Abstract
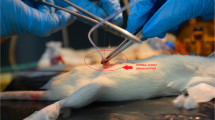
Effects of bilateral efferent duct ligation (EDL) on sperm motility and testicular endocrinology were investigated in adult male rats. Bilateral EDL was created surgically in adult male rats (EDL group) and shamoperated rats were used as control (control group). Five rats from each group were killed on d 3, 5, 7, 14, and 35 after the surgery. The sperm motility parameters were determined by a computer-assisted sperm analysis system using sperm collected from the cauda epididymis. Concentrations of spermatozoa in epididymis and testis were counted. The motility of sperm decreased remarkably in EDL rats compared with controls on 5 d after the operation. Four sperm motility parameters—straight velocity (VSL), deviation of the sperm head from the mean trajectory (ALH, mean), the maximum amplitude of lateral head displacement (ALH, max) and curvilinear velocity (VCL)—increased on 3 d after the operation, and followed by a subsequent decline 5 and 7 dlater. Concentrations of sperm significantly decreased in both testes and epididymis from 3 and 5 d after the operation. Plasma concentrations of FSH and LH increased significantly in EDL rats from 5 and 7 d after the operation, whereas plasma concentrations of immunoreactive (ir)-inhibin, inhibin B, and testosterone decreased. Testicular content of irinhibin showed an initial increase on 3 d after the operation, followed by a subsequent decline to levels significantly below controls by d 7 postoperation. On the other hand, testicular contents of testosterone were significantly higher in the EDL group than the control group on d7–35 after the operation, whereas circulating levels of testosterone remained low. In the EDL testes, marked degenerative changes in the Sertoli cells and spermatogonia were observed, whereas Leydig cells showed clear hyperplasia. These results demonstrated that bilateral EDL induced a rapid reduction of sperm motility parameters during a short time. Present results also suggest that EDL first induces impairment of Sertoli cells function and this leads to reduction of sperm activity and secretion of inhibins. On the other hand, circulating levels of testosterone reduced after EDL and this leads to hypersecretion of LH. A large amount of LH resulted in a stimulation of Leydig cells hyperplasia.
Similar content being viewed by others
References
Waites, G. M. and Setchell, B. P. (1969). Some physiological aspects of the function of the testis. In: The gonads, McKerns, K. (ed.). Appleton-Century-Crofts. New York, pp. 649–714.
Setchell, B. P. and Waites, G. M. (1970). J. Endorcinol. 47, 81–86.
Anton, E. (1979). Fertil. Steril. 31, 187–194.
Smith, G. (1962). J. Endocrinol. 23, 285–299.
McEntee, K. (1990). Efferent ductules, epididymis, and deferent duct. In: Reproductive pathology of domestic mammals McEntee, K. (ed.). Academic Press. San Diego, CA, pp. 307–332.
Koskimies, A. I. and Kormano, M. (1975). J. Reprod. Fertil. 43, 345–348.
Brooks, D. E. (1981). Biol. Reprod. 25, 1099–1117.
Syntin, P., Dacheux, F., Druart, X., Gatti, J. L., Okamura, N., and Dacheux, J. L. (1996). Biol. Reprod. 55, 956–974.
Vreeburg, J. T., Holland, M. K., Cornwall, G. A. and Orgebin-Crist, M. C. (1990). Biol. Reprod. 43, 113–120.
Kirchhoff, C., Osterhoff, C., Pera, I., and Schroter, S. (1998). Andrologia 30, 225–232.
Boue, F., Lassalle, B., Duquenne C., et al. (1992). Mol. Reprod. Dev. 33, 470–480.
Zini, A., and Schlegel, P. N. (1997). J., Urol. 158, 659–663.
Lan, Z. J., Labus, J. C., and Hinton, B. T. (1998). Biol. Reprod. 58, 197–206.
Hermo, L., Xiaohong, S., and Morales, C. R. (2000). J. Androl. 21, 122–144.
Shabanowitz, R. B. and Killian, G. J. (1987). Biol. Reprod. 36, 753–768.
Holland, M. K., Vreeburg, J. T., and Orgebin-Crist, M. C. (1992). J. Androl. 13, 266–273.
Wong, P. Y. and Lee, W. M. (1983). Biol. Reprod. 28, 206–212.
Wishart, G. J. and Ashizawa, K. (1987). J. Reprod. Fertil. 80, 607–611.
Fan, X. and Robaire, B. (1998). Endocrinology 139, 2128–2136.
Jensen, T. K., Andersson, A. M., Hjollund, N. H., et al. (1997). J. Clin. Endocrinol. Metab. 82, 4059–4063.
Pierik, F. H., Van Ginneken, A. M., Dohle, G. R., Vreeburg, J. T., and Weber, R. F. (2000). Int. J. Androl. 23, 340–346.
Buzzard, J. J., Loveland, K. L., O'Bryan, M. K., et al. (2004). Endocrinology 145, 3532–3541.
Ozkan, K. U., Kucukaydin, M., Muhtaroglu, S., Kontas, O., and Karaca, F. (2003). Urol. Int. 71, 73–76.
Jin, W., Herath, C. B., Yoshida, M., et al. (2002). J. Androl. 23, 845–853.
Kondo, M., Udono, T., Jin, W., et al. (2000). Endocr. J. 47, 707–714.
Anthony, C. T., Danzo, B. J., and Orgebin-Crist, M. C. (1984). Endocrinology 114, 1413–1418.
Anthony, C. T., Danzo, B. J., and Orgebin-Crist, M. C. (1984) Endocrinology 114, 1419–1425.
Risbridger, G. P., Kerr, J. B., Peake, R. A., and de Kretser, D. M. (1981). Endocrinology 109, 1234–1241.
de Kretser, D. M. (1982). Int. J. Androl. 5, 11–17.
Strader, L. F., Linder, R. E., and Perreault, S. D. (1996). Reprod. Toxicol. 10, 529–533.
Meistrich, M. L. (1989). J. Am. Coll. Toxicol. 8, 551–567.
Hamada, T., Watanabe, G., Kokuho, T., et al. (1989). J. Endocrinol. 122, 697–704.
Taya, K., Watanabe, G., and Sasamoto, S. (1985). Jpn. J. Anim. Reprod. 31, 186–197.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ren, L., Medan, M.S., Li, C. et al. Effects of bilateral efferent duct ligation on sperm motility and secretion of FSH, LH, inhibin, and testosterone in adult male rats. Endocr 30, 151–160 (2006). https://doi.org/10.1385/ENDO:30:2:151
Received:
Revised:
Accepted:
Issue Date:
DOI: https://doi.org/10.1385/ENDO:30:2:151