Abstract
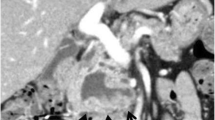
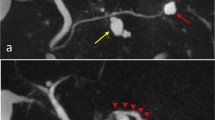
The patient was a 74-year-old female. Screening computed tomography for examination of the abdomen showed a cystic mass in the pancreatic body. Close investigation using endoscopic retrograde cholangiopancreatography and magnetic resonance cholangiopancreatography revealed a very rare finding: the main pancreatic duct bifurcated at the pancreatic body, and these two ducts converged at the caudal side. A multilocular cystic mass in the pancreatic body and mucus discharge from the orifice of major papilla were observed. There was no protruded lesion in the main pancreatic duct. No findings suggested apparent malignancy. The patient was diagnosed as having hyperplastic intraductal papillary mucinous neoplasm of branch type showing a ring-shaped pancreatic duct, and was placed under follow-up.





Similar content being viewed by others
References
Langman J. Medical embryology, vol 4. Baltimore: Williams &Wilkins; 1981.
Gore RM, Levine MS, Lanfer I. Text book of gastrointestinal radiology, vol. 2. Philadelphia: WB Saunders Company; 1994.
Bret PM, Reinhold C, Taurel P, et al. Pancreas divisum: evaluation with MR cholangiopancreatography. Radiology. 1996;199:99–103.
Parker HW. Congenital anomalies of the pancreas. In: Spivak MV, editor. Gastroenterologic-endoscopy. Philadelphia: WB Saunders; 1987. p. 770–9.
Krishnamurty VS. Bifid pancreas: an unusual anomaly associated with acute pancreatitis. Int J Pancreatol. 1994;16:179–81.
Ohhashi K, Murakami F, Takekoshi T, et al. Four cases of “mucin-producing” cancer of the pancreas on specific findings of the papilla of Vater. Proc Dig Endosc. 1982;20:348.
Maguchi H. Differential diagnosis and treatment guidelines for IPMTs and MCTs (in Japanese with English abstract). Suizo (J Jpn Panc Soc). 2003;18:673–80.
Salvia R, Castillo CF, Bassi C, et al. Main-duct intraductal papillary mucinous neoplasms of the pancreas: clinical predictors of malignancy and long-term survival following resection. Ann Surg. 2004;239:678–85.
Maguchi H. Clinicopathological and diagnostic study of mucin producing pancreatic tumors (in Japanese with English abstract). Nippon Shokakibyo Gakkai Zasshi. 1994;91:1003–15.
Maguchi H, Takahashi K, Katanuma A, Hayashi T, Yoshida A, Sakurai Y. Intraductal papillary mucinous tumor: imaging diagnosis (in Japanese with English abstract). Nippon Geka Gakkai Zasshi. 2003;104:447–52.
Sohn TA, Yeo CJ, Cameron JL, et al. Intraductal papillary mucinous neoplasms of the pancreas: an updated experience. Ann Surg. 2004;239:788–99.
Nagakawa T, Suga T, Muraoka S. Therapeutic Strategy for intraductal papillary-mucinous tumors. Clin Gastroenterol. 2006;21:219–25.
Yamaguchi K, Ohuchida J, Ohtuka T, et al. Intraductal papillary-mucinous tumor of the pancreas concomitant with ductal carcinoma of the pancreas. Pancreatology. 2002;2:484–90.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shudo, R., Maeda, S., Yoshizaki, H. et al. A rare ring-shaped anomaly of the main pancreatic duct accompanying a branch duct IPMN. Clin J Gastroenterol 2, 361–364 (2009). https://doi.org/10.1007/s12328-009-0107-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12328-009-0107-7