Abstract
Background
Drug-related problems (DRPs) are common in aged care facilities and few studies have been conducted to determine the impact of the pharmacist-conducted medication review services. Studies determining the prevalence of chronic kidney disease (CKD) and data regarding inappropriate prescribing of renally cleared medications in aged care facilities in Australia are also lacking.
Objectives
To investigate the number and nature of DRPs identified and recommendations made by pharmacists in residents of aged care facilities. To determine the prevalence of CKD and estimate the magnitude of inappropriate prescribing of renally cleared medications in residents of aged care facilities.
Methods
DRPs identified and recommendations made by pharmacists were classified using the adapted version of the DOCUMENT classification system. The modification of diet in renal disease formula was used to estimate the prevalence of CKD, and the Cockcroft–Gault formula was used to estimate the magnitude of inappropriate prescribing of renally cleared medications.
Results
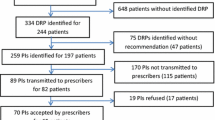
Over 98 % of residents of aged care facilities had at least one DRP. Most (83.8 %) recommendations made by accredited pharmacists to resolve DRPs were accepted by general practitioners. CKD was prevalent in 48 % of residents, and inappropriate prescribing of renally cleared medications was identified in 28 (16 %) residents with CKD.
Conclusions
DRPs are common in aged care facilities and the impact of medication review services appears to be high. CKD is also common among residents of aged care facilities, and inappropriate prescribing of renally cleared medications was also prevalent, warranting attention to regular renal function monitoring and appropriate drug and dose selection in residents of aged care facilities.

Similar content being viewed by others
References
Hamilton HJ, Gallagher PF, O’Mahony D. Inappropriate prescribing and adverse drug events in older people. BMC Geriatr. 2009;9:5. doi:10.1186/1471-2318-9-5.
Williams M, Peterson GM, Tenni PC, et al. DOCUMENT: a system for classifying drug-related problems in community pharmacy. Int J Clin Pharm. 2012;34(1):43–52. doi:10.1007/s11096-011-9583-1.
Fick DM, Cooper JW, Wade WE, et al. Updating the Beers criteria for potentially inappropriate medication use in older adults: results of a US consensus panel of experts. Arch Intern Med. 2003;163(22):2716–24. doi:10.1001/archinte.163.22.2716.
Beyth RJ, Shorr RI. Principles of drug therapy in older patients: rational drug prescribing. Clin Geriatr Med. 2002;18(3):577–92.
Walley T, Scott AK. Prescribing in the elderly. Postgrad Med J. 1995;71(838):466–71.
Mangoni AA, Jackson SH. Age-related changes in pharmacokinetics and pharmacodynamics: basic principles and practical applications. Br J Clin Pharmacol. 2004;57(1):6–14.
ElDesoky ES. Pharmacokinetic-pharmacodynamic crisis in the elderly. Am J Ther. 2007;14(5):488–98. doi:10.1097/01.mjt.0000183719.84390.4d.
Stafford AC, Alswayan MS, Tenni PC. Inappropriate prescribing in older residents of Australian care homes. J Clin Pharm Ther. 2011;36(1):33–44. doi:10.1111/j.1365-2710.2009.01151.x.
Castelino RL, Bajorek BV, Chen TF. Targeting suboptimal prescribing in the elderly: a review of the impact of pharmacy services. Ann Pharmacother. 2009;43(6):1096–106. doi:10.1345/aph.1L700.
Beers MH, Ouslander JG, Fingold SF, et al. Inappropriate medication prescribing in skilled-nursing facilities. Ann Intern Med. 1992;117(8):684–9.
Gill SS, Misiaszek BC, Brymer C. Improving prescribing in the elderly: a study in the long term care setting. Can J Clin Pharmacol. 2001;8(2):78–83.
O’Connor MN, Gallagher P, O’Mahony D. Inappropriate prescribing: criteria, detection and prevention. Drugs Aging. 2012;29(6):437–52. doi:10.2165/11632610-000000000-00000.
Ruggiero C, Dell’Aquila G, Gasperini B, et al. Potentially inappropriate drug prescriptions and risk of hospitalization among older, Italian, nursing home residents: the ULISSE project. Drugs Aging. 2010;27(9):747–58. doi:10.2165/11538240-000000000-00000.
Hanlon JT, Wang X, Handler SM, et al. Potentially inappropriate prescribing of primarily renally cleared medications for older veterans affairs nursing home patients. J Am Med Dir Assoc. 2011;12(5):377–83. doi:10.1016/j.jamda.2010.04.008.
Rahimi AR, Kennedy K, Thomason M, et al. Improper renal dosing in long-term care facilities. South Med J. 2008;101(8):802–5. doi:10.1097/SMJ.0b013e31817f1f71.
Levey AS, Coresh J, Balk E, et al. National Kidney Foundation practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Ann Intern Med. 2003;139(2):137–47.
Stevens LA, Coresh J, Greene T, et al. Assessing kidney function: measured and estimated glomerular filtration rate. N Engl J Med. 2006;354(23):2473–83. doi:10.1056/NEJMra054415.
Olyaei AJ, Steffl JL. A quantitative approach to drug dosing in chronic kidney disease. Blood Purif. 2011;31(1–3):138–45. doi:10.1159/000321857.
Coresh J, Selvin E, Stevens LA, et al. Prevalence of chronic kidney disease in the United States. JAMA. 2007;298(17):2038–47. doi:10.1001/jama.298.17.2038.
Jose MD, Otahal P, Kirkland G, et al. Chronic kidney disease in Tasmania. Nephrology (Carlton). 2009;14(8):743–9. doi:10.1111/j.1440-1797.2009.01198.x.
Rothberg MB, Kehoe ED, Courtemanche AL, et al. Recognition and management of chronic kidney disease in an elderly ambulatory population. J Gen Intern Med. 2008;23(8):1125–30. doi:10.1007/s11606-008-0607-z.
Papaioannou A, Clarke JA, Campbell G, et al. Assessment of adherence to renal dosing guidelines in long-term care facilities. J Am Geriatr Soc. 2000;48(11):1470–3.
Department of Health. Medication Management Reviews/Residential Medication Management Review. 2013. http://www.health.gov.au/internet/main/publishing.nsf/Content/medication_management_reviews.htm. Accessed 30 Sep 2013.
Nishtala PS, Hilmer SN, McLachlan AJ, et al. Impact of residential medication management reviews on drug burden index in aged-care homes: a retrospective analysis. Drugs Aging. 2009;26(8):677–86. doi:10.2165/11316440-000000000-00000.
Pharmaceutical Society of Australia. Guidelines for pharmacists providing Residential Medication Management Review (RMMR) and Quality Use of Medicines (QUM). 2011. http://www.psa.org.au/aprc-residential-medication-review/unserstand-service-information. Accessed 30 Sep 2013.
Nishtala PS, McLachlan AJ, Bell JS, et al. A retrospective study of drug-related problems in Australian aged care homes: medication reviews involving pharmacists and general practitioners. J Eval Clin Pract. 2011;17(1):97–103. doi:10.1111/j.1365-2753.2010.01374.x.
Roberts MS, Stokes JA, King MA, et al. Outcomes of a randomized controlled trial of a clinical pharmacy intervention in 52 nursing homes. Br J Clin Pharmacol. 2001;51(3):257–65.
Zermansky AG, Alldred DP, Petty DR, et al. Clinical medication review by a pharmacist of elderly people living in care homes: randomised controlled trial. Age Ageing. 2006;35(6):586–91. doi:10.1093/ageing/afl075.
WHO Collaborating Centre for Drug Statistics Mthodology. Anatomical Therapeutic Chemical (ATC) Classification System. Norweigan Institute of Public Health. http://www.whocc.no/atc_ddd_publications/atc_ddd_index/. Accessed 25 Sep 2013.
WHO. International Classification of Diseases (ICD)-10, version 2010. http://www.who.int/classifications/icd/en/. Accessed 25 Sep 2013.
Stevens LA, Nolin TD, Richardson MM, et al. Comparison of drug dosing recommendations based on measured GFR and kidney function estimating equations. Am J Kidney Dis. 2009;54(1):33–42. doi:10.1053/j.ajkd.2009.03.008.
Australian Medicines Handbook (AMH). Evidence-based independent medicines reference. 2014. https://shop.amh.net.au/. Accessed 21 July2014.
Faull R, Lee L. Prescribing in renal disease. Australian Prescriber. 2007. http://www.australianprescriber.com/magazine/30/1/17/20. Accessed 25 Sep 2013.
R Core Team (2013) R: A language for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. http://www.r-project.org/. Accessed 3 Oct 2013.
Finkers F, Maring JG, Boersma F, et al. A study of medication reviews to identify drug-related problems of polypharmacy patients in the Dutch nursing home setting. J Clin Pharm Ther. 2007;32(5):469–76. doi:10.1111/j.1365-2710.2007.00849.x.
Gurwitz JH, Field TS, Avorn J, et al. Incidence and preventability of adverse drug events in nursing homes. Am J Med. 2000;109(2):87–94.
Nguyen JK, Fouts MM, Kotabe SE, et al. Polypharmacy as a risk factor for adverse drug reactions in geriatric nursing home residents. Am J Geriatr Pharmacother. 2006;4(1):36–41. doi:10.1016/j.amjopharm.2006.03.002.
Gurwitz JH, Field TS, Judge J, et al. The incidence of adverse drug events in two large academic long-term care facilities. Am J Med. 2005;118(3):251–8. doi:10.1016/j.amjmed.2004.09.018.
Vlasses PH, Lucarotti RL, Miller DA, et al. Drug therapy review in a skilled nursing facility: an innovative approach. J Am Pharm Assoc. 1977;17(2):92–4.
Mandryk JA, Wai A, Mackson JM, et al. Evaluating the impact of educational interventions on use of antithrombotics in Australia. Pharmacoepidemiol Drug Saf. 2008;17(2):160–71. doi:10.1002/pds.1536.
Schoen C, Osborn R, Huynh PT, et al. Taking the pulse of health care systems: experiences of patients with health problems in six countries. Health Aff (Millwood). 2005;Suppl Web Exclusives:W5-509-25. doi:10.1377/hlthaff.w5.509.
Harding G, Wilcock M. Community pharmacists’ perceptions of medicines use reviews and quality assurance by peer review. Pharm World Sci. 2010;32(3):381–5. doi:10.1007/s11096-010-9381-1.
McClellan WM, Resnick B, Lei L, et al. Prevalence and severity of chronic kidney disease and anemia in the nursing home population. J Am Med Dir Assoc. 2010;11(1):33–41. doi:10.1016/j.jamda.2009.07.003.
Khanal A, Castelino RL, Peterson GM, et al. Dose adjustment guidelines for medications in patients with renal impairment: how consistent are drug information sources? Intern Med J. 2014;44(1):77–85. doi:10.1111/imj.12291.
Sweileh WM, Janem SA, Sawalha AF, et al. Medication dosing errors in hospitalized patients with renal impairment: a study in Palestine. Pharmacoepidemiol Drug Saf. 2007;16(8):908–12. doi:10.1002/pds.1412.
Decloedt E, Leisegang R, Blockman M, et al. Dosage adjustment in medical patients with renal impairment at Groote Schuur Hospital. S Afr Med J. 2010;100(5):304–6.
Khanal A, Peterson GM, Castelino RL, et al. Renal drug dosing recommendations: evaluation of product information for brands of the same drug. Intern Med J. 2014;44(6):591–6. doi:10.1111/imj.12446.
Hanlon JT, Aspinall SL, Semla TP, et al. Consensus guidelines for oral dosing of primarily renally cleared medications in older adults. J Am Geriatr Soc. 2009;57(2):335–40. doi:10.1111/j.1532-5415.2008.02098.x.
Desrochers JF, Lemieux JP, Morin-Belanger C, et al. Development and validation of the PAIR (Pharmacotherapy Assessment in Chronic Renal Disease) criteria to assess medication safety and use issues in patients with CKD. Am J Kidney Dis. 2011;58(4):527–35. doi:10.1053/j.ajkd.2011.04.020.
Acknowledgments
Pankti Gheewala, Gregory Peterson, Colin Curtain, Prasad Nishtala, Paul Hannan and Ronald Castelino have no potential conflicts of interests that are directly relevant to the content of this study. No sources of funding were used to assist in this study. Paul J. Hannan is a consultant for Meditrax Pty Ltd. The authors acknowledge Meditrax Pty Ltd and staff for providing de-identified medication reviews used in this study.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Gheewala, P.A., Peterson, G.M., Curtain, C.M. et al. Impact of the Pharmacist Medication Review Services on Drug-Related Problems and Potentially Inappropriate Prescribing of Renally Cleared Medications in Residents of Aged Care Facilities. Drugs Aging 31, 825–835 (2014). https://doi.org/10.1007/s40266-014-0208-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-014-0208-y