Abstract
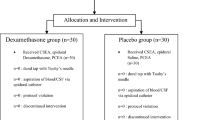
This randomized, double-blinded, placebo-controlled trial investigated the effect of continuous epidural butorphanol on intrathecal morphine-related pruritus in patients undergoing cesarean section. Eighty-three patients undergoing elective cesarean section under spinal anesthesia (1.5 mL of isobaric bupivacaine 0.5 % and 0.1 mg of preservative-free morphine) were enrolled in this study. Subjects were randomized to receive epidural butorphanol (n = 43) or normal saline combined bupivacaine (n = 40). In the study group, after the umbilical cord was clamped, patients were administered an epidural loading dose of 1 mg followed by a 48-h infusion of 0.004 % butorphanol with 0.1 % bupivacaine at a rate of 2 mL/h. In the normal saline group, saline was used for the loading dose and the infusion 0.1 % bupivacaine at a same rate. Postoperatively, a blinded observer recorded the incidence/severity of pruritus, visual analog pain scores and sedation level at 1, 3, 6, 9, 12, 24 and 48 h. The 48-h consumption of breakthrough analgesic (tramadol) was also noted. The primary outcome was the incidence of pruritus at 48 h. At 48 h, the incidence of pruritus was significantly lower in the butorphanol group (16.3 vs. 52.5 %; P < 0.001). Furthermore, compared with the normal saline group, the intensity of pruritus was also decreased with epidural butorphanol at 3, 6 and 9 h (all P ≤ 0.008). The pain scores were significantly lower at 12, 24 and 48 h (all P < 0.05) in the butorphanol groups. Patients only receiving bupivacaine required a higher cumulative dose of tramadol (37.5 ± 62.8 vs. 9.3 ± 36.6; P = 0.014). In patients undergoing elective cesarean section, continuous epidural butorphanol with bupivacaine decreases the incidence and severity of intrathecal morphine-related pruritus without adversely affecting the quality of postoperative analgesia.
Similar content being viewed by others
References
Rathmell, J. P., Lair, T. R., & Nauman, B. (2005). The role of intrathecal drugs in the treatment of acute pain. Anesthesia and Analgesia, 101(5 Suppl), S30–S43.
Aiono-Le Tagaloa, L., Butwick, A. J., & Carvalho, B. (2009). A survey of perioperative and postoperative anesthetic practices for cesarean delivery. Anesthesiology Research and Practice, 2009, 510642.
Szarvas, S., Harmon, D., & Murphy, D. (2003). Neuraxial opioid-induced pruritus: A review. Journal of Clinical Anesthesia, 15(3), 234–239.
Waxler, B., Dadabhoy, Z. P., Stojiljkovic, L., & Rabito, S. F. (2005). Primer of postoperative pruritus for anesthesiologists. Anesthesiology, 103(1), 168–178.
Kelly, M. C., Carabine, U. A., & Mirakhur, R. K. (1998). Intrathecal diamorphine for analgesia after caesarean section. A dose finding study and assessment of side-effects. Anaesthesia, 53(3), 231–237.
Jaw, S. P., Hoskins, B., & Ho, I. K. (1993). Opioid antagonists and butorphanol dependence. Pharmacology, Biochemistry and Behavior, 44(3), 497–500.
Nelson, K. E., & Eisenach, J. C. (2005). Intravenous butorphanol, meperidine, and their combination relieve pain and distress in women in labor. Anesthesiology, 102(5), 1008–1013.
Wu, Z., Kong, M., Wang, N., Finlayson, R. J., & De Tran, Q. H. (2012). Intravenous butorphanol administration reduces intrathecal morphine-induced pruritus after cesarean delivery: A randomized, double-blind, placebo-controlled study. Journal of Anesthesia, 26(5), 752–757.
Gunter, J. B., McAuliffe, J., Gregg, T., Weidner, N., Varughese, A. M., & Sweeney, D. M. (2000). Continuous epidural butorphanol relieves pruritus associated with epidural morphine infusions in children. Paediatric Anaesthesia, 10(2), 167–172.
Yokoyama, Y., Yokoyama, T., Nagao, Y., Nakagawa, T., & Magaribuchi, T. (2009). Treatment of epidural morphine induced pruritus with butorphanol. Masui, 58(2), 178–182.
Hu, B., Lu, Z., Li, G., & Li, G. (2004). Effect of hot compress on intrathecal morphine-induced pruritus. A series of 90 cases. [Chinese]. Journal of Fourth MiI Medical University, 25, 1156.
Lockington, P. F., & Fa’aea, P. (2007). Subcutaneous naloxone for the prevention of intrathecal morphine induced pruritus in elective Caesarean delivery. Anaesthesia, 62(7), 672–676.
Ramsay, M. A., Savege, T. M., Simpson, B. R., & Goodwin, R. (1974). Controlled sedation with alphaxalone–alphadolone. British Medical Journal, 2(5920), 656–659.
Flaherty, S. A. (1996). Pain measurement tools for clinical practice and research. AANA Journal, 64(2), 133–140.
Gerancher, J. C., Floyd, H., & Eisenach, J. (1999). Determination of an effective dose of intrathecal morphine for pain relief after cesarean delivery. Anesthesia and Analgesia, 88(2), 346–351.
Palmer, C. M., Emerson, S., Volgoropolous, D., & Alves, D. (1999). Dose-response relationship of intrathecal morphine for postcesarean analgesia. Anesthesiology, 90(2), 437–444.
Gutstein, H. B., & Akil, H. (2006). Opioid analgesics. In J. G. Hardman, L. E. Limberd, & A. G. Gilman (Eds.), Goodman and Gilman’s the pharmacological basis of therapeutics (11th ed., pp. 547–590). New York: McGraw-Hill.
Colbert, S., O’Hanlon, D. M., Galvin, S., Chambers, F., & Moriarty, D. C. (1999). The effect of rectal diclofenac on pruritus in patients receiving intrathecal morphine. Anaesthesia, 54(10), 948–952.
Ballantyne, J. C., Loach, A. B., & Carr, D. B. (1988). Itching after epidural and spinal opiates. Pain, 33(22), 149–160.
Jinks, S. L., & Carstens, E. (1998). Spinal NMDA receptor involvement in expansion of dorsal horn neuronal receptive field area produced by intracutaneous histamine. Journal of Neurophysiology, 79(4), 1613–1618.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wu, Z., Kong, M., Chen, J. et al. Continous Epidural Butorphanol Decreases the Incidence of Intrathecal Morphine-Related Pruritus After Cesarean Section: A Randomized, Double-Blinded, Placebo-Controlled Trial. Cell Biochem Biophys 70, 209–213 (2014). https://doi.org/10.1007/s12013-014-9884-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12013-014-9884-9