Opinion statement
Clinical presentation, neurologic condition, and imaging findings are the key components in establishing a treatment plan for acute SDH. Location and size of the SDH and presence of midline shift can rapidly be determined by computed tomography of the head. Immediate laboratory work up must include PT, PTT, INR, and platelet count. Presence of a coagulopathy or bleeding diathesis requires immediate reversal and treatment with the appropriate agent(s), in order to lessen the risk of hematoma expansion. Reversal protocols used are similar to those for intracerebral hemorrhage, with institutional variations. Immediate neurosurgical evaluation is sought in order to determine whether the SDH warrants surgical evacuation. Urgent or emergent surgical evacuation of a SDH is largely influenced by neurologic examination, imaging characteristics, and presence of mass effect or elevated intracranial pressure. Generally, evacuation of an acute SDH is recommended if the clot thickness exceeds 10 mm or the midline shift is greater than 5 mm, regardless of the neurologic condition. In patients with patients with an acute SDH with clot thickness <10 mm and midline shift <5 mm, specific considerations of neurologic findings and clinical circumstances will be of importance. In addition, consideration will be given as to whether an individual patient is likely to benefit from surgery. For an acute SDH, evacuation by craniotomy or craniectomy is preferred over burr holes based on available data. Postoperative care includes monitoring of resolution of pneumocephalus, mobilization and drain removal, and monitoring for signs of SDH reaccumulation. Medical considerations include seizure prophylaxis and management as well as management and resumption of antithrombotic and anticoagulant medication.
Similar content being viewed by others
Introduction
Subdural hematomas (SDH) are commonly classified as acute or chronic SDH. Those definitions are arbitrarily made by time of onset and imaging characteristics, without clear criteria or consensus literature. Acute SDH in the setting of severe traumatic brain injury (TBI) is usually associated with underlying parenchymal brain injury, while nontraumatic SDH or SDH after minor to moderate trauma is often isolated. Acute-on-chronic SDH ensues if a patient with a chronic SDH develops acute bleeding over the chronic SDH. Treatment approach to this underreported entity largely depends on the relative size and effect of the acute component, and is similar to either acute or chronic SDH in most cases [1]. For the purpose of this review, we will focus on acute SDH in adult patients.
Hemorrhage in the subdural space is caused by tearing of a surface or bridging vessel [2], usually subsequent to an acceleration-deceleration motion [3]. Venous bleeding is usually halted by rising intracranial pressure (ICP) or direct compression by the clot itself [4]. An arterial source accounts for up to 30 % of SDH cases, and is usually caused by rupture of small (<1 mm in diameter) cortical arteries [4, 5]. The etiology may predispose for different SDH locations: If caused by arterial rupture, the SDH is more likely found temporoparietal, while SDH those caused by tearing of bridging veins are predominately located frontoparietal [5]. Intracranial hypotension with resultant traction on bridging veins or engorgement of cerebral veins and subsequent leakage of fluid into the subdural space is another mechanism that can lead to SDH formation [6]. After the initial SDH accumulation, over a period of about 2 weeks, synthesis of dural collagen is induced and fibroblastic growth results in formation of a thick outer membrane over the inner dural surface, followed by encapsulation of the clot [7].
The most common cause for SDH is head trauma related to motor vehicle or other accidents, falls, or assaults [8]. Spontaneous SDH, ie, occurrence of SDH in absence of provoking factors, is much less common, 2.6 % in one report of acute SDH [9]. Underlying etiologies include ruptured aneurysms with or without concomitant SAH [10], arteriovenous malformations [11], meningiomas [12], dural metastatic disease [13], and hematologic or solid neoplasms [14, 15]. Common risk factors for the development of a SDH include cerebral atrophy [7], use of antithrombotic agents [16], and coagulopathy [17]. The exact incidence of acute SDH is unknown, and depends on the patient age group. As cerebral atrophy poses a risk, acute SDH associated with minor trauma is more commonly seen in older patients, however, acute SDH associated with severe head injury is predominantly seen in younger men.
Clinical presentation depends on the extent of the SDH and comprises a wide spectrum of manifestations, from asymptomatic, headaches, ipsi- or contralateral focal deficits, over seizures to disturbances of consciousness [2]. Similar to the rates of incidence, mortality depends on circumstances and clinical factors. Acute SDH in the setting of major head trauma is one of the most lethal head injuries, with estimated mortality rates between 50 %–90 % [18], while in-hospital mortality in acute SDH not related to major trauma has been found to be 11.8 % [19]. The level of consciousness on presentation is a major predictive factor for mortality [20]. Survival furthermore depends on SDH characteristics (thickness, midline shift) [21], hematoma volume [22], patient age [22], and patency of the basal cisterns [23].
Treatment
Immediate treatment considerations
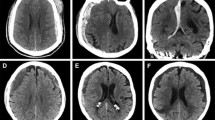
Imaging is key to make the diagnosis and establish a treatment plan. Head computed tomography (CT) is the fastest modality to determine presence, size and acuity of a SDH, and presence and size of midline shift (MLS). Immediate laboratory work up must include PT, PTT, INR, and platelet count. General treatment considerations include the assessment for need of mechanical ventilation, correction of a coagulopathy and treatment of seizures. Any patient with a confirmed or suspected acute SDH is at risk of rapid deterioration and should have immediate neurosurgical consultation to decide for surgical or nonsurgical management.
Pharmacologic treatment
Reversal of coagulopathy
A coagulopathy may be present due to the use of prescription antithrombotic or anticoagulant medication, or due to an underlying medical condition. Specific risks and interventions to reverse a coagulopathy vary depending on the underlying etiology.
The risk of hematoma expansion renders any intracerebral hemorrhage (ICH) a potentially life-threatening situation. Hematoma expansion in the setting of coagulopathy is a well recognized risk in patients with SDH [24]. In one study, radiographic SDH expansion was found in 20 %–22 %; clinically significant expansion of SDH occurred in 10.7 %–11.6 %, which was a similar rate for warfarin-related SDH and patients not taking warfarin [25]. For acute-on-chronic SDH, consideration needs to be given to the fact that solid clot formation may not occur due to excessive activation of coagulation and fibrinolytic systems [1], and therefore even a smaller acute component can potentially pose risk for expansion. Studies comparing mortality in traumatic head injury in patients with anticoagulation with warfarin vs control patients found differences in mortality rates up to 30 % [26]. Coagulopathy was found to be independently associated with increased risk of in-hospital death in patients with acute SDH [24]. The degree of anticoagulation as indicated by the admission INR has been shown to directly correlate to mortality in warfarin-treated trauma patients [27]. On the other hand, the potential benefit of reversing anticoagulation must be weighed against the individual risk of reversing anticoagulation. Most data on reversal strategies stem from treatment of anticoagulant-associated ICH rather than SDH. Furthermore, data are very limited on the risk of bleeding with subtherapeutic INR, and the ideal target for INR reversal. A target INR of 1.2–1.5 is usually considered adequate reversal [28, 29]. Rapid reversal is key and has been shown to reduce hemorrhage progression and mortality for ICH [30]. Normalizing the INR as soon as possible is a very important determinant for successful INR reversal: Every 30 minutes of delay in the first dose of fresh frozen plasma (FFP) in one study was associated with a 20 % decreased odds of INR reversal within 24 hours [31]. Options for reversal include the administration of Vitamin K, FFP, prothrombin complex concentrates (PCC), and recombinant activated factor VII (rFVIIa).
Vitamin K
Vitamin K not only is an essential component of warfarin reversal due to the inhibited formation of factors II, VII, IX, and X by warfarin [32], but should be administered to all patients with anticoagulant-related ICH, as it boosts synthesis of clotting factors and prevents rebound coagulopathy after FFP, PCC, or rFVIIa, which all have short half-lives, have worn off [33].
- Standard dosage :
-
The usual dose for intravenous (iv.) vitamin K is 5–10 mg infused at a rate of 1 mg/min [34], with most reversal protocols using 10 mg [35]. Additional subsequent doses can be given to achieve adequate coagulation [36]. Iv. administration of vitamin K is recommended by most guidelines of national organizations [37], as it results in lowering the INR as early as 2 hours [38].
- Main side effect :
-
The major risk associated with iv. administration, anaphylaxis, is minimized by slow infusion and newer preparations [39].
Fresh frozen plasma
FFP, the most widely used factor replacement in the U.S., contains factors I, II, V, VII, IX, X, XI, XIII, and antithrombin.
- Standard dosage :
-
Large volumes of FFP (10–15 mL/kg) are often required for full reversal of anticoagulation. For calculation of dosing for an individual patient, a recent study proposed the formula “DeltaINR after 1 FFP = 0.57 × PreINR – 0.72” [40].
- Main side effects :
-
Like for other blood products, there is a risk for transfusion-related events [41]. Large transfusion volumes bear the risk of volume overload and pulmonary edema [42].
- Special points :
-
Due to requirement for type-specific matching, thawing, and delivery from blood bank, transfusion may be associated with significant delays [31]. Immediate administration of 2 units of universal donor FFP significantly reduced mortality rates in one study [35].
Prothrombin complex concentrates
PCC contain factors II, VII, IX, and X in varying amounts highly concentrated in small amounts of volume. PCCs can correct the INR within minutes.
- Standard dosage :
-
Dosing must be individualized based on PCC product used, patient’s INR, clinical situation, and extent of SDH.
- Special points :
-
In a study comparing PCC and FFP, there was no difference in hematoma growth in patients whose INR was corrected within 2 hours [43], however, recent data showed that survival was better when using PCC as part of a reversal protocol for ICH [44]. Urgent warfarin reversal using FFP vs PCC in emergency departments showed faster reversal, lower red cell transfusion requirements and fewer adverse events for PCC compared with FFP [45]. Retrospective data on neurosurgical patients, including patients with SDH undergoing surgical intervention, showed that PCC as part of the reversal protocol were effective and safe [46], but randomized prospective data are lacking to date.
Recombinant activated factor VII
rFVIIa is a hemostatic agent with rapid onset and a half-life of about 2.5 hours [47]. Its safety and efficacy has been evaluated for treatment of traumatic ICH. While there were higher rates of thromboembolic events in the rFVIIa group, this was not a statistically significant difference. Furthermore, use of rFVIIa may reduce ICH expansion, but it failed to improve mortality or functional outcome [48, 49].
- Standard dosage :
-
10–100 mcg/kg iv. [50].
- Main side effects :
-
Thromboembolic events.
- Special points :
-
This is an unlabeled use for rFVIIa. Lower doses (10–20 mcg/kg) are preferred given higher risk of thromboembolic events with higher dosing. Response is individually variable. Per American Heart Association guidelines, routine use as single agent is not recommended for warfarin-related ICH [51]. In comparison, reversal with FFP takes longer than with rFVIIa or PCC, and rFVIIa and PCC seem to be more effective, but carry a higher risk of INR rebound [52••].
Pharmacologic reversal strategies for other anticoagulants
- Heparin :
-
For patients on heparin, full reversal can be achieved by slow iv. infusion of protein sulfate at a dose of 1 mg protamine sulfate/100 units heparin [53]. The exact dosing depends on dose and timing of heparin given. For low molecular weight heparin (LMWH), only partial reversal can be achieved with protein sulfate [54]. A dose of 1 mg/100 anti-Xa units of LMWH, or smaller doses when LMWH was given more than 8 hours prior, may reduce clinical bleeding [55].
- Pentasaccharide anticoagulants :
-
For patients treated with fondaparinux or other pentasaccharide anticoagulants, the limited yet best available data support the use of rFVIIa, despite this not being an approved indication, and with uncertainty regarding optimal dosing and role for concomitant therapeutics or transfusions [56].
- Direct thrombin or factor Xa inhibitors :
-
There are no specific reversal agents for newer anticoagulants, such as direct thrombin inhibitors (eg, dabigatran) or direct Xa inhibitors (eg, rivaroxaban), and experience with SDH in patients taking these medications is limited. There is some suggestion that PCCs may have limited effectiveness in reversing the effect of rivaroxaban but not of dabigatran [57]. The use of rFVIIa in ICH patients on dabigatran has shown theoretical potential [58].
Reversal of antiplatelet effects
For antithrombotics, data vary regarding the impact of antiplatelet therapy on hematoma expansion and outcome for patients presenting with ICH, but overall, increased risk of hematoma growth while on these agents is suggested [59]. Prehospital antiplatelet therapy in head trauma patients is associated with increased morbidity but not clearly with increased risk of mortality when compared with those patients not treated before injury [60, 61]. Furthermore, it is uncertain whether the use of aspirin increases the risk of SDH. The overall incidence is low, but varies depending on the age of the patient population [62•]. Possible therapeutics for reversal of antiplatelet therapy in patients with head injury include platelets, desmopressin, and rFVIIa [63]. Clear data and guidelines for treatment when antiplatelet intake is known are lacking, and practice for use of transfusions or therapeutics ranges widely. While the use of platelet transfusions in patients with TBI on preinjury antiplatelet therapy has been reviewed, baseline demographics, and transfusion protocols were variable and patient numbers too small to assess correlation of transfusion with mortality and morbidity outcomes [60, 64]. The clinical utility of desmopressin and rFVIIa has not been assessed for reversal of coagulopathies associated with prehospital antiplatelet therapy in patients with SDH. In a study for reversal of antiplatelet effects of clopidogrel and aspirin prior to a neurosurgical procedure, desmopressin lead to improved platelet function from 48 %–71 % when infused at 0.3 g/kg over 20 minutes [65].
Seizures in patients with SDH
Acute SDH is known to be a risk factor for early post-traumatic seizures [66]. In a series of acute SDH, 3 % had seizures prior to surgery, and 25 % during the acute postoperative period, with a median time of 1 day to the first postoperative seizure [67]. Isolated acute SDH, evacuation by craniotomy and worse GCS before and after surgery were found to be predictive of postoperative seizures after acute SDH [67].
- Indication for pharmacologic treatment :
-
Recommendations for TBI in general, and thus, pertaining to traumatic acute SDH, suggest use of antiepileptic drugs (AEDs) if the presentation is accompanied by seizures, if the level of consciousness is decreased (GCS <10), and/or if the CT scan is abnormal [68••] (Class I evidence, Level A recommendation for use of phenytoin in adult patients with severe TBI by the American Academy of Neurology). In acute SDH without history of even minor or trivial trauma, practice varies between institutions regarding AED prophylaxis. Given the high prevalence of a history of minor trauma in patients with acute SDH, which may initially often be underreported [67], our practice is to use AED prophylaxis for one week unless there are contraindications or the risk of AED prescription outweighs the benefit.
- Duration of treatment :
-
Prophylactic anti-epileptics are effective in reducing early seizures, but not late seizures, rate of mortality or and disability [69]. Therefore, anticonvulsant prophylaxis is usually stopped after 7 days if there is no seizure activity [68••].
- Specific agents :
-
Phenytoin has been studied the most and proven to be efficient in preventing early post-traumatic seizures TBI patients [70]. Due to its favorable side effect profile, levetiracetam is now being used commonly. In available data, levetiracetam and phenytoin demonstrate equal efficacy in seizure prevention after brain injury [71].
Surgery
Surgical vs nonsurgical management
Urgent need for surgical evacuation of a SDH is largely influenced by neurologic examination, acuity of the hemorrhage, imaging characteristics, and presence of mass effect or elevated intracranial pressure. When patients with acute SDH present with other associated intracranial injuries, such as contusions or diffuse axonal injury, a GCS of <15 at presentation is not necessarily an indication to operate. Further aspects for triage into operative and nonoperative management are age of the patient, advanced directives, and the probability of a favorable outcome. No randomized trials have compared surgery with conservative management for patients with acute SDH. Multiple studies have shown that patients with acute SDH >10 mm in initial hematoma thickness or >5 mm of MLS are likely to require operative intervention [23, 72, 73].
- Indications for surgery :
-
To date, recommended indications for surgical intervention for acute SDH as purposed by the Congress of Neurological Surgeons and American Association of Neurosurgeons are [8] (Class IV evidence):
-
Evacuation of an acute SDH with clot thickness >10 mm or midline shift >5 mm, regardless of the Glasgow coma scale (GCS) score
-
Patients with an acute SDH with clot thickness <10 mm, midline shift <5 mm, and GCS <9 should receive monitoring of intracranial pressure (ICP) and can be treated nonoperatively if they are neurologically stable since the injury, have no pupillary abnormalities, and have no intracranial hypertension (ICP >20 mm Hg)
-
In a large cohort of patients with nontraumatic SDH, surgical evacuation was associated with decreased mortality compared with nonsurgical management [19]. However, prior to any intervention, careful consideration must be given to whether the patient is likely to benefit from surgery. Pupillary abnormalities or low GCS are significant predictors of poor outcome [74, 75, 76••]. The mortality rate for patients with acute SDH and one unreactive pupil on initial examination was 81 % and 97 % for those with bilateral unreactive pupils [74]. Furthermore, associated intracranial lesions were predictive of a higher mortality rate (91 %) [74]. Mortality rates also rise steeply with lower GCS scores on presentation, with fatality rates of 93 % and higher for GCS of 3 [20, 74]. For higher GCS scores, mortality rates vary with other factors such as age of the patient, from 45 %–82 % in one study [20]. Multiple studies have also shown that older patients, especially those with low GCS, are less likely to have a meaningful recovery after SDH evacuation [22, 76••, 77–79]. However, in a large inpatient sample for nontraumatic acute SDH, surgical SDH evacuation was associated with decreased in-hospital mortality especially in the elderly patient population [19]. Consideration should also be given to comorbidities and medical factors determining surgical candidacy, as most surgeries will have to be performed emergently or urgently, therefore not permitting for detailed preoperative risk stratification or medical optimization. Cardiac abnormalities and preexisting cardiac disease, for example, are commonly found in patients with isolated acute SDH [80].
- Indications for nonsurgical management :
-
Limited observational data suggest that stable patients with isolated small acute SDH can be managed nonoperatively [72, 73]. Nonoperative management in an intensive care unit is also recommended for neurologically stable patients with an acute traumatic SDH with clot thickness <10 mm, midline shift <5 mm, without pupillary abnormalities, and no intracranial hypertension on ICP monitoring when presenting with a GCS score <9 [8]. Outcomes were reported to be at least as safe for those patients compared with surgical treatment when ICP and clinical condition remained stable [23]. If triaged to nonsurgical treatment, close observation, ICP monitoring if indicated, and serial brain imaging are important, as hematoma enlargement and neurologic deterioration requiring surgery may occur later on. For patients with traumatic head injury, serial follow-up head CT scans should be obtained during the first 36 hours after injury, as there is a high incidence of clot expansion during this interval [81]. The individual timing of the first follow-up scan depends on the initial presentation and findings.
- Change of treatment plan to surgical evacuation :
-
Risk factors for hematoma expansion and eventual requirement of surgery include lower GCS score on presentation, additional intracranial injuries on CT scan such as mass effect, intraventricular hemorrhage, and epidural hematoma [81], as well as a combination of neurologic worsening and MLS >5 mm [82], or neurologic deterioration in the setting of initial clot thickness >10 mm [72].
Timing of surgery
When the decision is made to proceed with hematoma evacuation, the expert panel recommendations are to avoid delay in surgical intervention [8]. However, multiple studies have produced conflicting results regarding outcomes and time to surgery [20, 76••, 83, 84]. One explanation for this could be that patients with more severe injury are likely to undergo surgery more rapidly, but subsequently produce poorer outcomes for the early surgery cohort. Two studies analyzing time to surgery from onset of coma and herniation, respectively, show improved outcomes for those who underwent surgery within 2–4 hours of clinical deterioration [83, 84]. While there is no defined “window” for surgical intervention, there is evidence to suggest that outcomes can be influenced by reducing the time between symptom onset and hematoma evacuation.
Standard procedure
- Surgical technique :
-
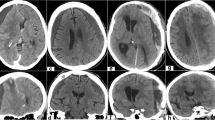
Surgical techniques available for evacuation of acute SDH include craniotomy, decompressive craniectomy, burr hole trephination, or craniostomy procedures [8]. The choice of procedure is influenced by the treating surgeon and the individual patient. The most commonly applied techniques for acute SDH are craniotomy and decompressive craniectomy, with or without duraplasty. Surgical evacuation of acute SDH is performed in a fully staffed operating room, with sterile technique, and under general anesthesia. Given that most SDH undergoing surgical treatment are fronto-parietal or hemispheric in distribution, a large frontal-temporal-parietal craniotomy is usually performed with special attention to the frontal and temporal poles. The craniotomy is started over the temporal lobe, which allows for immediate hematoma evacuation and brainstem decompression. Once the craniotomy is completed, the dura is opened widely. The hematoma is then removed with irrigation, suction, and forceps [85]. Usually, a torn bridging vein or a cortical contusion can be identified and then controlled with bipolar cautery and/or hemostatic agents. Figure 1 shows an example of a frontotemporal craniotomy. If a dural sinus injury is suspected, the anesthesiologist should be alerted to the possibility of significant blood loss as well as the need to monitor for air embolism. While a subdural drain may be left in situ in the setting of coagulopathy or active oozing, primary hemostasis must be obtained in order to prevent reaccumulation of the hematoma. When the brain is relaxed and sunken away from the craniotomy site, a water-tight dural closure is performed and the bone flap is replaced. However, if there is significant edema, or if there is concern for future swelling, the initial craniotomy may be left open or even be extended to allow for adequate decompression. In presence of significant amount of cerebral edema, the dura is only loosely approximated and the scalp flap is closed. The bone flap is stored sterilely in the bone bank and replaced at a later date [85].
- Considerations for surgical technique :
-
Few studies have compared outcome between surgical procedures. In a series evaluating patients with burr holes, craniotomy with or without dural graft or decompressive craniectomies, a significant increase in morbidity and mortality for those patients treated with burr holes alone was found [20]. While burr hole evacuation is an effective treatment for chronic SDH, the technique is poorly suited and rarely used for acute SDH due to the inadequate exposure and inability to visualize and control active hemorrhage. However, for acute-on-chronic SDH, burr hole evacuation may be the best treatment approach, depending on clot density and relative size of the acute clot compared with the chronic component [1]. To date, there are no data to evaluate burr hole evacuation as a less invasive possibility selectively for the elderly who may not be a good candidate for a major surgical procedure. Decompressive hemicraniectomy, with removal of a more extensive bone flap, which is stored and then replaced weeks to months later, has also been compared with standard craniotomy. The enhanced decompression may help to decrease ICP and is theorized to improve outcomes. However, recent studies have failed to show a difference from the standard approach [86, 87•, 88]. Any potential advantages to craniectomy must be weighed against the added risk of the need to replace the bone flap in a second, later, surgical procedure, the cranioplasty. The complication rate for cranioplasty has been found as high as 34 %, with 16 % of unilateral cranioplasties requiring additional surgery [89].
Postoperative care after SDH evacuation
Postoperative care after SDH evacuation is similar to that of other cranial procedures. The patient is ideally extubated and transferred to an intensive care unit. Immediate clinical follow-up usually consists of hourly neurologic examination checks and a postoperative CT scan of the head. Perioperative antibiotic prophylaxis is continued for a period of 24 hours after surgery. The use of subdural or subgaleal drains after acute SDH is often surgeon-dependent and is yet to be evaluated in the literature. Similarly, there is no set time for drain removal, and there are large variations between institutions. Typically, removal will be approached hours to days later, when the draining fluid has assumed a serosanguinous quality and the output is decreasing. The patient is then mobilized, starting with elevation of the bed and then ambulation if possible. During the period of mobilization, it is important to monitor for development of headaches or other symptoms or signs of pneumocephalus. Furthermore, monitoring for reaccumulation of the SDH is important. The exact incidence of re-hemorrhage for acute SDH is not known and varies with patient population. In a large cohort with acute nontraumatic SDH, 7.4 % of patients required repeat evacuation during the same hospitalization [19].
Pneumocephalus after SDH evacuation
Pneumocephalus is common after neurosurgical procedures, especially craniotomies [90]. One series found that in at least 66 % of postcraniotomy scans, 5 %–10 % of intracranial volume was occupied by air [91]. Predisposing factors for pneumocephalus after evacuation of were age >60 years and MLS >5 mm [92]. An important factor for development and evolution of pneumocephalus is head positioning during surgery and closure [93]. Furthermore, duration of surgery, hydrocephalus, intraoperative osmotherapy, and hyperventilation include some of the intra- and perioperative factors believed to facilitate the development of pneumocephalus [94]. To date, no particular anesthetic technique has been shown to decrease the amount of pneumocephalus after neurosurgical procedures [94]. Clinically, pneumocephalus can remain asymptomatic or manifest with headaches, nausea and vomiting, seizures, dizziness, and depressed neurologic status [95]. Tension pneumocephalus can be life-threatening [96], as it behaves in a similar way as an intracranial space-occupying lesion causing intracranial hypertension with potential downward herniation [97]. Air embolism and cardiac arrest can occur as a consequence of pneumocephalus [97, 98]. The development of tension pneumocephalus has frequently been reported after SDH evacuation, especially burr hole evacuation of chronic SDH [99, 100]. Imaging signs of tension pneumocephalus include separation and compression of the frontal lobes with widened interhemispheric fissure resembling the silhouette of Mount Fuji (“Mount Fuji sign”), and presence of multiple small air bubbles scattered through several cisterns (“air bubble sign”) [101]. For bilateral subdural collections, which pose a special challenge to keep the amount of pneumocephalus small, setting of the incision with intact dura and rapid turning of the head after completion of one side has been suggested to minimize the time required to drain both subdural collections [94]. Another possibility is to reposition the head during dural closure in a way that facilitates the escape of remaining air by bringing the dural defect to the highest point of the cranial cavity [94].
Treatment of pneumocephalus commonly consists of supplemental oxygen. Several reports show the hastened resolution of intracranial air collections with higher concentrations of oxygen [102]. In a study comparing 100 % oxygen via non-rebreather mask and room air for 24 hours, the mean rate of pneumocephalus reduction in the non-rebreather group was 65 % vs 31 % in the control group [90]. Pneumocephalus resulting from small bone defects may respond well to conservative measures such as bed rest, head of bed elevation, avoidance of positive pressure, and pain control [103].
Considerations for follow-up
If a craniectomy was performed, the patient will have to wear a helmet when out of bed. Sutures are typically removed on postoperative day 10–14. Repeat imaging is often performed several weeks after surgery to monitor for chronic subdural development.
Resuming antiplatelets and anticoagulation after SDH
There are no unified management criteria regarding the timing for resumption of anticoagulation following a surgically treated SDH. For ICH, most available data on resumption of anticoagulation concern patients with mechanical heart valves, as this is one of the most pressing reasons for anticoagulation [104, 105]. The general opinion concerning anticoagulation in prosthetic valve patients is that it can be withheld safely for 2–3 weeks [106]. In a series of 12 SDH patients with evacuation of SDH while on anticoagulation for mechanical heart valve, anticoagulation was withheld for an average of 9 days, without major bleeding or thrombotic complications [107]. In another series of SDH patients who underwent surgical evacuation, the authors concluded that anticoagulation therapy can be discontinued for up to 1–2 weeks with minimal risk of thromboembolism [108]. In a study of patients with ICH, 54 % had resumed anticoagulation by day 30 without recurrence of ICH [109]. For ICH, Eckman et al. published a decision analysis with respect to anticoagulation for atrial fibrillation [105]; however, similar data are not available for SDH. It is our experience that, in the absence of guidelines or data, the timing of resumption of anticoagulation is for the most part subject to the neurosurgeon’s individual assessment of a given case.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Lee KS et al. Acute-on-chronic subdural hematoma: not uncommon events. J Korean Neurosurg Soc. 2011;50(6):512–6.
Victor M, Ropper A. Craniocerebral trauma. In: Ropper A, Victor M, editors. Adams and victor’s principles of neurology. New York: McGraw-Hill; 2001. p. 925.
Besenski N. Traumatic injuries: imaging of head injuries. Eur Radiol. 2002;12(6):1237–52.
Gennarelli TA, Thibault LE. Biomechanics of acute subdural hematoma. J Trauma. 1982;22(8):680–6.
Maxeiner H, Wolff M. Pure subdural hematomas: a postmortem analysis of their form and bleeding points. Neurosurgery. 2002;50(3):503–8. discussion 508–9.
Holmes JM. Intracranial hypotension associated with subdural haematoma. Br Med J. 1953;1(4824):1363–6.
Mayer S, Rowland L. Head Injury. In: Rowland L, editor. Merritt’s Neurology. Philadelphia: Lippincott Williams & Wilkins; 2000. p. 401.
Bullock MR et al. Surgical management of acute subdural hematomas. Neurosurgery. 2006;58(3 Suppl):S16–24. discussion Si–iv.
Komatsu Y et al. Acute subdural hemorrhage of arterial origin: report of three cases. No Shinkei Geka. 1997;25(9):841–5.
Gelabert-Gonzalez M, Iglesias-Pais M, Fernandez-Villa J. Acute subdural haematoma due to ruptured intracranial aneurysms. Neurosurg Rev. 2004;27(4):259–62.
Rengachary SS, Szymanski DC. Subdural hematomas of arterial origin. Neurosurgery. 1981;8(2):166–72.
Okuno S et al. Falx meningioma presenting as acute subdural hematoma: case report. Surg Neurol. 1999;52(2):180–4.
Bergmann M, Puskas Z, Kuchelmeister K. Subdural hematoma due to dural metastasis: case report and review of the literature. Clin Neurol Neurosurg. 1992;94(3):235–40.
Ichimura S et al. Nontraumatic acute subdural hematoma associated with the myelodysplastic/myeloproliferative neoplasms. J Neurosci Rural Pract. 2012;3(1):98–9.
Reichman J et al. Subdural hematoma in patients with cancer. Neurosurgery. 2012;71(1):74–9.
Reymond MA et al. Aspirin as a risk factor for hemorrhage in patients with head injuries. Neurosurg Rev. 1992;15(1):21–5.
Seckin H et al. Chronic subdural hematoma in patients with idiopathic thrombocytopenic purpura: a case report and review of the literature. Surg Neurol. 2006;66(4):411–4. discussion 414.
Wilberger Jr JE, Harris M, Diamond DL. Acute subdural hematoma: morbidity, mortality, and operative timing. J Neurosurg. 1991;74(2):212–8.
Busl KM, Prabhakaran S. Predictors of mortality in nontraumatic subdural hematoma. J Neurosurg. 2013.
Hatashita S et al. Acute subdural hematoma: severity of injury, surgical intervention, and mortality. Neurol Med Chir (Tokyo). 1993;33(1):13–8.
Zumkeller M et al. Computed tomographic criteria and survival rate for patients with acute subdural hematoma. Neurosurgery. 1996;39(4):708–12. discussion 712–3.
Howard III MA et al. Acute subdural hematomas: an age-dependent clinical entity. J Neurosurg. 1989;71(6):858–63.
Servadei F et al. Importance of a reliable admission Glasgow Coma Scale score for determining the need for evacuation of post-traumatic subdural hematomas: a prospective study of 65 patients. J Trauma. 1998;44(5):868–73.
Bershad EM et al. Coagulopathy and in hospital deaths in patients with acute subdural hematoma. J Neurosurg. 2008;109(4):664–9.
Roguski M, et al. Mild elevations of international normalized ratio at hospital Day 1 and risk of expansion in warfarin-associated subdural hematomas. J Neurosurg. 2013.
McMillian WD, Rogers FB. Management of prehospital antiplatelet and anticoagulant therapy in traumatic head injury: a review. J Trauma. 2009;66(3):942–50.
Pieracci FM et al. Degree of anticoagulation, but not warfarin use itself, predicts adverse outcomes after traumatic brain injury in elderly trauma patients. J Trauma. 2007;63(3):525–30.
Oyama H et al. Acute subdural hematoma in patients with medication associated with risk of hemorrhage. Neurol Med Chir (Tokyo). 2011;51(12):825–8.
Panczykowski DM, Okonkwo DO. Premorbid oral antithrombotic therapy and risk for reaccumulation, reoperation, and mortality in acute subdural hematomas. J Neurosurg. 2010;114(1):47–52.
Ivascu FA et al. Rapid warfarin reversal in anticoagulated patients with traumatic intracranial hemorrhage reduces hemorrhage progression and mortality. J Trauma. 2005;59(5):1131–7. discussion 1137–9.
Goldstein JN et al. Timing of fresh frozen plasma administration and rapid correction of coagulopathy in warfarin-related intracerebral hemorrhage. Stroke. 2006;37(1):151–5.
Hanslik T, Prinseau J. The use of vitamin K in patients on anticoagulant therapy: a practical guide. Am J Cardiovasc Drugs. 2004;4(1):43–55.
Goldstein JN, Rosand J, Schwamm LH. Warfarin reversal in anticoagulant-associated intracerebral hemorrhage. Neurocrit Care. 2008;9(2):277–83.
Aguilar MI et al. Treatment of warfarin-associated intracerebral hemorrhage: literature review and expert opinion. Mayo Clin Proc. 2007;82(1):82–92.
Ivascu FA et al. Treatment of trauma patients with intracranial hemorrhage on preinjury warfarin. J Trauma. 2006;61(2):318–21.
Ansell J et al. The pharmacology and management of the vitamin K antagonists: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004;126(3 Suppl):204S–33S.
Ansell J et al. Managing oral anticoagulant therapy. Chest. 2001;119(1 Suppl):22S–38S.
Watson HG et al. A comparison of the efficacy and rate of response to oral and intravenous Vitamin K in reversal of over-anticoagulation with warfarin. Br J Haematol. 2001;115(1):145–9.
Fiore LD et al. Anaphylactoid reactions to vitamin K. J Thromb Thrombolysis. 2001;11(2):175–83.
Rashidi A, Tahhan HR. Fresh frozen plasma dosing for warfarin reversal: a practical formula. Mayo Clin Proc. 2013;88(3):244–50.
MacLennan S, Williamson LM. Risks of fresh frozen plasma and platelets. J Trauma. 2006;60(6 Suppl):S46–50.
Hanley JP. Warfarin reversal. J Clin Pathol. 2004;57(11):1132–9.
Huttner HB et al. Hematoma growth and outcome in treated neurocritical care patients with intracerebral hemorrhage related to oral anticoagulant therapy: comparison of acute treatment strategies using vitamin K, fresh frozen plasma, and prothrombin complex concentrates. Stroke. 2006;37(6):1465–70.
Hanger HC et al. Warfarin-related intracerebral haemorrhage: better outcomes when reversal includes prothrombin complex concentrates. Intern Med J. 2012;43(3):308–16.
Hickey M, et al. Outcomes of urgent warfarin reversal using fresh frozen plasma vs prothrombin complex concentrate in the emergency department. Circulation. 2013.
Cabral KP et al. Prothrombin complex concentrates to reverse warfarin-induced coagulopathy in patients with intracranial bleeding. Clin Neurol Neurosurg. 2012;115(6):770–4.
McEvoy GK. AHFS Drug Information, in American Society of Health-System Pharmacists, Inc. Bethesda, MD; 2005.
Mayer SA et al. Efficacy and safety of recombinant activated factor VII for acute intracerebral hemorrhage. N Engl J Med. 2008;358(20):2127–37.
Narayan RK et al. Recombinant factor VIIA in traumatic intracerebral hemorrhage: results of a dose-escalation clinical trial. Neurosurgery. 2008;62(4):776–86. discussion 786–8.
Ilyas C et al. Recombinant factor VIIa for warfarin-associated intracranial bleeding. J Clin Anesth. 2008;20(4):276–9.
Morgenstern LB et al. Guidelines for the management of spontaneous intracerebral hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2010;41(9):2108–29.
Woo CH, et al. Rapid warfarin reversal in the setting of intracranial hemorrhage: a comparison of plasma, Recombinant activated factor VII, and Prothrombin Complex Concentrate. World Neurosurg. 2012. This study provides a comparison of 3 different reversal strategies for warfarin-treated patients with ICH regarding safety and effectiveness.
Valentine KA, Hull RD. Therapeutic use of heparin and low molecular weight heparin. UpToDate. 2012.
Harenberg J et al. Inhibition of low molecular weight heparin by protamine chloride in vivo. Thromb Res. 1985;38(1):11–20.
Hirsh J et al. Parenteral anticoagulants: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008;133(6 Suppl):141S–59S.
Elmer J, Wittels KA. Emergency reversal of pentasaccharide anticoagulants: a systematic review of the literature. Transfus Med. 2011;22(2):108–15.
Eerenberg ES et al. Reversal of rivaroxaban and dabigatran by prothrombin complex concentrate: a randomized, placebo-controlled, crossover study in healthy subjects. Circulation. 2011;124(14):1573–9.
Oh JJ et al. Recombinant factor VIIa for refractory bleeding after cardiac surgery secondary to anticoagulation with the direct thrombin inhibitor lepirudin. Pharmacotherapy. 2006;26(4):569–77.
Thompson BB et al. Prior antiplatelet therapy and outcome following intracerebral hemorrhage: a systematic review. Neurology. 2010;75(15):1333–42.
Ohm C et al. Effects of antiplatelet agents on outcomes for elderly patients with traumatic intracranial hemorrhage. J Trauma. 2005;58(3):518–22.
Spektor S et al. Low-dose aspirin prophylaxis and risk of intracranial hemorrhage in patients older than 60 years of age with mild or moderate head injury: a prospective study. J Neurosurg. 2003;99(4):661–5.
Connolly BJ et al. Aspirin therapy and risk of subdural hematoma: meta-analysis of randomized clinical trials. J Stroke Cerebrovasc Dis. 2013;22(4):444–8. This meta-analysis of studies evaluating the risk of SDH in setting of antiplatelet treatment with aspirin reviews studies since 1980 and provides a great overview over the differences observed depending on patient population and clinical setting.
Powner DJ, Hartwell EA, Hoots WK. Counteracting the effects of anticoagulants and antiplatelet agents during neurosurgical emergencies. Neurosurgery. 2005;57(5):823–31. discussion 823–31.
Jones K et al. The effects of preinjury clopidogrel use on older trauma patients with head injuries. Am J Surg. 2006;192(6):743–5.
Ranucci M et al. Platelet mapping and desmopressin reversal of platelet inhibition during emergency carotid endarterectomy. J Cardiothorac Vasc Anesth. 2007;21(6):851–4.
Wiedemayer H et al. Early seizures following nonpenetrating traumatic brain injury in adults: risk factors and clinical significance. Brain Inj. 2002;16(4):323–30.
Rabinstein AA et al. Seizures after evacuation of subdural hematomas: incidence, risk factors, and functional impact. J Neurosurg. 2009;112(2):455–60.
Swadron SP et al. Emergency neurological life support: traumatic brain injury. Neurocrit Care. 2012;17 Suppl 1:S112–21. This recent protocol was published as part of the Emergency Neurological Life Support Series by the Neurocritical Care Society. The article reviews steps of early intervention for patients with TBI, and provides a protocolized approach to early care for those patients.
Schierhout G, Roberts I. Withdrawn: antiepileptic drugs for preventing seizures following acute traumatic brain injury. Cochrane Database Syst Rev. 6:CD000173.
Temkin NR et al. A randomized, double-blind study of phenytoin for the prevention of post-traumatic seizures. N Engl J Med. 1990;323(8):497–502.
Zafar SN et al. Phenytoin vs Leviteracetam for seizure prophylaxis after brain injury—a meta-analysis. BMC Neurol. 2012;12:30.
Mathew P et al. Acute subdural haematoma in the conscious patient: outcome with initial nonoperative management. Acta Neurochir (Wien). 1993;121(3–4):100–8.
Wong CW. Criteria for conservative treatment of supratentorial acute subdural haematomas. Acta Neurochir (Wien). 1995;135(1–2):38–43.
Koc RK et al. Acute subdural hematoma: outcome and outcome prediction. Neurosurg Rev. 1997;20(4):239–44.
Kotwica Z, Brzezinski J. Acute subdural haematoma in adults: an analysis of outcome in comatose patients. Acta Neurochir (Wien). 1993;121(3–4):95–9.
Leitgeb J et al. Outcome after severe brain trauma due to acute subdural hematoma. J Neurosurg. 2012;117(2):324–33. This study is one of the largest prospective observational studies for assessment and predictors of outcome in moderate and severe TBI with a component of acute SDH.
Cagetti B et al. The outcome from acute subdural and epidural intracranial haematomas in very elderly patients. Br J Neurosurg. 1992;6(3):227–31.
Jamjoom A. Justification for evacuating acute subdural haematomas in patients above the age of 75 years. Injury. 1992;23(8):518–20.
Kotwica Z, Jakubowski JK. Acute head injuries in the elderly. An analysis of 136 consecutive patients. Acta Neurochir (Wien). 1992;118(3–4):98–102.
Busl KM, Mahesh R, Ouyang B, Garg R, Temes RE. Cardiac abnormalities in patients with acute subdural hemorrhage. Neurocritical Care. 2013.
Oertel M et al. Progressive hemorrhage after head trauma: predictors and consequences of the evolving injury. J Neurosurg. 2002;96(1):109–16.
Wong CW. CT and clinical criteria for conservative treatment of supratentorial traumatic intracerebral haematomas. Acta Neurochir (Wien). 1995;135(3–4):131–5.
Haselsberger K, Pucher R, Auer LM. Prognosis after acute subdural or epidural haemorrhage. Acta Neurochir (Wien). 1988;90(3–4):111–6.
Sakas DE, Bullock MR, Teasdale GM. One-year outcome following craniotomy for traumatic hematoma in patients with fixed dilated pupils. J Neurosurg. 1995;82(6):961–5.
Pascual JM, Prieto R. Surgical Management of Severe Closed Head Injury in Adults. In: Quiñones-Hinojosa A, editor. Schmidek and Sweet Operative Neurosurgical Technique. Philadelphia: Elsevier, Inc; 2012. p. 1513–38.
Chen SH et al. Comparison of craniotomy and decompressive craniectomy in severely head-injured patients with acute subdural hematoma. J Trauma. 2011;71(6):1632–6.
Li LM et al. Outcome following evacuation of acute subdural haematomas: a comparison of craniotomy with decompressive craniectomy. Acta Neurochir (Wien). 2012;154(9):1555–61. This study is a recent retrospective analysis of surgically treated acute SDH, comparing craniotomy with decompressive hemicraniectomy by outcome assessment at 6 months.
Woertgen C et al. Comparison of craniotomy and craniectomy in patients with acute subdural haematoma. J Clin Neurosci. 2006;13(7):718–21.
Gooch MR et al. Complications of cranioplasty following decompressive craniectomy: analysis of 62 cases. Neurosurg Focus. 2009;26(6):E9.
Gore PA et al. Normobaric oxygen therapy strategies in the treatment of postcraniotomy pneumocephalus. J Neurosurg. 2008;108(5):926–9.
Reasoner DK et al. The incidence of pneumocephalus after supratentorial craniotomy. Observations on the disappearance of intracranial air. Anesthesiology. 1994;80(5):1008–12.
Ihab Z. Pneumocephalus after surgical evacuation of chronic subdural hematoma: is it a serious complication? Asian J Neurosurg. 2012;7(2):66–74.
Nazzaro JM et al. Head positioning and risk of pneumocephalus, air embolism, and hemorrhage during subthalamic deep brain stimulation surgery. Acta Neurochir (Wien). 2010;152(12):2047–52.
Schirmer CM, Heilman CB, Bhardwaj A. Pneumocephalus: case illustrations and review. Neurocrit Care. 2010;13(1):152–8.
Markham JW. The clinical features of pneumocephalus based upon a survey of 284 cases with report of 11 additional cases. Acta Neurochir (Wien). 1967;16(1):1–78.
Shaikh N, et al. Tension pneumocephalus as complication of burr-hole drainage of chronic subdural hematoma: a case report. Surg Neurol Int. 2010;1.
Thiagarajah S et al. Cardiac arrest associated with tension pneumocephalus. Anesthesiology. 1982;56(1):73–5.
Cipriani NA et al. Air embolism with pneumocephalus. Arch Neurol. 2009;66(9):1172–3.
Lavano A et al. Symptomatic tension pneumocephalus after evacuation of chronic subdural haematoma: report of seven cases. Clin Neurol Neurosurg. 1990;92(1):35–41.
Sharma BS et al. Tension pneumocephalus following evacuation of chronic subdural haematoma. Br J Neurosurg. 1989;3(3):381–7.
Ishiwata Y et al. Subdural tension pneumocephalus following surgery for chronic subdural hematoma. J Neurosurg. 1988;68(1):58–61.
Standefer M, Bay JW, Trusso R. The sitting position in neurosurgery: a retrospective analysis of 488 cases. Neurosurgery. 1984;14(6):649–58.
DelGaudio JM, Ingley AP. Treatment of pneumocephalus after endoscopic sinus and microscopic skull base surgery. Am J Otolaryngol. 2009;31(4):226–30.
Claassen DO et al. Restarting anticoagulation therapy after warfarin-associated intracerebral hemorrhage. Arch Neurol. 2008;65(10):1313–8.
Eckman MH et al. Can patients be anticoagulated after intracerebral hemorrhage? A decision analysis. Stroke. 2003;34(7):1710–6.
Ananthasubramaniam K et al. How safely and for how long can warfarin therapy be withheld in prosthetic heart valve patients hospitalized with a major hemorrhage? Chest. 2001;119(2):478–84.
Amin AG, et al. Postoperative anticoagulation in patients with mechanical heart valves following surgical treatment of subdural hematomas. Neurocrit Care. 2012.
Wijdicks EF et al. The dilemma of discontinuation of anticoagulation therapy for patients with intracranial hemorrhage and mechanical heart valves. Neurosurgery. 1998;42(4):769–73.
Phan TG, Koh M, Wijdicks EF. Safety of discontinuation of anticoagulation in patients with intracranial hemorrhage at high thromboembolic risk. Arch Neurol. 2000;57(12):1710–3.
Acknowledgments
The authors would like to thank Dr. Ricardo Fontes for providing the original photograph images for Fig. 1.
Compliance with Ethics Guidelines
Conflict of Interest
Carter Gerard declares that he has no conflict of interest. Katharina M. Busl declares that she has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with animal subjects performed by any of the authors. With regard to the authors’ research cited in this paper, all procedures were followed in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1975, as revised in 2000 and 2008.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Critical Care Neurology
Rights and permissions
About this article
Cite this article
Gerard, C., Busl, K.M. Treatment of Acute Subdural Hematoma. Curr Treat Options Neurol 16, 275 (2014). https://doi.org/10.1007/s11940-013-0275-0
Published:
DOI: https://doi.org/10.1007/s11940-013-0275-0