Abstract
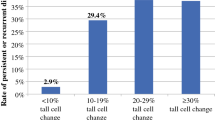
The morphologic criteria for tall cell variant (TCV) of papillary thyroid carcinoma (PTC) were modified in the 2017 WHO Classification of Tumors of Endocrine Organs, with a decrease in the requirements for both the height of cells and in the percentage of tumor demonstrating a tall cell morphology. The aim of this study was to determine if the change in criteria would result in a significant increase in the percentage of tumors that meet criteria for TCV. In addition, we evaluated the correlation between morphology, molecular alterations, and clinical behavior of TCV. We studied three cohorts to evaluate the above stated questions. The first cohort was comprised of 97 PTC consecutively resected over a 12-month period that were originally diagnosed as classic PTC, PTC with tall cell features, or TCV. Tumor slides of each case were reviewed to determine the percentage of the tall cell component (< 30%, 30–49%, and > 50%) and the height of the cells in this component. This cohort was evaluated to determine if the change in WHO criteria would result in a significant increase in the percentage of tumors that meet criteria for TCV. Our second cohort consisted of nine consecutively resected PTC with a tall cell component > 30% (with tall cells defined as at least 2–3× as tall as wide) that had molecular characterization through a targeted, next-generation sequencing (NGS) assay. The molecular characteristics were correlated with the percentage of the tall cell component. Finally, a third cohort comprised of seven clinically aggressive TCV (defined as those with T4 disease, disease recurrence, or subsequent tumor dedifferentiation) was evaluated to determine histologic and molecular characteristics. In cohort 1, the number of cases classified as TCV increased significantly with the change in definition of TCV: 8 (8%) cases met the previous criteria for TCV (cells 3× as tall as wide in > 50% of the tumor), whereas 24 (25%) cases met the new 2017 WHO criteria (cells 2–3× as tall as wide in > 30% of the tumor) (p = 0.0020). Molecular analysis of cohort 2 revealed that all 9 cases harbored a BRAF V600E mutation. Pathogenic secondary mutations were absent in cases with < 50% tall cells, but they were detected in 2 (33%) of 6 cases with > 50% tall cells (2 cases with TERT promoter mutations, including 1 that also had an AKT2 mutation). Histologic and molecular analysis of the clinically aggressive cohort (cohort 3), revealed that all cases had > 50% tall cells and 3 (43%) had secondary oncogenic mutations (all TERT promoter mutations). We found that the modified morphologic criteria put forth in the 2017 WHO tripled the number of cases that would be classified as TCV. Moreover, clinically aggressive tumors and those harboring secondary oncogenic mutations all had a tall cell component > 50%. Additional large multi-institutional studies incorporating clinical outcome and molecular data would be valuable to determine the best histologic definition of TCV.

Similar content being viewed by others
References
Haugen BR, Alexander EK, Bible KC et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. ed.^, eds.: Mary Ann Liebert, Inc. 140 Huguenot Street, 3rd Floor New Rochelle, NY 10801 USA, 2016; 1–133.
Wang X, Cheng W, Liu C, Li J Tall cell variant of papillary thyroid carcinoma: current evidence on clinicopathologic features and molecular biology. Oncotarget 7: 40792–40799, 2016.
Ito Y, Hirokawa M, Fukushima M, Inoue H., Yabuta T., Uruno T., Kihara M., Higashiyama T., Takamura Y., Miya A., Kobayashi K., Matsuzuka F., Miyauchi A. Prevalence and prognostic significance of poor differentiation and tall cell variant in papillary carcinoma in Japan. World journal of surgery 32: 1535–1543- discussion 1544-1535, 2008.
Kazaure HS, Roman SA, Sosa JA Aggressive variants of papillary thyroid cancer: incidence, characteristics and predictors of survival among 43,738 patients. Annals of surgical oncology 19: 1874–1880, 2012.
Morris LGT, Shaha AR, Tuttle RM, Sikora AG, Ganly I Tall-cell variant of papillary thyroid carcinoma: a matched-pair analysis of survival. Thyroid : official journal of the American Thyroid Association 20: 153–158, 2010.
DeLellis RA, Lloyd R, Heitz PU, Eng C World Health Organization Classification of Tumours: Pathology and Genetics Tumours of Endocrine Organs, 2004.
Lloyd RV, Osamura R, Kloppel G, Rosai J WHO Classification of Tumours of Endocrine Organs, 2017.
Beninato T, Scognamiglio T, Kleiman DA, Uccelli A, Vaca D, Fahey III TJ, Zarnegar R Ten percent tall cells confer the aggressive features of the tall cell variant of papillary thyroid carcinoma. Surgery 154: 1331–1336- discussion 1336, 2013.
Dettmer MS, Schmitt A, Steinert H et al. Tall cell papillary thyroid carcinoma: new diagnostic criteria and mutations in BRAF and TERT. Endocrine-related cancer 22: 419–429, 2015.
Ganly I, Ibrahimpasic T, Rivera M, Nixon I, Palmer F, Patel SG, Tuttle RM, Shah JP, Ghossein R Prognostic implications of papillary thyroid carcinoma with tall-cell features. Thyroid : official journal of the American Thyroid Association 24: 662–670, 2014.
Oh WJ, Lee YS, Cho U, Bae JS, Lee S, Kim MH, Lim DJ, Park GS, Lee YS, Jung CK Classic papillary thyroid carcinoma with tall cell features and tall cell variant have similar clinicopathologic features. Korean journal of pathology 48: 201–208, 2014.
Cancer Genome Atlas Research Network Integrated genomic characterization of papillary thyroid carcinoma. Cell 159: 676–690, 2014.
Liu R, Bishop J, Zhu G, Zhang T, Ladenson PW, Xing M Mortality Risk Stratification by Combining BRAF V600E and TERT Promoter Mutations in Papillary Thyroid Cancer: Genetic Duet of BRAF and TERT Promoter Mutations in Thyroid Cancer Mortality. JAMA oncology 3: 202–208, 2016.
Liu X, Bishop J, Shan Y, Pai S, Liu D, Murugan AK, Sun H, el-Naggar AK, Xing M Highly prevalent TERT promoter mutations in aggressive thyroid cancers. Endocrine-related cancer 20: 603–610, 2013.
Sholl LM, Do K, Shivdasani P et al. Institutional implementation of clinical tumor profiling on an unselected cancer population. JCI insight 1: e87062, 2016.
Garcia EP, Minkovsky A, Jia Y, Ducar MD, Shivdasani P, Gong X, Ligon AH, Sholl LM, Kuo FC, MacConaill LE, Lindeman NI, Dong F Validation of OncoPanel: A Targeted Next-Generation Sequencing Assay for the Detection of Somatic Variants in Cancer. Archives of pathology & laboratory medicine 141: 751–758, 2017.
Kandil E, Krishnan B, Noureldine SI, Yao L, Tufano RP Hemithyroidectomy: a meta-analysis of postoperative need for hormone replacement and complications. ORL; journal for oto-rhino-laryngology and its related specialties 75: 6–17, 2013.
Alexander C, Bader JB, Schaefer A, Finke C, Kirsch CM Intermediate and long-term side effects of high-dose radioiodine therapy for thyroid carcinoma. J Nucl Med 39: 1551–1554, 1998.
Almeida JP, Sanabria AE, Lima EN, Kowalski LP Late side effects of radioactive iodine on salivary gland function in patients with thyroid cancer. Head & neck 33: 686–690, 2011.
Brown AP, Chen J, Hitchcock YJ, Szabo A, Shrieve DC, Tward JD The risk of second primary malignancies up to three decades after the treatment of differentiated thyroid cancer. J Clin Endocrinol Metab 93: 504–515, 2008.
Iyer NG, Morris LG, Tuttle RM, Shaha AR, Ganly I Rising incidence of second cancers in patients with low-risk (T1N0) thyroid cancer who receive radioactive iodine therapy. Cancer 117: 4439–4446, 2011.
Sandeep TC, Strachan MW, Reynolds RM et al. Second primary cancers in thyroid cancer patients: a multinational record linkage study. J Clin Endocrinol Metab 91: 1819–1825, 2006.
Agrawal N, Abbott CE, Liu C, Kang S, Tipton L, Patel K, Persky M, King L, Deng FM, Bannan M, Ogilvie JB, Heller K, Hodak SP Noninvasive Follicular Tumor with Papillary-Like Nuclear Features: Not a Tempest in a Teapot. Endocr Pract 23: 451–457, 2017.
Hernandez-Prera JC, Machado RA, Asa SL, Baloch Z, Faquin WC, Ghossein R, LiVolsi VA, Lloyd RV, Mete O, Nikiforov YE, Seethala RR, Suster S, Thompson LD, Turk AT, Sadow PM, Urken ML, Wenig BM Pathologic Reporting of Tall-Cell Variant of Papillary Thyroid Cancer: Have We Reached a Consensus? Thyroid 27: 1498–1504, 2017.
Welch HG, Doherty GM Saving Thyroids - Overtreatment of Small Papillary Cancers. The New England journal of medicine 379: 310–312, 2018.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wong, K.S., Higgins, S.E., Marqusee, E. et al. Tall Cell Variant of Papillary Thyroid Carcinoma: Impact of Change in WHO Definition and Molecular Analysis. Endocr Pathol 30, 43–48 (2019). https://doi.org/10.1007/s12022-018-9561-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12022-018-9561-4