Abstract
Background
There has been an increased use of total thyroidectomy (TT), including in the management of benign thyroid diseases. We sought to compare the risk of complications between TT and unilateral thyroidectomy (UT) and to evaluate the effect of surgeon’s experience on outcomes.
Methods
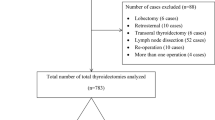
Nationwide Inpatient Sample from 2003 to 2009 was used to perform cross-sectional analysis of all adult patients who underwent TT and UT for benign or malignant conditions. Logistic regression was used to evaluate outcomes and to provide correlation between outcome and surgeon volume. Surgeon volume was categorized as low or high (performing <10 or >99 thyroid operations/year, respectively).
Results
A total of 62,722 procedures were included. Most cases were TT (57.9 %) performed for benign disease. There was a significantly increased risk of complication after TT compared to UT (20.4 vs. 10.8 %: p < 0.0001). High-volume surgeons performed only 5.0 % of the procedures overall, with 62.6 % of the high-volume surgeon procedures being TTs. Low-volume surgeons were more likely to have postoperative complications after TT compared to high-volume surgeons (odds ratio 1.53, 95 % confidence interval 1.12, 2.11, p = 0.0083). Mean charges were significantly higher for TT compared to lobectomy ($19,365 vs. $15,602, p < 0.0001), and length of stay was longer for TT compared to lobectomy (1.63 vs. 1.29 days, p < 0.0001).
Conclusions
TT is associated with a significantly higher risk of complications compared to UT even among high-volume surgeons. Higher surgeon volume is associated with improved patient outcomes.

Similar content being viewed by others
References
Dunn JT. Guarding our nation’s thyroid health. J Clin Endocrinol Metab. 2002;87:486–8.
Sosa JA, Udelsman R. Total thyroidectomy for differentiated thyroid cancer. J Surg Oncol. 2006;94:701–7.
Brown RL, de Souza JA, Cohen EE. Thyroid cancer: burden of illness and management of disease. J Cancer. 2011;2:193–9.
Spanheimer PM, Sugg SL, Lal G, Howe JR, Weigel RJ. Surveillance and intervention after thyroid lobectomy. Ann Surg Oncol. 2011;18:1729–33.
Ho TW, Shaheen AA, Dixon E, Harvey A. Utilization of thyroidectomy for benign disease in the United States: a 15-year population-based study. Am J Surg. 2011;201:570–4.
Birkmeyer JD, Siewers AE, Finlayson EV, et al. Hospital volume and surgical mortality in the United States. N Engl J Med. 2002;346:1128–37.
Birkmeyer JD, Sun Y, Wong SL, Stukel TA. Hospital volume and late survival after cancer surgery. Ann Surg. 2007;245:777–83.
Finlayson EV, Goodney PP, Birkmeyer JD. Hospital volume and operative mortality in cancer surgery: a national study. Arch Surg. 2003;138:721–6.
Cheung MC, Hamilton K, Sherman R, Byrne MM, Nguyen DM, Franceschi D, Koniaris LG. Impact of teaching facility status and high-volume centers on outcomes for lung cancer resection: an examination of 13,469 surgical patients. Ann Surg Oncol. 2009;16:3–13.
Chen H, Zeiger MA, Gordon TA, Udelsman R. Parathyroidectomy in Maryland: effects of an endocrine center. Surgery. 1996;120:948–53.
Zelen J, Bilfinger TV, Anagnostopoulos CE. Coronary artery bypass grafting: the relationship of surgical volume, hospital location, and outcome. N Y State J Med. 1991;91:290–2.
Birkmeyer JD, Stukel TA, Siewers AE, Goodney PP, Wennberg DE, Lucas FL. Surgeon volume and operative mortality in the United States. N Engl J Med. 2003;349:2117–27.
Dimick JB, Cowan JA Jr, Stanley JC, Henke PK, Pronovost PJ, Upchurch GR Jr. Surgeon specialty and provider volumes are related to outcome of intact abdominal aortic aneurysm repair in the United States. J Vasc Surg. 2003;38:739–44.
Courcoulas A, Schuchert M, Gatti G, Luketich J. The relationship of surgeon and hospital volume to outcome after gastric bypass surgery in Pennsylvania: a 3-year summary. Surgery. 2003;134:613–23.
Nguyen NT, Paya M, Stevens CM, Mavandadi S, Zainabadi K, Wilson SE. The relationship between hospital volume and outcome in bariatric surgery at academic medical centers. Ann Surg. 2004;240:586–94.
Ho V, Heslin MJ. Effect of hospital volume and experience on in-hospital mortality for pancreaticoduodenectomy. Ann Surg. 2003;237:509–14.
Sosa JA, Bowman HM, Gordon TA, et al. Importance of hospital volume in the overall management of pancreatic cancer. Ann Surg. 1998;228:429–38.
Casson AG, Van Lanschot JJ. Improving outcomes after esophagectomy: the impact of operative volume. J Surg Oncol. 2005;92:262–6.
Sosa JA, Bowman HM, Tielsch JM, Powe NR, Gordon TA, Udelsman R. The importance of surgeon experience for clinical and economic outcomes from thyroidectomy. Ann Surg. 1998;228:320–30.
Loyo M, Tufano RP, Gourin CG. National trends in thyroid surgery and the effect of volume on short-term outcomes. Laryngoscope. 2013;123:2056–63.
Gourin CG, Tufano RP, Forastiere AA, Koch WM, Pawlik TP, Bristow RE. Volume-based trends in thyroid surgery. Arch Otolaryngol Head Neck Surg. 2010;136:1191–8.
Cherenfant J, Gage M, Mangold K, et al. Trends in thyroid surgery in Illinois. Surgery. 2013;154:1016–23.
Kandil E, Noureldine SI, Abbas A, Tufano RP. The impact of surgical volume on patient outcomes following thyroid surgery. Surgery. 2013;154:1346–52.
Becker WF. Presidential address: pioneers in thyroid surgery. Ann Surg. 1977;185:493–504.
Stavrakis AI, Ituarte PH, Ko CY, Yeh MW. Surgeon volume as a predictor of outcomes in inpatient and outpatient endocrine surgery. Surgery. 2007;142:887–99.
Saunders BD, Wainess RM, Dimick JB, Doherty GM, Upchurch GR, Gauger PG. Who performs endocrine operations in the United States? Surgery. 2003;134:924–31.
Barczynski M, Konturek A, Stopa M, Cichon S, Richter P, Nowak W. Total thyroidectomy for benign thyroid: is it really worthwhile? Ann Surg. 2011;254:724–30.
Vaiman M, Nagibin A, Olevson J. Complications in primary and completed thyroidectomy. Surg Today. 2010;40:114–8.
Ozbas S, Kocak S, Aydintung S, Cakmak A, Demirkiran MA, Wishart GC. Comparison of the complications of subtotal, near total, and total thyroidectomy in the surgical management of multinodular goiter. Endocr J. 2005;52:199–205.
Wheeler MH. Total thyroidectomy for benign thyroid disease. Lancet. 1998;351:1526–7.
Koyuncu A, Dökmetas HS, Turan M, et al. Comparison of different thyroidectomy techniques for benign thyroid disease. Endocrine J. 2003;50:723–7.
American Thyroid Association (ATA) Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer; Cooper DS, Doherty GM, Haugen BR, et al. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009;19:1167–214.
HCUP Databases. Healthcare cost and utilization project. Rockville, MD: Agency for Healthcare Research and Quality; 2013. http://www.hcup-us.ahrq.gov/nisoverview.jsp. Accessed 2 Jan 2014.
Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–9.
Hay ID, Hutchinson ME, Gonzalez-Losada T, et al. Papillary thyroid microcarcinoma: a study of 900 cases observed in a 60-year period. Surgery. 2008;144:980–7.
Lin HW, Bhattacharyya N. Survival impact of treatment options for papillary microcarcinoma of the thyroid. Laryngoscope. 2009;119:1983–7.
Baudin E, Travagli JP, Ropers J, et al. Microcarcinoma of the thyroid gland: the Gustave-Roussy Institute experience. Cancer. 1998;83:553–9.
Delbridge L, Guinea AI, Reeve TS. Total thyroidectomy for bilateral benign multinodular goiter: effect of changing practice. Arch Surg. 1999;134:1389–93.
Bellantone R, Lombardi CP, Bossola M, et al. Total thyroidectomy for management of benign thyroid disease: review of 526 cases. World J Surg. 2002;26:1468–71.
Reeve TS, Curtin A, Fingleton L, et al. Can total thyroidectomy be performed as safely by general surgeons in provincial centers as by surgeons in specialized endocrine surgical units? Making the case for surgical training. Arch Surg. 1994;129:834–6.
Quan H, Li B, Saunders LD, et al. Assessing validity of ICD-9-CM and ICD-10 administrative data in recording clinical conditions in a unique dually coded database. Health Serv Res. 2008;43:1424–41.
Conflict of interest
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hauch, A., Al-Qurayshi, Z., Randolph, G. et al. Total Thyroidectomy is Associated with Increased Risk of Complications for Low- and High-Volume Surgeons. Ann Surg Oncol 21, 3844–3852 (2014). https://doi.org/10.1245/s10434-014-3846-8
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-014-3846-8