Abstract
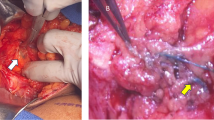
Lymphatic microsurgical preventing healing approach (LYMPHA) for prevention of breast cancer-related lymphedema (BCRL)—a preliminary report BCRL—is a chronic debilitating condition which impairs quality of life of breast cancer survivors. The aim is to study the feasibility of preventing lymphedema by performing “Lymphatic Microsurgical Preventive Healing Approach (LYMPHA).” Patients undergoing breast cancer surgery with complete nodal dissection were taken up for the study. After the standard axillary nodal dissection, lymphatics were identified by the help of blue dye and were anastomosed with a tributary to the axillary vein. Post-operatively, patients were followed up clinically for development of lymphedema and lymphoscintigraphy was performed after treatment completion. A total of 35 patients were enrolled for the study. The average BMI was 29.5. LYMPHA was feasible in all cases. The number of lymphatics identified was 1 to 5 per axilla. Two patients developed transient lymphedema which resolved with conservative therapy and patients were able to discontinue the compression garment. Follow-up lymphoscintigraphy is performed in two patients, which showed normal lymphatic flow. LYMPHA is a feasible technique, not difficult to perform, takes a short time, is accomplished in same general anesthesia as for axillary dissection, and gives no extra scar. The early results are promising and long-term follow-up may make the procedure as a routine.



Similar content being viewed by others
References
Siegel R, DeSantis C, Virgo K, Stein K, Mariotto A, Smith T, Cooper D, Gansler T, Lerro C, Fedewa S, Lin C, Leach C, Cannady RS, Cho H, Scoppa S, Hachey M, Kirch R, Jemal A, Ward E (2012) Cancer treatment and survivorship statistics, 2012. CA Cancer J Clin 62(4):220–241. https://doi.org/10.3322/caac.21149
Armer JM, Stewart BR (2010) Post-breast cancer lymphedema: incidence increases from 12 to 30 to 60 months. Lymphology 43(3):118–127
Kim M, Kim SW, Lee SU, Lee NK, Jung SY, Kim TH, Lee ES, Kang HS, Shin KH (2013) A model to estimate the risk of breast cancer-related lymphedema: combinations of treatment-related factors of the number of dissected axillary nodes, adjuvant chemotherapy, and radiation therapy. Int J Radiat Oncol Biol Phys 86(3):498–503. https://doi.org/10.1016/j.ijrobp.2013.02.018
DiSipio T, Rye S, Newman B, Hayes S (2013) Incidence of unilateral arm lymphoedema after breast cancer: a systematic review and meta-analysis. Lancet Oncol 14(6):500–515. https://doi.org/10.1016/S1470-2045(13)70076-7
Boccardo F, Casabona F, De Cian F, Friedman D, Villa G, Bogliolo S, Ferrero S, Murelli F, Campisi C (2009) Lymphedema microsurgical preventive healing approach: a new technique for primary prevention of arm lymphedema after mastectomy. Ann Surg Oncol 16(3):703–708. https://doi.org/10.1245/s10434-008-0270-y
Boccardo FM, Casabona F, Friedman D, Puglisi M, De Cian F, Ansaldi F, Campisi C (2011 Sep) Surgical prevention of arm lymphedema after breast cancer treatment. Ann Surg Oncol 18(9):2500–2505. https://doi.org/10.1245/s10434-011-1624-4
Campis CC, Ryan M, Boccardo F, Campis C (2016) A single-site technique of multiple lymphatic–venous anastomoses for the treatment of peripheral lymphedema: long-term clinical outcome. J Reconstr Microsurg 32:42–49
Petrek JA, Senie RT, Peters M, Rosen PP (2001) Lymphedema in a cohort of breast carcinoma survivors 20 years after diagnosis. Cancer 92(6):1368–1377. https://doi.org/10.1002/1097-0142(20010915)92:6<1368::AID-CNCR1459>3.0.CO;2-9
Tsai RJ, Dennis LK, Lynch CF, Snetselaar LG, Zamba GK, Scott-Conner C (2009) The risk of developing arm lymphedema among breast cancer survivors: a meta-analysis of treatment factors. Ann Surg Oncol 16(7):1959–1972. https://doi.org/10.1245/s10434-009-0452-2
Kim M, Shin KH, Jung SY, Lee S, Kang HS, Lee ES (2016) Identification of prognostic risk factors for transient and persistent lymphedema after multimodal treatment for breast cancer. Cancer Res Treat 48(4):1330–1337. https://doi.org/10.4143/crt.2015.463
Tobin MB, Lacey HJ, Meyer L, Mortimer PS (1993) The psychological morbidity of breast cancer-related arm swelling: psychological morbidity of lymphoedema. Cancer 72(11):3248–3252. https://doi.org/10.1002/1097-0142(19931201)72:11<3248::AID-CNCR2820721119>3.0.CO;2-Z
Hidding JT, Beurskens CH, van der Wees PJ, van Laarhoven HW, Nijhuis-van der Sanden MW (2014) Treatment related impairments in arm and shoulder in patients with breast cancer: a systematic review. PLoS One 9(5):e96748
Dupuy A, Benchikhi H, Roujeau JC, Bernard P, Vaillant L, Chosidow O, Sassolas B, Guillaume JC, Grob JJ, Bastuji-Garin S (1999) Risk factors for erysipelas of the leg (cellulitis): case-control study. BMJ 318(7198):1591–1594. https://doi.org/10.1136/bmj.318.7198.1591
Jørgensen MG, Toyserkani NM, Sørensen JA (2017 Mar 28) The effect of prophylactic lymphovenous anastomosis and shunts for preventing cancer-related lymphedema: a systematic review and meta-analysis. Microsurgery. https://doi.org/10.1002/micr.30180. [Epub ahead of print]
Boccardo F, Casabona F, De Cian F, Friedman D, Murelli F, Puglisi M, et al. Lymphatic microsurgical preventing healing approach (LYMPHA) for primary surgical prevention of breast cancer-related lymphedema: over 4 years follow-up. Microsurgery 2014;34(6):421–4, 424, DOI: https://doi.org/10.1002/micr.22254
Feldman S, Bansil H, Ascherman J, Grant R, Borden B, Henderson P, Ojo A, Taback B, Chen M, Ananthakrishnan P, Vaz A, Balci F, Divgi CR, Leung D, Rohde C (2015) Single institution experience with lymphatic microsurgical preventive healing approach (LYMPHA) for the primary prevention of lymphedema. Ann Surg Oncol 22(10):3296–3301. https://doi.org/10.1245/s10434-015-4721-y
Acknowledgements
The authors would like to thank Ms. Shalini Pandey for helping with data compilation for the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The authors declare that they have no conflict of interest.
Additional information
This study reports about feasibility of preventive microsurgical lymphovenous anastomosis in the axilla at the time of axillary dissection for breast cancer. The early results of this procedure are encouraging.
Electronic Supplementary Material
Rights and permissions
About this article
Cite this article
Agrawal, J., Mehta, S., Goel, A. et al. Lymphatic Microsurgical Preventing Healing Approach (LYMPHA) for Prevention of Breast Cancer-Related Lymphedema—a Preliminary Report. Indian J Surg Oncol 9, 369–373 (2018). https://doi.org/10.1007/s13193-018-0731-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13193-018-0731-0