Abstract
Background
Young breast cancer patients have a poorer prognosis, especially when their tumors are hormone receptor positive. We analyzed the association between Ki67 and age and the impact of these factors on outcomes in hormone receptor-positive breast cancer.
Methods
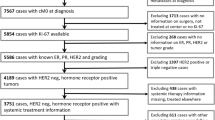
The records of 9,321 hormone receptor-positive invasive breast cancer patients from three large centers were retrospectively reviewed. Each institution separately assayed Ki67 level immunohistochemically. Univariate and multivariate analysis for recurrence-free survival (RFS) was performed on 4,738 patients from a single center.
Results
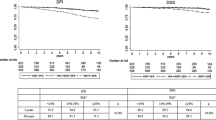
Ki67 level was inversely proportional to age in all three data sets and was significantly higher for younger patients (p < 0.001, 0.03, and <0.001, respectively). This correlation was seen only in the human epidermal growth factor receptor 2 (HER2)-negative population. Survival analysis showed that both very young age (<35 years) and high Ki67 level (≥10 %) were independent prognostic factors. Although young age was a worse prognostic indicator regardless of HER2 status, Ki67 index was associated with worse prognosis only in HER2-negative patients. When patients were stratified into those with low and high Ki67, young age remained a significant factor for RFS, with hazard ratios in these two Ki67 groups of 2.15 and 2.57, respectively (p < 0.001). Also, the young age/low Ki67 group had significantly poorer RFS than the older age/high Ki67 group (p < 0.001).
Conclusions
Ki67 level was higher in younger patients. However, very young patients had a poorer prognosis regardless of Ki67 level. Unknown biologic factors other than high cell proliferation might play a role in the aggressiveness of hormone receptor-positive breast cancer in very young patients.


Similar content being viewed by others
References
Narod SA. Breast cancer in young women. Nat Rev Clin Oncol. 2012;9:460–70.
Voogd AC, Nielsen M, Peterse JL, et al. Differences in risk factors for local and distant recurrence after breast-conserving therapy or mastectomy for stage I and II breast cancer: pooled results of two large European randomized trials. J Clin Oncol. 2001;19:1688–97.
Collins LC, Marotti JD, Gelber S, et al. Pathologic features and molecular phenotype by patient age in a large cohort of young women with breast cancer. Breast Cancer Res Treat. 2012;131:1061–6.
Rubino C, Arriagada R, Delaloge S, et al. Relation of risk of contralateral breast cancer to the interval since the first primary tumour. Br J Cancer. 2010;102:213–9.
Bharat A, Aft RL, Gao F, et al. Patient and tumor characteristics associated with increased mortality in young women (< or = 40 years) with breast cancer. J Surg Oncol. 2009;100:248–51.
Morrison DH, Rahardja D, King E, et al. Tumour biomarker expression relative to age and molecular subtypes of invasive breast cancer. Br J Cancer. 2012;107:382–7.
Anders CK, Hsu DS, Broadwater G, et al. Young age at diagnosis correlates with worse prognosis and defines a subset of breast cancers with shared patterns of gene expression. J Clin Oncol. 2008;26:3324–30.
Adami HO, Malker B, Holmberg L, et al. The relation between survival and age at diagnosis in breast cancer. N Engl J Med. 1986;315:559–63.
Azim HA Jr, Michiels S, Bedard PL, et al. Elucidating prognosis and biology of breast cancer arising in young women using gene expression profiling. Clin Cancer Res. 2012;18:1341–51.
Kim EK, Noh WC, Han W, et al. Prognostic significance of young age (<35 years) by subtype based on ER, PR, and HER2 status in breast cancer: a nationwide registry-based study. World J Surg. 2011;35:1244–53.
Ahn SH, Son BH, Kim SW, et al. Poor outcome of hormone receptor-positive breast cancer at very young age is due to tamoxifen resistance: nationwide survival data in Korea—a report from the Korean Breast Cancer Society. J Clin Oncol. 2007;25:2360–8.
Goldhirsch A, Colleoni M, Gelber RD. Endocrine therapy of breast cancer. Ann Oncol. 2002;13(Suppl 4):61–8.
Aebi S, Gelber S, Castiglione-Gertsch M, et al. Is chemotherapy alone adequate for young women with oestrogen-receptor-positive breast cancer? Lancet. 2000;355:1869–74.
Colleoni M, Rotmensz N, Peruzzotti G, et al. Role of endocrine responsiveness and adjuvant therapy in very young women (below 35 years) with operable breast cancer and node negative disease. Ann Oncol. 2006;17:1497–503.
Liu YR, Jiang YZ, Yu KD, et al. Different patterns in the prognostic value of age for breast cancer–specific mortality depending on hormone receptor status: a SEER population-based analysis. Ann Surg Oncol. In press.
Dai H, van’t Veer L, Lamb J, et al. (2005) A cell proliferation signature is a marker of extremely poor outcome in a subpopulation of breast cancer patients. Cancer Res. 65:4059–66.
Perreard L, Fan C, Quackenbush JF, et al. Classification and risk stratification of invasive breast carcinomas using a real-time quantitative RT-PCR assay. Breast Cancer Res. 2006;8:R23.
Choi DH, Kim S, Rimm DL, et al. Immunohistochemical biomarkers in patients with early-onset breast carcinoma by tissue microarray. Cancer J. 2005;11:404–11.
Colleoni M, Rocca A, Sandri MT, et al. Low-dose oral methotrexate and cyclophosphamide in metastatic breast cancer: antitumor activity and correlation with vascular endothelial growth factor levels. Ann Oncol. 2002;13:73–80.
Paik S, Shak S, Tang G, et al. A multigene assay to predict recurrence of tamoxifen-treated, node-negative breast cancer. N Engl J Med. 2004;351:2817–26.
Gerdes J, Lemke H, Baisch H, et al. Cell cycle analysis of a cell proliferation-associated human nuclear antigen defined by the monoclonal antibody Ki-67. J Immunol. 1984;133:1710–5.
Dowsett M, Nielsen TO, A’Hern R, et al. Assessment of Ki67 in breast cancer: recommendations from the International Ki67 in Breast Cancer Working Group. J Natl Cancer Inst. 2011;103:1656–64.
Yerushalmi R, Woods R, Ravdin PM, et al. Ki67 in breast cancer: prognostic and predictive potential. Lancet Oncol. 2010;11:174–83.
Jung SY, Han W, Lee JW, et al. Ki-67 expression gives additional prognostic information on St Gallen 2007 and Adjuvant! Online risk categories in early breast cancer. Ann Surg Oncol. 2009;16:1112–21.
Cha Y, Han SW, Seol H, et al. Immunohistochemical features associated with sensitivity to lapatinib-plus-capecitabine and resistance to trastuzumab in HER2-positive breast cancer. Anticancer Res. 2014;34:4275–80.
Han W, Kang SY; Korean Breast Cancer Society. Relationship between age at diagnosis and outcome of premenopausal breast cancer: age less than 35 years is a reasonable cut-off for defining young age-onset breast cancer. Breast Cancer Res Treat. 2010;119:193–200.
Cancello G, Maisonneuve P, Mazza M, et al. Pathological features and survival outcomes of very young patients with early breast cancer: how much is “very young”? Breast. 2013;22:1046–51.
Anders CK, Fan C, Parker JS, et al. Breast carcinomas arising at a young age: unique biology or a surrogate for aggressive intrinsic subtypes? J Clin Oncol. 2011;29:e18–20.
Polley MY, Leung SC, McShane LM, et al. An international Ki67 reproducibility study. J Natl Cancer Inst. 2013;105:1897–906.
Acknowledgment
Supported in part by a National Research Foundation of Korea (NRF) Grant funded by the Korea government (MSIP) (Grant 2012M3A9B2028834) and the SNUH Research Fund (Grant 04-2010-1150).
Disclosure
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kim, J., Han, W., Jung, SY. et al. The Value of Ki67 in Very Young Women with Hormone Receptor-Positive Breast Cancer: Retrospective Analysis of 9,321 Korean Women. Ann Surg Oncol 22, 3481–3488 (2015). https://doi.org/10.1245/s10434-015-4399-1
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-015-4399-1