Abstract
Pyoderma gangrenosum (PG) is a rare inflammatory neutrophilic disorder with prototypical clinical presentations. Its pathophysiology is complex and not fully explained. Recent information regarding the genetic basis of PG and the role of auto-inflammation provides a better understanding of the disease and new therapeutic targets. PG equally affects patients of both sexes and of any age. Uncontrolled cutaneous neutrophilic inflammation is the cornerstone in a genetically predisposed individual. Multimodality management is often required to reduce inflammation, optimize wound healing, and treat underlying disease. A gold standard for the management of PG does not exist and high-level evidence is limited. Multiple factors must be taken into account when deciding on the optimum treatment for individual patients: location, number and size of lesion/ulceration(s), extracutaneous involvement, presence of associated disease, cost, and side effects of treatment, as well as patient comorbidities and preferences. Refractory and rapidly progressive cases require early initiation of systemic therapy. Newer targeted therapies represent a promising pathway for the management of PG, and the main focus of this review is the management and evidence supporting the role of new targeted therapies in PG.





Similar content being viewed by others
References
Ahronowitz I, Harp J, Shinkai K. Etiology and management of pyoderma gangrenosum: a comprehensive review. Am J Clin Dermatol. 2012;13(3):191–211.
Marzano AV, Fanoni D, Antiga E, Quaglino P, Caproni M, Crosti C, et al. Expression of cytokines, chemokines and other effector molecules in two prototypic autoinflammatory skin diseases, pyoderma gangrenosum and Sweet’s syndrome. Clin Exp Immunol. 2014;178(1):48–56.
Hafner J, Nobbe S, Partsch H, Lauchli S, Mayer D, Amann-Vesti B, et al. Martorell hypertensive ischemic leg ulcer: a model of ischemic subcutaneous arteriolosclerosis. Arch Dermatol. 2010;146(9):961–8.
Weizman A, Huang B, Targan S, Dubinsky M, Fleshner P, Kaur M, et al. Pyoderma gangrenosum among patients with inflammatory bowel disease: a descriptive cohort study. J Cutan Med Surg. 2015;19:125–31.
Shahid S, Myszor M, De Silva A. Pyoderma gangrenosum as a first presentation of inflammatory bowel disease. BMJ Case Rep. 2014;2014:pii:bcr2014204853.
Ahronowitz I, Harp J, Shinkai K. Etiology and mangement of pyoderma gangrenosum: a comprehensive review. Am J Clin Dermatol. 2012;13:191–211.
Gameiro A, Pereira N, Cardoso JC, Goncalo M. Pyoderma gangrenosum: challenges and solutions. Clin Cosmet Investig Dermatol. 2015;8:285–93.
Adachi Y, Kindzelskii AL, Cookingham G, Shaya S, Moore EC, Todd RF 3rd, et al. Aberrant neutrophil trafficking and metabolic oscillations in severe pyoderma gangrenosum. J Investig Dermatol. 1998;111:259–68.
Magro CM, Kiani B, Li J, Crowson AN. Clonality in the setting of Sweet’s syndrome and pyoderma gangrenosum is not limited to underlying myeloproliferative disease. J Cutan Pathol. 2007;34(7):526–34.
Jabbari H, Payvarmehr F, SeyedAlinaghi S, Roosta N. A case report of cyclic neutropenia associated with pyoderma gangrenosum. Acta Med Iran. 2011;49(11):763–5.
Mehta AJ, Charman CR. Pyoderma gangrenosum in association with autoimmune neutropenia of infancy. Pediatr Dermatol. 2008;25(6):620–2.
Thakur N, Sodani R, Chandra J, Singh V. Leukocyte adhesion defect type 1 presenting with recurrent pyoderma gnagrenosum. Indian J Dermatol. 2013;58:158.
Butler D, Shinkai K. What do autoinflammatory syndromes teach about common cutaneous diseases such as pyoderma gangrenosum? A commentary. Dermatol Clin. 2013;31(3):427–35.
Braswell SF, Kostopoulos TC, Ortega-Loayza AG. Pathophysiology of pyoderma gangrenosum (PG): an updated review. J Am Acad Dermatol. 2015;73(4):691–8.
Steele RB, Nugent WH, Braswell SF, Frisch S, Ferrell J, Ortega-Loayza AG. Pyoderma gangrenosum and pregnancy: an example of abnormal inflammation and challenging treatment. Br J Dermatol. 2016;174(1):77–87.
Palanivel JA, Macbeth AE, Levell NJ. Pyoderma gangrenosum in association with Janus kinase 2 (JAK2V617F) mutation. Clin Exp Dermatol. 2013;38(1):44–6.
Marzano AV, Trevisan V, Gattorno M, Ceccherini I, De Simone C, Crosti C. Pyogenic arthritis, pyoderma gangrenosum, acne, and hidradenitis suppurativa (PAPASH): a new autoinflammatory syndrome associated with a novel mutation of the PSTPIP1 gene. JAMA Dermatol. 2013;149(6):762–4.
Marzano AV, Borghi A, Meroni PL, Cugno M. Pyoderma gangrenosum and its syndromic forms: Evidence for a link with autoinflammation. Br J Dermatol. 2016;175(5):882–91.
Marzano AV, Cugno M, Trevisan V, Fanoni D, Venegoni L, Berti E, et al. Role of inflammatory cells, cytokines and matrix metalloproteinases in neutrophil-mediated skin diseases. Clin Exp Immunol. 2010;162(1):100–7.
Caproni M, Antiga E, Volpi W, Verdelli A, Venegoni L, Quaglino P, et al. The Tre.Th 17 cell ratio is reduced in the skin lesions of patients with pyoderma gangrenosum. Br J Dermatol. 2015;173:275–8.
Quaglino P, Fava P, Caproni M, Antiga E, De Simone C, Papini M, et al. Phenotypical characterization of circulating cell subsets in pyoderma gangrenosum patients: the experience of the Italian immuno-pathology group. J Eur Acad Dermatol Venereol. 2016;30:655–8.
Marzano AV, Ceccherini I, Gattorno M, Fanoni D, Caroli F, Rusmini M, et al. Association of pyoderma gangrenosum, acne, and suppurative hidradenitis (PASH) shares genetic and cytokine profiles with other autoimflammatory diseases. Medicine (Baltimore). 2014;93(27):e187.
Marzano AV, Fanoni D, Antiga E, Quaglino P, Caproni M, Crosti C, et al. Expression of cytokines, chemokines and other effector molecules in two prototypic autoinflammatory skin diseases, pyoderma gangrenosum and Sweet’s syndrome. Clin Exp Immunol. 2014;178:48–56.
Guenova E, Teske A, Fehrenbacher B, Hoerber S, Adamczyk A, Schaller M, et al. Interleukin 23 expression in pyoderma gangrenosum and targeted therapy with ustekinumab. Arch Dermatol. 2011;147:1203–5.
Hideki M, Tetsurou T, Sakae F, Kensei K, Makoto O, Toshinobu K. Idiopathic myelofibrosis and pyoderma gangrenosum involving a mutation of Janus kinase 2 (JAK2V617F), showing poor prognosis. Eur J Dermatol. 2013;23(2):256–7.
Sandhu K, Handa S, Kanwar AJ. Idiopathic pyoderma gangrenosum in a child. Pediatr Dermatol. 2004;21(3):276–7.
Wu BC, Patel ED, Ortega-Loayza AG. Drug-induced pyoderma gangrenosum: a model to understand the pathogenesis of pyoderma gangrenosum. Br J Dermatol. 2016 (Epub 19 Nov 2016).
Patel F, Fitzmaurice S, Duong C, He Y, Fergus J, Raychaudhuri SP, et al. Effectice strategies for the management of pyoderma gangrenosum:a comprehensive review. Acta Derm Venereol. 2015;95:525–31.
Wallach D, Vignon-Pennamen MD. Pyoderma gangrenosum and Sweet syndrome: the prototypic neutrophilic dermatoses. Br J Dermatol. 2015 (Epub 22 Jul 2015).
Hughes AP, Jackson JM, Callen JP. Clinical features and treatment of peristomal pyoderma gangrenosum. JAMA. 2000;284(12):1546–8.
Zuo KJ, Fung E, Tredget EE, Lin A. A systemic review of post-surgical pyoderma gangrenosum:identification of risk factors and proposed management strategy. J Plast Reconstr Aesthet Surg. 2015;68:295–303.
Tolkachjov SN, Fahy AS, Wetter DA, Brough KR, Bridges AG, Davis MD, et al. Postoperative pyoderma gangrenosum (PG): the Mayo Clinic experience of 20 years from 1994 through 2014. J Am Acad Dermatol. 2015;73:615–22.
Ducic I, Odell P, Corsten M. Postoperative Meleney’s ulcer. J Otolaryngol. 1998;27:97–9.
Pinato DJ, Sharma R. Imatinib induced pyoderma gangrenosum. J Postgrad Med. 2013;59(3):244–5.
Bennett MH, Jackson JM, Jorizzo JL, Fleischer AB Jr, White WL, Callen JP. Pyoderma Gangrenosum. A comparison of typical and atypical forms with an emphasis on time to remission. Case review of 86 patients from 2 institutions. Medicine (Baltimore). 2000;79(37–46).
Bhatti H, Khalid N, Rao B. Superficial pyoderma gangrenosum treated with infliximab: a case report. Cutis. 2012;90(6):297–9.
DeFilippis EM, Feldman SR, Huang B. The genetics of pyoderma gangrenosum an implications for treatment: a systemic review. Br J Dermatol. 2015;172:1487–97.
Binus AM, Qureshi AA, Li V, Winterfield LS. Pyoderma gangrenosum: a retrospective review of patients characteristics, cormorbidities and therapy in 103 patients. Br J Dermatol. 2011;165:1244–50.
Card TR, Langan SM, Chu TP. Extra-gastrointestinal manifestations of inflammatory bowel disease may be less common than previously reported. Dig Dis Sci. 2016;61(9):2619–26.
Saracino A, Kelly R, Liew D, Chong A. Pyoderma gangrenosum requiring inpatient management: a report of 26 cases with follow up. Australas J Dermatol. 2011;52(3):218–21.
Krüger S, Piroth W, Amo Takyi B, Breuer C, Schwarz ER. Multiple aseptic pulmonary nodules with central necrosis in association with pyoderma gangrenosum. Chest. 2001;119:977–8.
Miserocchi E, Modorati G, Foster CS, Brancato R. Ocular and extracutaneous involvement in pyoderma gangrenosum. Opthalmology. 2002;109:1941–3.
Vignon-Pennamen MD. The extracutaneous involvement in the neutrophillic dermatoses. Clin Dermatol. 2000;18:339–47.
Gade M, Studstrup F, Andersen AK, Hilberg O, Fogh C, Bendstrup E. Pulmonary manifestations of pyoderma gangrenosum: 2 cases and a review of the literature. Respir Med. 2015;109(4):443–50.
Be M, Cha HJ, Park C, Park Y, Jung H, Lee Y, et al. Multiple cavitary nodules with oyoderma gangrenosum in patients with rheumatoid arthritis. Ann Transl Med. 2016;4:39.
Andrisani G, Guidi L, Papa A, Potenza AE, Cervelli D, Armuzzi A. A case of pyoderma gangrenosum with ulcerative colitis treated with combined approach: infliximab and surgery. J Crohn Colitis. 2013;7(5):421–6.
Oda F, Tohyama M, Murakami A, Kanno K, Sonobe N, Sayama K. Bromoderma mimicking pyoderma gangrenosum caused by commercial sedatives. J Dermatol. 2016;43(5):564–6.
Goodarzi H, Sivamani RK, Garcia MS, Wehrli LN, Craven H, Ono Y, et al. Effective strategies for the management of pyoderma gangrenosum. Adv Wound Care. 2012;1(5):194–9.
Klode J, Stoffels I, Korber A, Weindorf M, Dissemond J. Relationship between the seasonal onset of chronic venous leg ulcers and climatic factors. J Eur Acad Dermatol Venereol. 2011;25(12):1415–9.
Al Ghazal P, Klode J, Dissemond J. Diagnostic criteria for pyoderma gangrenosum: results of a survey among dermatologic wound experts in Germany. J Dtsch Dermatol Ges. 2014;12(12):1129–31.
Su WP, Davis M, Weenig RH, Powell FC, Perry HO. Pyoderma gangrenosum: clinicopathologic correlation and proposed diagnostic criteria. Int J Dermatol. 2004;43:790–800.
Marzano AV, Trevisan V, Lazzari R, Crosti C. Pyoderma gangrenosum: study of 21 patients and proposal of a ‘clinicotherapeutic’ classification. J Dermatolog Treat. 2011;22(5):254–60.
Tada M, Nakanishi T, Hirata C, Okano T, Sugioka Y, Wakitani S, et al. Use of infliximab in a patient with pyoderma gangrenosum and rheumatoid arthritis. Mod Rheumatol. 2010;20(6):598–601.
Wollina U. Pyoderma gangrenosum: a review. Orphanet J Rare Dis. 2007;2:19.
D’Inca R, Fagiuoli S, Sturniolo GC. Tacrolimus to treat pyoderma gangrenosum resistant to cyclosporine. Ann Intern Med. 1998;128(9):783–4.
Weizman A, Huang B, Berel D, Targan SR, Dubinsky M, Fleshner P, et al. Clinical, serologic, and genetic factors associated with pyoderma gangrenosum and erythema nodosum in inflammatory bowel disease patients. Inflamm Bowel Dis. 2014;20(3):525–33.
Weizman AV, Huang B, Targan S, Dubinsky M, Fleshner P, Kaur M, et al. Pyoderma gangrenosum among patients with inflammatory bowel disease: a descriptive cohort study. J Cutan Med Surg. 2014;18(5):361.
Sinagra E, Orlando A, Renna S, Maida M, Cottone M. Multifocal pyoderma gangrenosum resistant to infliximab in active ulcerative colitis: don’t forget the role of cyclosporin. Inflamm Bowel Dis. 2012;18(8):E1594–5.
Langan SM, Powell FC. Vegetative pyoderma gangrenosum: a report of two new cases and a review of the literature. Int J Dermatol. 2005;44(8):623–9.
Handler MZ, Hamilton H, Aires D. Treatment of peristomal pyoderma gangrenosum with topical crushed dapsone. J Drugs Dermatol. 2011;10(9):1059–61.
Chiba T, Isomura I, Suzuki A, Morita A. Topical tacrolimus therapy for pyoderma gangrenosum. J Dermatol. 2005;32(3):199–203.
Cozzani E, Gasparini G, Parodi A. Pyoderma gangrenosum: a systematic review. G Ital Dermatol Venereol. 2014;149(5):587–600.
Ambooken B, Khader A, Muhammed K, Rajan U, Snigdha O. Malignant pyoderma gangrenosum eroding the parotid gland successfully treated with dexamethasone pulse therapy. Int J Dermatol. 2014;53(12):1536–8.
Ormerod AD, Thomas KS, Craig FE, Mitchell E, Greenlaw N, Norrie J, et al. Comparison of the two most commonly used treatments for pyoderma gangrenosum: results of the STOP GAP randomised controlled trial. BMJ. 2015;350:h2958.
Reynoso-von Drateln C, Perla-Navarro AV, Gamez-Nava JI, Gonzalez-Lopez L, Galvan-Villegas F, Ramos-Remus C. Intravenous cyclophosphamide pulses in pyoderma gangrenosum: an open trial. J Rheumatol. 1997;24(4):689–93.
Wollina U. Pyoderma gangrenosum: a systemic disease? Clin Dermatol. 2015;33(5):527–30.
Wollina U, Tchernev G. Pyoderma gangrenosum: pathogenetic oriented treatment approaches. Wien Med Wochenschr. 2014;164(13–14):263–73.
Kolios AG, Maul JT, Meier B, Kerl K, Traidl-Hoffmann C, Hertl M, et al. Canakinumab in adults with steroid-refractory pyoderma gangrenosum. Br J Dermatol. 2015;173(5):1216–23.
Caproni M, Antiga E, Volpi W, Verdelli A, Venegoni L, Quaglino P, et al. The Treg/Th17 cell ratio is reduced in the skin lesions of patients with pyoderma gangrenosum. Br J Dermatol. 2015;173(1):275–8.
Campanati A, Brisigotti V, Ganzetti G, Molinelli E, Giuliodori K, Consales V, et al. Finally, recurrent pyoderma gangrenosum treated with adalimumab: case report and review of the literature. J Eur Acad Dermatol Venereol. 2015;29(6):1245–7.
Campanati A, Ganzetti G, Giuliodori K, Molinelli E, Offidani A. Biologic therapy in psoriasis: safety profile. Curr Drug Saf. 2016;11(1):4–11.
Brooklyn TN, Dunnill MG, Shetty A, Bowden JJ, Williams JD, Griffiths CE, et al. Infliximab for the treatment of pyoderma gangrenosum: a randomised, double blind, placebo controlled trial. Gut. 2006;55(4):505–9.
Adisen E, Oztas M, Gurer MA. Treatment of idiopathic pyoderma gangrenosum with infliximab: induction dosing regimen or on-demand therapy? Dermatology. 2008;216(2):163–5.
Fonder MA, Cummins DL, Ehst BD, Anhalt GJ, Meyerle JH. Adalimumab therapy for recalcitrant pyoderma gangrenosum. J Burns Wounds. 2006;5:e8.
Chan JL, Graves MS, Cockerell CJ, Pandya AG. Rapid improvement of pyoderma gangrenosum after treatment with infliximab. J Drugs Dermatol. 2010;9(6):702–4.
Campos-Munoz L, Conde-Taboada A, Aleo E, Toledano E, Lopez-Bran E. Refractory pyoderma gangrenosum treated with infliximab in an infant. Clin Exp Dermatol. 2014;39(3):336–9.
Marzano AV, Tourlaki A, Alessi E, Caputo R. Widespread idiopathic pyoderma gangrenosum evolved from ulcerative to vegetative type: a 10-year history with a recent response to infliximab. Clin Exp Dermatol. 2008;33(2):156–9.
Zold E, Nagy A, Devenyi K, Zeher M, Barta Z. Successful use of adalimumab for treating fistulizing Crohn’s disease with pyoderma gangrenosum: two birds with one stone. World J Gastroenterol. 2009;15(18):2293–5.
Smith DJ Jr. Use of biobrane in wound management. J Burn Care Rehabil. 1995;16(3 Pt 1):317–20.
Heffernan MP, Anadkat MJ, Smith DI. Adalimumab treatment for pyoderma gangrenosum. Arch Dermatol. 2007;143(3):306–8.
Pomerantz RG, Husni ME, Mody E, Qureshi AA. Adalimumab for treatment of pyoderma gangrenosum. Br J Dermatol. 2007;157(6):1274–5.
Hubbard VG, Friedmann AC, Goldsmith P. Systemic pyoderma gangrenosum responding to infliximab and adalimumab. Br J Dermatol. 2005;152(5):1059–61.
Saraceno R, Babino G, Chiricozzi A, Zangrilli A, Chimenti S. PsAPASH: a new syndrome associated with hidradenitis suppurativa with response to tumor necrosis factor inhibition. J Am Acad Dermatol. 2015;72(1):e42–4.
Sagami S, Ueno Y, Tanaka S, Nagai K, Hayashi R, Chayama K. Successful use of adalimumab for treating pyoderma gangrenosum with ulcerative colitis under corticosteroid-tapering conditions. Intern Med. 2015;54(17):2167–72.
Reddick CL, Singh MN, Chalmers RJ. Successful treatment of superficial pyoderma gangrenosum associated with hidradenitis suppurativa with adalimumab. Dermatol Online J. 2010;16(8):15.
McGowan JW, Johnson CA, Lynn A. Treatment of pyoderma gangrenosum with etanercept. J Drugs Dermatol. 2004;3(4):441–4.
Reguiai Z, Grange F. The role of anti-tumor necrosis factor-alpha therapy in pyoderma gangrenosum associated with inflammatory bowel disease. Am J Clin Dermatol. 2007;8(2):67–77.
Kim FS, Pandya AG. The use of etanercept in the treatment of peristomal pyoderma gangrenosum. Clin Exp Dermatol. 2012;37(4):442–3.
Charles CA, Leon A, Banta MR, Kirsner RS. Etanercept for the treatment of refractory pyoderma gangrenosum: a brief series. Int J Dermatol. 2007;46(10):1095–9.
Pastor N, Betlloch I, Pascual JC, Blanes M, Banuls J, Silvestre JF. Pyoderma gangrenosum treated with anti-TNF alpha therapy (etanercept). Clin Exp Dermatol. 2006;31(1):152–3.
Roy DB, Conte ET, Cohen DJ. The treatment of pyoderma gangrenosum using etanercept. J Am Acad Dermatol. 2006;54(3 Suppl 2):S128–34.
Goldenberg G, Jorizzo JL. Use of etanercept in treatment of pyoderma gangrenosum in a patient with autoimmune hepatitis. J Dermatol Treat. 2005;16(5–6):347–9.
Rogge FJ, Pacifico M, Kang N. Treatment of pyoderma gangrenosum with the anti-TNFalpha drug—etanercept. J Plast Reconstr Aesthet Surg. 2008;61(4):431–3.
Disla E, Quayum B, Cuppari GG, Pancorbo R. Successful use of etanercept in a patient with pyoderma gangrenosum complicating rheumatoid arthritis. J Clin Rheumatol. 2004;10(1):50–2.
Fahmy M, Ramamoorthy S, Hata T, Sandborn WJ. Ustekinumab for peristomal pyoderma gangrenosum. Am J Gastroenterol. 2012;107(5):794–5.
Goldminz AM, Botto NC, Gottlieb AB. Severely recalcitrant pyoderma gangrenosum successfully treated with ustekinumab. J Am Acad Dermatol. 2012;67(5):e237–8.
Dinarello CA, van der Meer JW. Treating inflammation by blocking interleukin-1 in humans. Semin Immunol. 2013;25(6):469–84.
Geusau A, Mothes-Luksch N, Nahavandi H, Pickl WF, Wise CA, Pourpak Z, et al. Identification of a homozygous PSTPIP1 mutation in a patient with a PAPA-like syndrome responding to canakinumab treatment. JAMA Dermatol. 2013;149(2):209–15.
Acquitter M, Plantin P, Kupfer I, Auvinet H, Marhadour T. Anakinra improves pyoderma gangrenosum in psoriatic arthritis: a case report. Ann Intern Med. 2015;163(1):70–1.
Brenner M, Ruzicka T, Plewig G, Thomas P, Herzer P. Targeted treatment of pyoderma gangrenosum in PAPA (pyogenic arthritis, pyoderma gangrenosum and acne) syndrome with the recombinant human interleukin-1 receptor antagonist anakinra. Br J Dermatol. 2009;161(5):1199–201.
Lin Z, Hegarty JP, Lin T, Ostrov B, Wang Y, Yu W, et al. Failure of anakinra treatment of pyoderma gangrenosum in an IBD patient and relevance to the PSTPIP1 gene. Inflamm Bowel Dis. 2011;17(6):E41–2.
Lipsker D, Lenormand C. Indications and modes of use for interleukin (IL)-1 antagonists in inflammatory dermatosis: a new therapeutic approach to immune-mediated inflammatory diseases [in French]. Ann Dermatol Venereol. 2012;139(6–7):459–67.
Patel F, Fitzmaurice S, Duong C, He Y, Fergus J, Raychaudhuri SP, et al. Effective strategies for the management of pyoderma gangrenosum: a comprehensive review. Acta Derm Venereol. 2015;95(5):525–31.
Mansouri B, Richards L, Menter A. Treatment of two patients with generalized pustular psoriasis with the interleukin-1beta inhibitor gevokizumab. Br J Dermatol. 2015;173(1):239–41.
Demidowich AP, Freeman AF, Kuhns DB, Aksentijevich I, Gallin JI, Turner ML, et al. Brief report: genotype, phenotype, and clinical course in five patients with PAPA syndrome (pyogenic sterile arthritis, pyoderma gangrenosum, and acne). Arthritis Rheum. 2012;64(6):2022–7.
Ter Haar N, Lachmann H, Ozen S, Woo P, Uziel Y, Modesto C, et al. Treatment of autoinflammatory diseases: results from the Eurofever Registry and a literature review. Ann Rheum Dis. 2013;72(5):678–85.
Lindor NM, Arsenault TM, Solomon H, Seidman CE, McEvoy MT. A new autosomal dominant disorder of pyogenic sterile arthritis, pyoderma gangrenosum, and acne: PAPA syndrome. Mayo Clin Proc. 1997;72(7):611–5.
Yeon HB, Lindor NM, Seidman JG, Seidman CE. Pyogenic arthritis, pyoderma gangrenosum, and acne syndrome maps to chromosome 15q. Am J Hum Genet. 2000;66(4):1443–8.
Wise CA, Gillum JD, Seidman CE, Lindor NM, Veile R, Bashiardes S, et al. Mutations in CD2BP1 disrupt binding to PTP PEST and are responsible for PAPA syndrome, an autoinflammatory disorder. Hum Mol Genet. 2002;11(8):961–9.
Braun-Falco M, Kovnerystyy O, Lohse P, Ruzicka T. Pyoderma gangrenosum, acne, and suppurative hidradenitis (PASH): a new autoinflammatory syndrome distinct from PAPA syndrome. J Am Acad Dermatol. 2012;66(3):409–15.
Calderon-Castrat X, Bancalari-Diaz D, Roman-Curto C, Romo-Melgar A, Amoros-Cerdan D, Alcaraz-Mas LA, et al. PSTPIP1 gene mutation in a pyoderma gangrenosum, acne and suppurative hidradenitis (PASH) syndrome. Br J Dermatol. 2016;175(1):194–8.
Staub J, Pfannschmidt N, Strohal R, Braun-Falco M, Lohse P, Goerdt S, et al. Successful treatment of PASH syndrome with infliximab, cyclosporine and dapsone. J Eur Acad Dermatol Venereol. 2015;29(11):2243–7.
Contassot E, Beer HD, French LE. Interleukin-1, inflammasomes, autoinflammation and the skin. Swiss Med Wkly. 2012;142:w13590.
Leuenberger M, Berner J, Di Lucca J, Fischer L, Kaparos N, Conrad C, et al. PASS Syndrome: an IL-1-driven autoinflammatory disease. Dermatology. 2016;232(2):254–8.
Heymann MC, Rosen-Wolff A. Contribution of the inflammasomes to autoinflammatory diseases and recent mouse models as research tools. Clin Immunol. 2013;147(3):175–84.
Garzorz N, Papanagiotou V, Atenhan A, Andres C, Eyerich S, Eyerich K, et al. Pyoderma gangrenosum, acne, psoriasis, arthritis and suppurative hidradenitis (PAPASH)-syndrome: a new entity within the spectrum of autoinflammatory syndromes? J Eur Acad Dermatol Venereol. 2016;30(1):141–3.
Gungor K, Gonen S, Kisakol G, Dikbas O, Kaya A. ANCA positive propylthiouracil induced pyoderma gangrenosum. J Endocrinol Invest. 2006;29(6):575–6.
Boulenger-Vazel A, Kupfer-Bessaguet I, Gouedard C, Leberre R, Leroy JP, Sonnet E, et al. Neutrophilic dermatosis associated with propylthiouracil-induced p-ANCA (p-antineutrophil cytoplasmic antibodies) [in French]. Ann Dermatol Venereol. 2005;132(1):27–31.
Hong SB, Lee MH. A case of propylthiouracil-induced pyoderma gangrenosum associated with antineutrophil cytoplasmic antibody. Dermatology. 2004;208(4):339–41.
Darben T, Savige J, Prentice R, Paspaliaris B, Chick J. Pyoderma gangrenosum with secondary pyarthrosis following propylthiouracil. Australas J Dermatol. 1999;40(3):144–6.
Gangaram HB, Tan LP, Gan AT, Suraiya HH, Ganesapillai T. Pyoderma gangrenosum following treatment with isotretinoin. Br J Dermatol. 1997;136(4):636–7.
Hughes BR, Cunliffe WJ. Development of folliculitis and pyoderma gangrenosum in association with abdominal pain in a patient following treatment with isotretinoin. Br J Dermatol. 1990;122(5):683–7.
Levy JM, Richler D, Mahmood MN, Brassard A. Pyoderma gangrenosum associated with alitretinoin therapy. JAAD Case Rep. 2016;2(2):135–7.
Kikuchi N, Hiraiwa T, Ohashi T, Hanami Y, Satoh M, Takenoshita H, et al. Pyoderma gangrenosum possibly triggered by adalimumab. Eur J Dermatol. 2012;22(6):804–5.
Vestita M, Guida S, Mazzoccoli S, Loconsole F, Foti C. Late paradoxical development of pyoderma gangrenosum in a psoriasis patient treated with infliximab. Eur J Dermatol. 2015;25(3):272–3.
Dixit S, Selva-Nayagam P, Hamann I, Fischer G. Vulvovaginal pyoderma gangrenosum secondary to rituximab therapy. J Low Genit Tract Dis. 2015;19(1):e6–9.
Sagara R, Kitami A, Nakada T, Iijima M. Adverse reactions to gefitinib (Iressa): revealing sycosis- and pyoderma gangrenosum-like lesions. Int J Dermatol. 2006;45(8):1002–3.
Akanay-Diesel S, Hoff NP, Kurle S, Haes J, Erhardt A, Haussinger D, et al. Sunitinib induced pyoderma gangrenosum-like ulcerations. Eur J Med Res. 2011;16(11):491–4.
Nadauld LD, Miller MB, Srinivas S. Pyoderma gangrenosum with the use of sunitinib. J Clin Oncol. 2011;29(10):e266–7.
Dean SM, Zirwas M. A second case of sunitinib-associated pyoderma gangrenosum. J Clin Aesthet Dermatol. 2010;3(8):34–5.
ten Freyhaus K, Homey B, Bieber T, Wilsmann-Theis D. Pyoderma gangrenosum: another cutaneous side-effect of sunitinib? Br J Dermatol. 2008;159(1):242–3.
Miall FM, Harman K, Kennedy B, Dyer MJ. Pyoderma gangrenosum complicating pegylated granulocyte colony-stimulating factor in Hodgkin lymphoma. Br J Haematol. 2006;132(1):115–6.
White LE, Villa MT, Petronic-Rosic V, Jiang J, Medenica MM. Pyoderma gangrenosum related to a new granulocyte colony-stimulating factor. Skinmed. 2006;5(2):96–8.
Merkel PA. Drugs associated with vasculitis. Curr Opin Rheumatol. 1998;10(1):45–50.
Glass AT, Bancila E, Milgraum S. Pyoderma gangrenosum in infancy: the youngest reported patient. J Am Acad Dermatol. 1991;25(1 Pt 1):109–10.
Johnson ML, Grimwood RE. Leukocyte colony-stimulating factors. A review of associated neutrophilic dermatoses and vasculitides. Arch Dermatol. 1994;130(1):77–81.
Keith PJ, Joyce JC, Wilson BD. Pyoderma gangrenosum: a possible cutaneous complication of levamisole-tainted cocaine abuse. Int J Dermatol. 2015;54(9):1075–7.
Tseng E, Alhusayen R, Sade S, Buckstein R, Prica A. Pyoderma gangrenosum secondary to azacitidine in myelodysplastic syndrome. Br J Haematol. 2015;169(4):461.
Matthews AG, Wylie G. Hydroxycarbamide-induced cutaneous ulceration with a difference. Br J Dermatol. 2014;171(6):1572–4.
Huang W, Nath R, Zayed H, Rubin P, Moore A, Snyder R, et al. Results of an open-label, proof of concept study of gevokizumab in the treatment of the acute, inflammatory phase of pyoderma gangrenosum. Available at: http://www.xoma.com/content/pipeline/documents/X052170_AAD2014_Poster_FINAL.pdf.
Zampeli VA, Lippert U, Nikolakis G, Makrantonaki E, Tzellos TG, Krause U, et al. Disseminated refractory pyoderma gangraenosum during an ulcerative colitis flare. Treatment with infliximab. J Dermatol Case Rep. 2015;9:62–6.
Akhras V, Sarkany R, Walsh S, Hyde N, Marsden RA. Superficial granulomatous pyoderma treated preoperatively with infliximab. Clin Exp Dermatol. 2009;34:e183-5.
Ferkolj I, Hocevar A, Golouh R, Dolenc Voljc M. Infliximab for treatment of resistant pyoderma gangrenosum associated with Crohn's disease. Acta Dermatovenerol Alp Pannonica Adriat. 2006;15:173-7.
Stichweh DS, Punaro M, Pascual V. Dramatic improvement of pyoderma gangrenosum with infliximab in a patient with PAPA syndrome. Pediatr Dermatol. 2005;22:262-5.
Swale VJ, Saha M, Kapur N, Hoffbrand AV, Rustin MH. Pyoderma gangrenosum outside the context of inflammatory bowel disease treated successfully with infliximab. Clin Exp Dermatol. 2005;30:134-6.
Mimouni D, Anhalt GJ, Kouba DJ, Nousari HC. Infliximab for peristomal pyoderma gangrenosum. Br J Dermatol. 2003;148:813-6.
Batres LA, Mamula P, Baldassano RN. Resolution of severe peristomal pyoderma gangrenosum with infliximab in a child with Crohn disease. J Pediatr Gastroenterol Nutr. 2002;34:558-60.
Grange F, Djilali-Bouzina F, Weiss AM, Polette A, Guillaume JC. Corticosteroid-resistant pyoderma gangrenosum associated with Crohn's disease: rapid cure with infliximab. Dermatol. 2002;205:278-80.
Triantafillidis JK, Cheracakis P, Sklavaina M, Apostolopoulou K. Favorable response to infliximab treatment in a patient with active Crohn disease and pyoderma gangrenosum. Scand J Gastroenterol. 2002;37:863-5.
Ljung T, Staun M, Grove O, Fausa O, Vatn MH, Hellstrom PM. Pyoderma gangrenosum associated with crohn disease: effect of TNF-alpha blockade with infliximab. Scand J Gastroenterol. 2002;37:1108-10.
Arguelles-Arias F, Castro-Laria L, Lobaton T, Aguas-Peris M, Rojas-Feria M, Barreiro-de Acosta M et al. Characteristics and treatment of pyoderma gangrenosum in inflammatory bowel disease. Dig Dis Sci. 2013;58:2949-54.
Regueiro M, Valentine J, Plevy S, Fleisher MR, Lichtenstein GR. Infliximab for treatment of pyoderma gangrenosum associated with inflammatory bowel disease. Amer J Gastroenterol. 2003;98:1821-6.
Hinterberger L, Muller CS, Vogt T, Pfohler C. Adalimumab: a treatment option for pyoderma gangrenosum after failure of systemic standard therapies. Dermatol Ther. 2012;2:6.
Kleinpenning MM, Langewouters AM, Van De Kerkhof PC, Greebe RJ. Severe pyoderma gangrenosum unresponsive to etanercept and adalimumab. J Dermatol Treat. 2011;22:261-5.
Disla E, Quayum B, Cuppari GG, Pancorbo R. Successful use of etanercept in a patient with pyoderma gangrenosum complicating rheumatoid arthritis. J Clin Rheumatol. 2004;10:50-2.
Vandevyvere K, Luyten FP, Verschueren P, Lories R, Segaert S, Westhovens R. Pyoderma gangrenosum developing during therapy with TNF-alpha antagonists in a patient with rheumatoid arthritis. Clin Rheumatol. 2007;26:2205–2206.
Acknowledgements
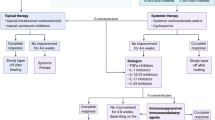
The authors would like to thank Delaram Farzanfar for her work on the tables and figures in this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for the preparation of this review and the paper has not been presented elsewhere.
Conflict of interest
Afsaneh Alavi has been a consultant and investigator for Abbvie, Galderma, Janssen, Novartis, Regeneron, Valeant, and Xoma, and received a grant from Abbvie; Lars E. French received study funding from Novartis; Alain Brassard has been a consultant and speaker for AbbVie, Janssen, Celgene, 3M, and Coloplast; and Robert S. Kirsner has been a consultant for Abbvie. Mark Davis has no conflicts of interest to declare.
Rights and permissions
About this article
Cite this article
Alavi, A., French, L.E., Davis, M.D. et al. Pyoderma Gangrenosum: An Update on Pathophysiology, Diagnosis and Treatment. Am J Clin Dermatol 18, 355–372 (2017). https://doi.org/10.1007/s40257-017-0251-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40257-017-0251-7