Abstract
Background and Purpose
Patients with acute brain injuries require strict physiologic control to minimize morbidity and mortality. This study aimed to assess in-hospital compliance to strict physiologic parameters (BP, HR, ICP, SpO2) in these populations.
Methods
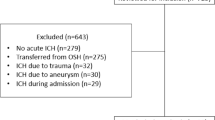
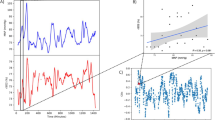
Patients with severe cerebrovascular events were admitted to the neurointensive care unit (NSICU) and were continuously monitored using the BedMasterEX (Excel Medical Electronics Inc, FL) system, which recorded hemodynamic data via an arterial catheter continuously in 5-s intervals. Furthermore, we investigated the impact of healthcare provider shift changes (6–8 a.m./p.m) and of day (6 a.m.–6 p.m.) versus night (6 p.m–6 a.m) shifts in hemodynamic control.
Results
Fifty patients admitted to the NSICU, 50 % male, mean age 59.7 ± 13.9 years with subarachnoid hemorrhage (23), ischemic stroke (8), subdural hematoma (4), intracerebral hemorrhage (3), intraventricular hemorrhage (2), and miscellaneous injuries (10) were enrolled. Data represented 2,337 total hours of continuous monitoring. Systolic BPs (SBP) were on average outside of recommended ranges 32.26 ± 30.46 % of the monitoring period. We subdivided adherence to ideal SBP range: optimal (≥99 % of time spent in NSICU within range) was achieved in 12 %, adequate (90 %) in 16 %, suboptimal (80 %) in 20 %, inadequate I (70 %) in 12 %, and inadequate II (<70 %) in 40 % of patients. Comparison of shift change %time and day versus night %time out of parameter yielded no statistically significant differences across SAH patients.
Conclusion
Hemodynamic management of patients with cerebrovascular injuries, based on targeted thresholds in the NSICU, yielded optimal control of SBP in only 28 % of our patients (within parameters ≥90 % of time).




Similar content being viewed by others
References
Leira R, et al. Early neurologic deterioration in intracerebral hemorrhage: predictors and associated factors. Neurology. 2004;63(3):461–7.
Jeffs L, et al. Patients’ views on bedside nursing handover: creating a space to connect. J Nurs Care Qual. 2014;29(2):149–54.
Albright KC, et al. Can comprehensive stroke centers erase the ‘weekend effect’? Cerebrovasc Dis. 2009;27(2):107–13.
Juul N, et al. Intracranial hypertension and cerebral perfusion pressure: influence on neurological deterioration and outcome in severe head injury. The Executive Committee of the International Selfotel Trial. J Neurosurg. 2000;92(1):1–6.
Spiotta AM, et al. Brain tissue oxygen-directed management and outcome in patients with severe traumatic brain injury. J Neurosurg. 2010;113(3):571–80.
Steiner LA, et al. Continuous monitoring of cerebrovascular pressure reactivity allows determination of optimal cerebral perfusion pressure in patients with traumatic brain injury. Crit Care Med. 2002;30(4):733–8.
Manley G, et al. Hypotension, hypoxia, and head injury: frequency, duration, and consequences. Arch Surg. 2001;136(10):1118–23.
Sheth KN, Sims JR. Neurocritical care and periprocedural blood pressure management in acute stroke. Neurology. 2012;79(13 Suppl 1):S199–204.
Fujii Y, et al. Multivariate analysis of predictors of hematoma enlargement in spontaneous intracerebral hemorrhage. Stroke. 1998;29(6):1160–6.
Dandapani BK, et al. Relation between blood pressure and outcome in intracerebral hemorrhage. Stroke. 1995;26(1):21–4.
Jauch EC, et al. Lack of evidence for an association between hemodynamic variables and hematoma growth in spontaneous intracerebral hemorrhage. Stroke. 2006;37(8):2061–5.
Tymianski M. Novel approaches to neuroprotection trials in acute ischemic stroke. Stroke. 2013;44(10):2942–50.
Group I.S.T.c., et al. The benefits and harms of intravenous thrombolysis with recombinant tissue plasminogen activator within 6 h of acute ischaemic stroke (the third international stroke trial [IST-3]): a randomised controlled trial. Lancet. 2012;379(9834):2352–63.
Fisher M. The ischemic penumbra: a new opportunity for neuroprotection. Cerebrovasc Dis. 2006;21(Suppl 2):64–70.
Del Zoppo GJ, et al. Expansion of the time window for treatment of acute ischemic stroke with intravenous tissue plasminogen activator: a science advisory from the American Heart Association/American Stroke Association. Stroke. 2009;40(8):2945–8.
Sacchetti ML. Is it time to definitely abandon neuroprotection in acute ischemic stroke? Stroke. 2008;39(6):1659–60.
Clark WM, et al. Recombinant tissue-type plasminogen activator (Alteplase) for ischemic stroke 3 to 5 hours after symptom onset. The ATLANTIS study: a randomized controlled trial. Alteplase thrombolysis for acute noninterventional therapy in ischemic stroke. JAMA. 1999;282(21):2019–26.
Adams HP Jr, et al. Guidelines for the early management of adults with ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups: the American Academy of Neurology affirms the value of this guideline as an educational tool for neurologists. Stroke. 2007;38(5):1655–711.
Jauch EC, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44(3):870–947.
European Stroke Initiative Writing, Cognard C, et al. Recommendations for the management of intracranial haemorrhage—part I: spontaneous intracerebral haemorrhage. The European Stroke Initiative Writing Committee and the Writing Committee for the EUSI Executive Committee. Cerebrovasc Dis. 2006;22(4):294–316.
Connolly ES Jr, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the American Heart Association/american Stroke Association. Stroke. 2012;43(6):1711–37.
Robertson CS. Management of cerebral perfusion pressure after traumatic brain injury. Anesthesiology. 2001;95(6):1513–7.
Muroi C, et al. Novel treatments for vasospasm after subarachnoid hemorrhage. Curr Opin Crit Care. 2012;18(2):119–26.
van Gijn J, Kerr RS, Rinkel GJ. Subarachnoid haemorrhage. Lancet. 2007;369(9558):306–18.
Acknowledgments
Financial Support: NIH Student Training Grant 5T35DK007431-29 MUSC Emergency Medicine, Neurosciences and Neurosurgery Departments.
Conflict of interest
Guilherme Porto, Alejandro Spiotta, Julio Chalela, Ryan Kellogg, and Edward Jauch declare that they have no interest of conflict.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Porto, G.B.F., Spiotta, A.M., Chalela, J.A. et al. Blood Pressure Guideline Adherence in Patients with Ischemic and Hemorrhagic Stroke in the Neurointensive Care Unit Setting. Neurocrit Care 23, 313–320 (2015). https://doi.org/10.1007/s12028-015-0116-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-015-0116-y