Abstract
Background
A diagnosis of non-classic lobular carcinoma in situ (NC-LCIS) encompasses a variety of lesions with poorly characterized natural history. We evaluated upgrade rates and factors associated with upgrade to malignancy following a core biopsy diagnosis of NC-LCIS, and its natural history.
Methods
Upon Institutional Review Board approval, pathology databases were searched for NC-LCIS core biopsy diagnoses (carcinoma in situ [CIS], CIS with ductal and lobular features [CIS/DLF], pleomorphic LCIS [P-LCIS], variant LCIS [V-LCIS], LCIS with necrosis). Cases with available core and excision pathology were included, while cases with concurrent ipsilateral invasive carcinoma (IC), ductal carcinoma in situ (DCIS), and/or atypical ductal hyperplasia were excluded.
Results
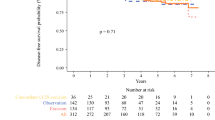
Overall, 121 NC-LCIS cases were identified from 1998 to 2017. We excluded 46 cases with concurrent cancer; 75 patients with 76 NC-LCIS core biopsy diagnoses followed by excision formed our study cohort. Median age was 56 years (range 41–83), and all imaging findings were classified as Breast Imaging Reporting and Data System 4; calcifications were the most common biopsy indication (80%). Excision yielded malignancy in 27 (36%) patients (IC 17, 63%; DCIS alone 10, 37%). We were unable to identify radiologic or pathologic features predictive of upgrade. Of 49 pure NC-LCIS cases, 15 (31%) had mastectomy, 9 (18%) had excision and radiation, and 25 (51%) had excision alone. At a median follow-up of 58 months (range 1–224), 1/25 (4%) patients with excision alone developed ipsilateral DCIS 14 months later.
Conclusions
In this series of NC-LCIS, 36% of cases were upgraded, supporting routine excision. We were unable to identify predictors of upgrade. Among 25 patients with pure NC-LCIS, only one patient developed a future ipsilateral cancer. Further study of the natural history of NC-LCIS is warranted.

Similar content being viewed by others
References
Lakhani SR, Ellis IO, Schnitt SJ, Tan PH, Van de Vijver M. WHO Classification of Tumours of the Breast, 4th ed. Lyon: IARC Press; 2012.
Fadare O, Dadmanesh F, Alvarado-Cabrero I, et al. Lobular intraepithelial neoplasia [lobular carcinoma in situ] with comedo-type necrosis: a clinicopathologic study of 18 cases. Am J Surg Pathol 2006;30:1445–53.
Alvarado-Cabrero I, Picon Coronel G, Valencia Cedillo R, Canedo N, Tavassoli FA. Florid lobular intraepithelial neoplasia with signet ring cells, central necrosis and calcifications: a clinicopathological and immunohistochemical analysis of ten cases associated with invasive lobular carcinoma. Arch Med Res 2010;41:436–41.
Tavassoli FA. Lobular neoplasia: evolution of its significance and morphologic spectrum. Int J Surg Pathol 2010;18(3 Suppl):174S–7S.
Shin SJ, Lal A, De Vries S, et al. Florid lobular carcinoma in situ: molecular profiling and comparison to classic lobular carcinoma in situ and pleomorphic lobular carcinoma in situ. Hum Pathol 2013;44:1998–2009.
Frost AR, Tsangaris TN, Silverberg SG. Pleomorphic lobular carcinoma in situ. Pathol Case Rev 1996;1:27–30.
Sneige N, Wang J, Baker BA, Krishnamurthy S, Middleton LP. Clinical, histopathologic, and biologic features of pleomorphic lobular (ductal-lobular) carcinoma in situ of the breast: a report of 24 cases. Mod Pathol 2002;15:1044–50.
Gomes DS, Porto SS, Balabram D, Gobbi H. Inter-observer variability between general pathologists and a specialist in breast pathology in the diagnosis of lobular neoplasia, columnar cell lesions, atypical ductal hyperplasia and ductal carcinoma in situ of the breast. Diagn Pathol 2014;9:121.
Sullivan ME, Khan SA, Sullu Y, Schiller C, Susnik B. Lobular carcinoma in situ variants in breast cores: potential for misdiagnosis, upgrade rates at surgical excision, and practical implications. Arch Pathol Lab Med 2010;134:1024–8.
Georgian-Smith D, Lawton TJ. Calcifications of lobular carcinoma in situ of the breast: radiologic-pathologic correlation. AJR Am J Roentgenol 2001;176:1255–9.
Lavoue V, Graesslin O, Classe JM, Fondrinier E, Angibeau H, Leveque J. Management of lobular neoplasia diagnosed by core needle biopsy: study of 52 biopsies with follow-up surgical excision. Breast 2007;16:533–9.
Chivukula M, Haynik DM, Brufsky A, Carter G, Dabbs DJ. Pleomorphic lobular carcinoma in situ (PLCIS) on breast core needle biopsies: clinical significance and immunoprofile. Am J Surg Pathol 2008;32:1721–6.
Carder PJ, Shaaban A, Alizadeh Y, Kumarasuwamy V, Liston JC, Sharma N. Screen-detected pleomorphic lobular carcinoma in situ (PLCIS): risk of concurrent invasive malignancy following a core biopsy diagnosis. Histopathology 2010;57:472–8.
Niell B, Specht M, Gerade B, Rafferty E. Is excisional biopsy required after a breast core biopsy yields lobular neoplasia? AJR Am J Roentgenol 2012;199:929–35.
Meroni S, Bozzini AC, Pruneri G, et al. Underestimation rate of lobular intraepithelial neoplasia in vacuum-assisted breast biopsy. Eur Radiol 2014;24:1651–8.
Flanagan MR, Rendi MH, Calhoun KE, Anderson BO, Javid SH. Pleomorphic lobular carcinoma in situ: radiologic-pathologic features and clinical management. Ann Surg Oncol 2015;22:4263–9.
Susnik B, Day D, Abeln E, et al. Surgical outcomes of lobular neoplasia diagnosed in core biopsy: prospective study of 316 cases. Clin Breast Cancer 2016;16:507–13.
Guo T, Wang Y, Shapiro N, Fineberg S. Pleomorphic lobular carcinoma in situ diagnosed by breast core biopsy: clinicopathologic features and correlation with subsequent excision. Clin Breast Cancer. 2018;18:e449–e454.
Downs-Kelly E, Bell D, Perkins GH, Sneige N, Middleton LP. Clinical implications of margin involvement by pleomorphic lobular carcinoma in situ. Arch Pathol Lab Med 2011;135:737–43.
De Brot M, Koslow Mautner S, Muhsen S, et al. Pleomorphic lobular carcinoma in situ of the breast: a single institution experience with clinical follow-up and centralized pathology review. Breast Cancer Res Treat 2017;165:411–20.
Khoury T, Karabakhtsian RG, Mattson D, et al. Pleomorphic lobular carcinoma in situ of the breast: clinicopathological review of 47 cases. Histopathology 2014;64:981–93.
King TA, Reis-Filho JS. Lobular neoplasia. Surg Oncol Clin N Am 2014;23:487–503.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
None.
Rights and permissions
About this article
Cite this article
Nakhlis, F., Harrison, B.T., Giess, C.S. et al. Evaluating the Rate of Upgrade to Invasive Breast Cancer and/or Ductal Carcinoma In Situ Following a Core Biopsy Diagnosis of Non-classic Lobular Carcinoma In Situ. Ann Surg Oncol 26, 55–61 (2019). https://doi.org/10.1245/s10434-018-6937-0
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-018-6937-0