Abstract
Background
This study aimed to determine the incidence, risk factors, and prognostic significance of retropharyngeal lymph node (RPLN) metastasis from malignancies of the oropharynx.
Methods
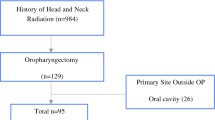
The study retrospectively analyzed 54 patients with oropharyngeal squamous cell carcinoma who underwent primary surgery-based treatment. Most of the patients had advanced stage (stage 3 or 4, 96.3 %) oropharyngeal cancer. Surgery alone was performed for 14 patients. Postoperative radiotherapy was administered to 14 patients and chemoradiation to 26 patients. Genotyping and detection of human papillomavirus (HPV) was available for 52 patients.
Results
Using pathologic analysis, RPLN metastasis was confirmed in 22 subjects. The patients with RPLN metastasis had a significantly lower disease-specific survival rate than the non-RPLN metastasis group (54.5 vs 75 %; p = 0.05). The pN+ (RPLN) yield of these cases was 18/22 (81.8 %) for cN+ (RPLN) versus 4/32 (7.4 %) for cN0 (RPLN). Multivariate analysis identified the independent factors associated with RPLN metastasis as radiographically positive retropharyngeal node (p = 0.012; odds ratio [OR] 53.920) and posterior pharyngeal wall invasion (p = 0.021; OR 33.014). A high-risk HPV-positive result was not significantly correlated with RPLN metastasis.
Conclusions
Elective RPLN dissection should be considered for patients with advanced neck and primary tumor, particularly those with posterior pharyngeal wall invasion.
Similar content being viewed by others
References
Coskun HH, Ferlito A, Medina JE, et al. Retropharyngeal lymph node metastases in head and neck malignancies. Head Neck. 2011;33:1520–9.
Chung EJ, Oh JI, Choi KY, Lee DJ, Park IS, Kim JH, Rho YS. Pattern of cervical lymph node metastasis in tonsil cancer: predictive factor analysis of contralateral and retropharyngeal lymph node metastasis. Oral Oncol. 2011;47:758–62.
McLaughlin MP, Mendenhall WM, Mancuso AA, et al. Retropharyngeal adenopathy as a predictor of outcome in squamous cell carcinoma of the head and neck. Head Neck. 1995;17:190–8.
Amatsu M, Mohri M, Kinishi M. Significance of retropharyngeal node dissection at radical surgery for carcinoma of the hypopharynx and cervical esophagus. Laryngoscope. 2001;111:1099–103.
Shimizu K, Inoue H, Saitoh M, et al. Distribution and impact of lymph node metastases in oropharyngeal cancer. Acta Otolaryngol. 2006;126:872–7.
Yoo SH, Son EM, Sung CO, Kim KR. Primary squamous cell carcinoma of the upper genital tract: utility of p16(INK4a) expression and HPV DNA status in its differential diagnosis from extended cervical squamous cell carcinoma. Korean J Pathol. 2013;47:549–56.
Ferlito A, Shaha AR, Rinaldo A. Retropharyngeal lymph node metastasis from cancer of the head and neck. Acta Otolaryngol. 2002;122:556–60.
Ballantyne AJ. Significance of retropharyngeal nodes in cancer of the head and neck. Am J Surg. 1964;108:500–4.
Byers RM, Wolf PF, Ballantyne AJ. Rationale for elective modified neck dissection. Head Neck Surg. 1988;10:160–7.
Hasegawa Y, Matsuura H. Retropharyngeal node dissection in cancer of the oropharynx and hypopharynx. Head Neck. 1994;16:173–80.
Dirix P, Nuyts S, Bussels B, Hermans R, Van den Bogaert W. Prognostic influence of retropharyngeal lymph node metastasis in squamous cell carcinoma of the oropharynx. Int J Radiat Oncol Biol Phys. 2006;65:739–44.
Chu HR, Kim JH, Yoon DY, Hwang HS, Rho YS. Additional diagnostic value of (18)F-FDG PET-CT in detecting retropharyngeal nodal metastases. Otolaryngol Head Neck Surg. 2009;141:633–8.
Morrissey DD, Talbot JM, Cohen JI, Wax MK, Andersen PE. Accuracy of computed tomography in determining the presence or absence of metastatic retropharyngeal adenopathy. Arch Otolaryngol Head Neck Surg. 2000;126:1478–81.
Hoffmann M, Görögh T, Gottschlich S, et al. Human papillomaviruses in head and neck cancer: 8-year survival analysis of 73 patients. Cancer Lett. 2005;218:199–206.
Smith EM, Ritchie JM, Summersgill KF, et al. Age, sexual behaviour, and human papillomavirus infection in oral cavity and oropharyngeal cancers. Int J Cancer. 2004;108:766–72.
Acknowledgment
This research was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (2014R1A1A2059344).
Disclosures
There are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chung, EJ., Kim, GW., Cho, BK. et al. Retropharyngeal Lymph Node Metastasis in 54 Patients with Oropharyngeal Squamous Cell Carcinoma Who Underwent Surgery-Based Treatment. Ann Surg Oncol 22, 3049–3054 (2015). https://doi.org/10.1245/s10434-014-4364-4
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-014-4364-4