cardiac surgical patients must not be denied the benefits of autologous blood predonation. Can J Anaesth 1994; 41: 1021–6
Report of the Expert Working Group. Guidelines for red blood cell and plasma transfusion for adults and children. CMAJ 1997; 156 Suppl.: S1-23
Etchason J, Petz L, Keeler E, et al. The cost effectiveness of preoperative autologous donations. N Engl J Med 1995; 332: 719–24
Feldman JM, Roth JV, Bjoraker DG. Maximum blood savings by acute normovolemic hemodilution. Anesth Analg 1995; 80: 108–13
Bryson GL, Laupacis A, Wells GA. Does acute normovolemic hemodilution reduce perioperative allogenic transfusion? A meta-analysis. The International Study of Perioperative Trans-fusion. Anesth Analg 1998; 86: 9–15
Matot I, Scheinin O, Jurim O, et al. Effectiveness of acute normovolemic hemodilution to minimize allogenic blood transfusion in major liver resections. Anesthesiology 2002; 97: 794–800
Williamson KR, Taswell HF. Intraoperative blood salvage: a review. Transfusion 1991; 31: 662–75
Perseghin P, Vigano M, Rocco G, et al. Effectiveness of leukocyte filters in reducing tumor cell contamination after intraoperative blood salvage in lung cancer patients. Vox Sang 1997; 72: 221–4
Ezzedine H, Baele P, Robert A. Bactériologie quality of in-traoperative autotransfusion. Surgery 1991; 109: 259–64
Siller TA, Dickson JH, Erwin WD. Efficacy and cost considerations of intraoperative autologous transfusion in spinal fusion for idiopathic scoliosis with predeposited blood. Spine 1996; 21: 848–52
Kang YG, Aggarwal S, Virji M, et al. Clinical evaluation of autotransfusion during liver transplantation. Anesth Analg 1991; 72: 94–100
Bull BS, Bull MH. The salvage blood syndrome: a sequel to mechanochemical activation of platelets and leucocytes? Blood Cells 1990; 16: 5–23
Guay J, Reineberg C, Poitras B, et al. A trial of desmopressin to reduce blood loss in patients undergoing spinal fusion for idiopathic scoliosis. Anesth Analg 1992; 75: 405–12
Theroux MC, Corddry DH, Tietz AE, et al. A study of desmopressin and blood loss during spinal fusion for neuro-muscular scoliosis: a randomized, double-blinded study. Anesthesiology 1997; 87: 260–7
Janssens M, Joris J, David JL, et al. High-dose aprotinin reduces blood loss in patients undergoing total hip replacement. Anes-thesiology 1994; 80: 23–9
Thorpe CM, Murphy W, Logan M. Use of aprotinine in knee replacement surgery. Br J Anaesth 1994; 73: 408–10
Peters DC, Noble S. Aprotinin: an update of its pharmacology and therapeutic use in open heart surgery and coronary artery bypass surgery. Drugs 1999; 57 (2): 233–60
Dietrich W, Späth P, Ebell A, et al. Prevalence of anaphylactic reactions to aprotinin: analysis of two hundred forty-eight reexposures to aprotinine in heart operations. J Thorac Cardi-ovasc Surg 1997; 113: 194–201
Diefenbach C, Abel M, Limpers B, et al. Fatal anaphylactic shock after aprotinin reexposure in cardiac surgery. Anesth Analg 1995; 80: 830–1
Capdevila X, Calvet Y, Biboulet P, et al. Aprotinin decreases blood loss and homologous transfusions in patients undergoing major orthopaedic surgery. Anesthesiology 1998; 88: 50–7
Brown RS, Thwaites BK, Mongan PD. Tranexamic acid is effective in decreasing postoperative bleeding and transfusions in primary coronary artery bypass operations: a double-blind, randomized, placebo-controlled trial. Anesth Analg 1997; 85: 963–70
Kaspar M, Ramsay MAE, Nguyen AT, et al. Continuous small-dose tranexamic acid reduces fibrinolysis but not transfusion requirements during orthotopic liver transplantation. Anesth Analg 1997; 85: 281–5
Hiippala ST, Strid LJ, Wennerstrand MI, et al. Tranexamic acid radically decreases blood loss and transfusions associated with total knee arthroplasty. Anesth Analg 1997; 84: 839–44
Enderby GEH. Controlled circulation with hypotensive drugs and posture to reduce bleeding during surgery: preliminary results with pentamethonium iodide. Lancet 1950; I: 1145–7
Kallinen J, Didier A, Miller JM, et al. The effects of CO2 and O2 gas mixtures on laser Doppler measured cochlear and skin blood flow in guinea pigs. Hear Res 1991; 55: 255–62
Carpenter RL, Caplan RA, Brown DL, et al. Incidence and risk factors for side effects of spinal anesthesia. Anesthesiology 1992; 76: 906–16
Sharrock NE, Bading B, Mineo R, et al. Deliberate hypotensive anesthesia for patients with normal and low cardiac output. Anesth Analg 1994; 79 (5): 899–904
Eroglu A, Uzunlar H, Erciyes N. Comparison of epidural anes-thesia and hypotensive total intravenous anesthesia on in-traoperative blood loss during total hip replacement. J Clin Anesth 2005; 17 (6): 420–5
Tobias JD. Sevoflurane for controlled hypotension during spinal surgery: preliminary experience in five adolescents. Paediatr Anaesth 1998; 8: 167–70
Sato J, Saito S, Takahashi T, et al. Sevoflurane and nitrous oxide anaesthesia suppresses heart rate variabilities during deliberate hypotension. Eur J Anaesthesiol 2001; 18: 805–10
Tomiyasu S, Hara T, Hasuo H, et al. Comparative analysis of systemic and coronary hemodynamics during sevoflurane-and isoflurane-induced hypotension in dogs. J Cardiovasc Pharmacol 1999; 33: 741–7
Stoelting RK. The hemodynamic effects of pancuronium and dtubocurarine in anesthetized patients. Anesthesiology 1972; 36: 612–5
Anderson M. Posterior spinal fusion with Harrington rod instrumentation using ‘balanced anesthesia’. South Med J 1978; 71: 660–1
Purdham RS. Reduced blood loss with hemodynamic stability during controlled hypotensive anesthesia for LeFort I maxillary osteotomy using high-dose fentanyl: a retrospective study. CRNA 1996; 7: 33–46
Eberhart LH, Folz BJ, Wulf H, et al. Intravenous anesthesia provides optimal surgical conditions during microscopic and endoscopic sinus surgery. Laryngoscope 2003; 113 (8): 1369–73
Manola M, De Luca E, Moscillo L, et al. Using remifentanil and sufentanil in functional endoscopic sinus surgery to improve surgical conditions. ORL J Otorhinolaryngol Relat Spec 2005; 67 (2): 83–6
Amaranath L, Kellermeyer WF Jr. Tachyphylaxis to sodium sodium nitroprusside. Anesthesiology 1976; 44: 345–8
Khambatta HF, Stone JG, Khan E. Hypertension during anesthesia on discontinuation of sodium sodium nitroprusside-induced hypotension. Anesthesiology 1979; 51: 127–30
Rowe GG, Henderson RH. Systemic and coronary hemodynamic effects of sodium sodium nitroprusside. Am Heart J 1974; 87: 83–7
Michenfelder JD, Milde JH. The interaction of sodium sodium nitroprusside hypotension and isoflurane in determining cerebral vasculature effects. Anesthesiology 1988; 69: 870–5
Hines R, Barash P. Infusion of sodium sodium nitroprusside induces platelet dysfunction in vitro. Anesthesiology 1989; 70: 611–5
Tinker JH, Michenfelder JD. Sodium sodium nitroprusside: pharmacology, toxicology and therapeutics. Anesthesiology 1976; 45: 340–54
Michenfelder JD, Theye RA. Canine systemic and cerebral effects of hypotension induced by hemorrhage, trimetaphan, halothane or sodium nitroprusside. Anesthesiology 1977; 46: 188–95
Khambatta HJ, Stone JG, Khan E. Propranolol alters renine release during sodium nitroprusside-induced hypotension and prevents hypertension on discontinuation of sodium nitroprusside. Anesth Analg 1981; 60: 569–73
Woodside J Jr, Garner L, Bedford RF, et al. Captopril reduces the dose requirement for sodium sodium nitroprusside-induced hypotension. Anesthesiology 1984; 60: 413–7
Heesen M, Dietrich GV, Boldt J, et al. Beta 2-adrenoceptor density of human lymphocytes after sodium nitroprusside-induced hypotension. Anesth Analg 1995; 81: 1250–4
Dietrich GV, Heesen M, Boldt J, et al. Platelet function and adrenoceptors during and after induced hypotension using sodium nitroprusside. Anesthesiology 1996; 85: 1334–40
Suttner SW, Boldt J, Schmidt CC, et al. The effects of sodium sodium nitroprusside-induced hypotension on splanchnic perfusion and hepatocellular integrity. Anesth Analg 1999; 89: 1371–7
Bernard JM, Moren J, Demeure D, et al. Diltiazem reduces the dose requirement for sodium nitroprusside-induced hypotension. Anesth Analg 1993; 77: 318–23
Tohmo H, Karanko M, Scheinin M, et al. Enalapril premedication attenuates the blood pressure response to trachéal intubation and stabilizes postoperative blood pressure after controlled hypotension with sodium sodium nitroprusside in neurovascular patients. J Neurosurg Anesthesiol 1993; 5: 13–21
Piper SN, Suttner SW, Schmidt CC, et al. Acute phase response to sodium nitroprusside-induced controlled hypotension in patients undergoing radical prostatectomy. Anaesthesia 2000; 55: 131–6
Vatner SF, Higgins CB, Milland RW, et al. Direct and reflex effects of nitroglycerin on coronary and left ventricular dynamics in conscious dogs. J Clin Invest 1972; 51: 2872–82
Habazettl H, Vollmar B, Christ M, et al. Heterogeneous microvascular coronary vasodilatation by adenosine and nitroglycerin in dogs. J Appl Physiol 1994; 76: 1951–60
Rogers MC, Hamburger C, Owen K, et al. Intracranial pressure during nitroglycerin-induced hypotension. Anesthesiology 1979; 51: 227–9
Werns SW, Rote WE, Davis JH, et al. Nitroglycerin inhibits experimental thrombosis and reocclusion after thrombolysis. Am Heart J 1994; 127: 727–37
Aoki H, Inoue M, Mizobe T, et al. Platelet function is inhibited by nitric oxide liberation during nitroglycerin-induced hypotension anaesthesia. Br J Anaesth 1997; 79: 476–81
Graybar G, Lobar D, Jones J. Comparison of sodium nitroprusside and nitroglycerin in perioperative blood loss with open heart surgery. Crit Care Med 1974; 2: 240–2
Kadam PP, Saksena SG, Jagtap SR, et al. Hypotensive anaesthesia for spine surgery: nitroglycerin vs. halothane. J Postgrad Med 1993; 39: 26–8
Bembridge JL, Moss E, Grummitt RM, et al. Comparison of propofol with enflurane during hypotensive anaesthesia for middle ear surgery. Br J Anaesth 1993; 71: 895–7
Sollevi A, Lagerkranser M, Irestedt L, et al. Controlled hypotension with adenosine in cerebral aneurysm surgery. Anesthesiology 1984; 61: 400–5
Kien ND, White DA, Reitan JA, et al. Cardiovascular function during controlled hypotension induced by adenosine triphosphate or sodium sodium nitroprusside in the anesthetized dog. Anesth Analg 1987; 66: 103–10
Van Aken H, Puchstein C, Anger C, et al. Changes in intracranial pressure and compliance during adenosine triphosphate-induced hypotension in dogs. Anesth Analg 1984; 63: 381–5
Lagerkranser M, Bergstrand G, Gordon E, et al. Cerebral blood flow and metabolism during adenosine-induced hypotension in patients undergoing cerebral aneurysm surgery. Acta Anaesthesiol Scand 1989; 33: 15–20
Belardinelli L, Mattos EC, Berne RM. Evidence for adenosine mediation of atrioventricular block in the ischemic canine myocardium. J Clin Invest 1981; 68: 195–205
Zall S, Eden E, Winso I, et al. Controlled hypotension with adenosine or sodium sodium nitroprusside during cerebral aneurysm surgery: effects on renal hemodynamics, excretory function, and renine release. Anesth Analg 1990; 71: 631–6
Barrett RJ, Wright KF. A selective adenosine A1 receptor antagonist attenuates renal dysfunction during controlled hypotension with adenosine in rats. Anesth Analg 1994; 79: 460–5
Aggarwal A, Farber NE, Warltier DC. Intraoperative bronchospasm caused by adenosine. Anesthesiology 1993; 79: 1132–5
Noma T, Ichinohe T, Kaneko Y. Inhibition of physiologic stress responses by regional nerve block during orthognathic surgery under hypotensive anesthesia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1998; 86: 511–5
Yamaguchi H, Harukuni I, Dohi S, et al. Lumbar epidural anesthesia prevents prostaglandine E1-induced diuretic effect in enflurane anesthetized patients. Can J Anaesth 1993; 40: 619–24
Abe K, Demizu A, Kamada K, et al. Local cerebral blood flow with prostaglandine E1 or trimetaphan during cerebral aneurysm clip ligation. Can J Anaesth 1991; 38: 831–6
Abe K, Iwanaga H, Yoshiya I. Carbon dioxide reactivity and local cerebral blood flow during prostaglandine E1-or nitroglycerin-induced hypotension. Can J Anaesth 1992; 39: 799–804
Kadoi Y, Saito S, Kunimoto F, et al. Cerebral oxygenation during prostaglandin E1 induced hypotension. Can J Anaesth 1998; 45: 860–4
Fukusaki M, Maekawa T, Yamaguchi K, et al. Combined effects of prolonged prostaglandin E1-induced hypotension and haemodilution on human hepatic function. Eur J Anaesthesiol 1997; 14: 157–63
Fukusaki M, Maekawa T, Kobayashi I, et al. Catecholamine and renin-angiotensin response during controlled hypotension induced by prostaglandin E1 combined with hemodilution during isoflurane anesthesia. J Clin Anesth 1997; 9: 321–7
Abe K, Kakiuchi M, Shimada Y. Epidural blood flow during prostaglandin E1 or trimetaphan induced hypotension. Pros-taglandins Leukot Essent Fatty Acids 1993; 49: 873–6
Abe K, Nishimura M, Kakiuchi M. Spinal cord blood flow during prostaglandin El induced hypotension. Prostaglandins Leukot Essent Fatty Acids 1994; 51: 173–6
Tsubo T, Hashimoto Y, Dobashi N, et al. Haemodynamic changes during induced hypotension: comparison of trimetaphan with prostaglandin E1 assessed using transoesophageal echocardiography. Can J Anaesth 1995; 42: 126–9
Shiraishi Y, Mochizuki T, Ikeda K. Oxygen uptake and carbon dioxide elimination during controlled hypotension induced by prostaglandin El or nitroglycerin. Br J Anaesth 1994; 72: 439–42
Yukioka H, Asada K, Fujimori M, et al. Prostaglandin El as a hypotensive drug during general anesthesia for total hip replacement. J Clin Anesth 1993; 5: 310–4
Zimpfer M, Fitzal S, Tonczar L. Verapamil as a hypotensive agent during neuroleptanalgesia. Br J Anaesth 1981; 53: 885–9
Leenen FH, Ruzicka M, Huang BS. Central sympathoinhibitory effects of calcium channel blockers. Curr Hypertens Rep 2001; 3: 314–21
Bernard JM, Moren J, Demeure D, et al. Diltiazem reduces the dose requirement for sodium nitroprusside-induced hypotension. Anesth Analg 1993; 77: 318–23
Takeda S, Ozawa Y, Tomaru T. Haemodynamic effects of hypotension induced by KRN2391 and nicardipine in isoflurane anaesthetized dogs. Can J Anaesth 1997; 44: 1002–7
Kimura T, Ito M, Komatsu T, et al. Heart rate and blood pressure power spectral analysis during calcium channel blocker induced hypotension. Can J Anaesth 1999; 46: 1110–6
Endoh H, Honda T, Ohashi S, et al. The influence of nicardipine-, and prostaglandine El-induced hypotension on cerebral pressure autoregulation in adult patients during propofol-fentanyl anesthesia. Anesth Analg 2002; 94: 169–73
Bernard JM, Pinaud M, François T, et al. Deliberate hypotension with nicardipine or sodium nitroprusside during total hip arthroplasty. Anesth Analg 1991; 73: 341–5
Bernard JM, Passuti N, Pinaud M. Long term hypotensive technique with nicardipine and sodium nitroprusside during isoflurane anesthesia for spinal surgery. Anesth Analg 1992; 75: 179–85
Lee TC, Buerkle H, Wang CJ, et al. Effect of isoflurane versus nicardipine on blood flow of lumbar paraspinal muscles during controlled hypotension for spinal surgery. Spine 2001; 26: 105–9
Hersey SL, O’Dell NE, Lowe S, et al. Nicardipine versus sodium nitroprusside for controlled hypotension during spinal surgery in adolescents. Anesth Analg 1997; 84: 1239–44
Tobias JD, Hersey S, Mencio GA, et al. Nicardipine for controlled hypotension during spinal surgery. J Pediatr Orthop 1996; 16: 370–3
Tobias JD. Nicardipine for controlled hypotension during orthognathic surgery. Plast Reconstr Surg 1997; 99: 1539–43
Aronson S, Goldberg LI, Roth S, et al. Preservation of renal blood flow during hypotension induced with fenoldopam in dogs. Can J Anaesth 1990; 37: 380–4
Brogden RN, Markham A. Fenoldopam: a review of its pharma-codynamic and pharmacokinetic properties and intravenous clinical potential in the management of hypertensive urgencies and emergencies. Drugs 1997; 54: 634–50
Halpenny M, Lakshmi S, O’Donnell A, et al. The effects of fenoldopam on coronary conduit blood flow after artery bypass graft surgery. J Cardiothorac Vasc Anesth 2001; 15: 72–6
Brath PC, MacGregor DA, Ford JG, et al. Dopamine and intraocular pressure in critically ill patients. Anesthesiology 2000; 93: 1398–400
Halpenny M, Markos F, Snow HM, et al. Effects of prophylactic fenoldopam infusion on renal blood flow and renal tubular function during acute hypovolemia in anesthetized dogs. Crit Care Med 2001; 29: 911–3
Prielipp RC, Wall MH, Groban L, et al. Reduced regional and global cerebral blood flow during fenoldopam-induced hypo-tension in volunteers. Anesth Analg 2001; 93: 45–52
Tobias JD. Fenoldopam for controlled hypotension during spi-nal fusion in children and adolescents. Paediatr Anaesth 2000; 10: 261–6
Knight PR, Lane GA, Hensinger RN, et al. Catecholamine and renine-angiotensin response during hypotensive anesthesia induced by sodium sodium nitroprusside or trimethaphan camsylate. Anesthesiology 1983; 59: 248–53
Tsutsui T, Maekawa T, Goodchild C, et al. Cerebral blood flow distribution during induced hypotension with haemorrhage, trimetaphan or sodium nitroprusside in rats. Br J Anaesth 1995; 74: 686–90
McCubbin JW, Page IH. Nature of the hypotensive action of a thiophanium derivative (Ro 2-2222) in dogs. J Pharmacol Exp Ther 1952; 105: 437–42
Marchai JM, Gomez-Luque A, Martos-Crespo F, et al. Clonidine decreases intraoperative bleeding in middle ear microsurgery. Acta Anaesthesiol Scand 2001; 45: 627–33
Lee J, Lovell AT, Parry MG, et al. I.V. clonidine: does it work as a hypotensive agent with inhalation anaesthesia? Br J Anaesth 1999; 82: 639–40
Woodcock TE, Millard RK, Dixon J, et al. Clonidine premedication for isoflurane-induced hypotension: sympathoadrenal responses and a computer-controlled assessment of the vapour requirement. Br J Anaesth 1988; 60: 388–94
Toivonen J, Kaukinen S. Clonidine premedication: a useful adjunction producing deliberate hypotension. Acta Anaesth Scand 1990; 34: 653–6
Murakami K, Mammoto T, Kita T, et al. Oral clonidine reduces the requirement of prostaglandin E1 for induced hypotension. Can J Anaesth 1999; 46: 1043–7
Kolassa N, Beller KD, Sanders KH. Involvement of brain 5-HT1A receptors in the hypotensive response to urapidil. Am J Cardiol 1989; 64: 7–10D
Kolassa N, Beller KD, Sanders KH. Evidence for the interaction of urapidil with 5-HT1A receptors in the brain leading to a decrease in blood pressure. Am J Cardiol 1989; 63 (6): 36–9C
Toivonen J, Kuikka P, Kaukinen S. Effects of deliberate hypotension induced by labetalol with isoflurane on neuropsychological function. Acta Anaesthesiol Scand 1993 Jan; 37: 7–11
Matson AM, Shaw M, Loughnan BA, et al. Pituitary-adrenal, hormonal changes during induced hypotension with labetalol or isoflurane for middle-ear surgery. Acta Anaesthesiol Scand 1998; 42: 17–22
Ornstein E, Young WL, Ostapkovich N, et al. Are all effects of esmolol equally rapid in onset? Anesth Analg 1995; 81: 297–300
Shah N, Del Valle O, Edmondson R, et al. Esmolol infusion during sodium nitroprusside-induced hypotension: impact on hemodynamics, ventricular performance, and venous admixture. J Cardiothorac Vasc Anesth 1992; 6: 196–200
Blau WS, Kafer ER, Anderson JA. Esmolol is more effective than sodium nitroprusside in reducing blood loss during orthognathic surgery. Anesth Analg 1992; 75: 172–8
Fahmi NR. Impact of oral captopril or propranolol on sodium nitroprusside: induced hypotension [abstract]. Anesthesiology 1984; 61: A41
Jacobi KE, Bohm BE, Rickauer AJ, et al. Moderate controlled hypotension with sodium sodium nitroprusside does not improve surgical conditions or decrease blood loss in endoscopie sinus surgery. J Clin Anesth 2000; 12: 202–7
Abdulatif M. Sodium sodium nitroprusside induced hypotension: haemodynamic response and dose requirements during propofol or halothane anaesthesia. Anaesth Intensive Care 1994; 22: 155–60
Tobias JD. Controlled hypotension in children: a critical review of available agents. Paediatr Drugs 2002; 4: 439–53
Hackmann T, Friesen M, Allen S, et al. Clonidine facilitates controlled hypotension in adolescent children. Anesth Analg 2003; 96 (4): 976–81
Beaussier M, Paugam C, Deriaz H, et al. Haemodynamic stability during moderate hypotensive anaesthesia for spinal surgery: a comparison between desflurane and isoflurane. Acta Anaesthesiol Scand 2000; 44: 1154–9
Hara T, Fukusaki M, Nakamura T, et al. Renal function in patients during and after hypotensive anesthesia with sevoflurane. J Clin Anesth 1998; 10: 539–45
Fukusaki M, Miyako M, Hara T, et al. Effects of controlled hypotension with sevoflurane anaesthesia on hepatic function of surgical patients. Eur J Anaesthesiol 1999; 16: 111–6
Acknowledgements
The author would like to thank Mathias Degoute (University of PARIS IV-Sorbonne) for his contribution to the manuscript. No sources of funding were used to assist in the preparation of this review. The author has no conflicts of interest that are directly relevant to the content of this review.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Degoute, CS. Controlled Hypotension. Drugs 67, 1053–1076 (2007). https://doi.org/10.2165/00003495-200767070-00007
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003495-200767070-00007