Abstract
Nonalcoholic fatty liver disease (NAFLD) and its spectrum ranging from simple steatosis to nonalcoholic steatohepatitis (NASH) and fibrosis have been increasing in the pediatric population. The presence and severity of fibrosis in patients with NAFLD are important prognostic factors for the risk of disease progression to cirrhosis. The gold standard for staging liver fibrosis is a liver biopsy. However, given the risks of this procedure, especially in the pediatric population, the development of noninvasive markers to diagnose and monitor progression of NAFLD is desirable. This paper will review recently developed noninvasive methods for diagnosing liver fibrosis in children with NAFLD. These include simple fibrosis scores, advanced biochemical markers, and radiologic imaging studies. Simple fibrosis scores use readily available laboratory tests; available one include AST/ALT ratio, AST to platelet ratio index (APRI), fibrosis (FIB)-4 index, NAFLD fibrosis score (NFS), pediatric NAFLD fibrosis index (PNFI), and pediatric NALFD fibrosis score (PNFS). Advanced biochemical markers include biomarkers of hepatocyte cell death such as cytokeratin 18 fragment levels, and markers of extracellular matrix turnover such as the Enhanced Liver Fibrosis (ELF) test and hyaluronic acid. Radiologic imaging studies estimate liver stiffness as a surrogate for liver fibrosis; these include transient elastography (TE), magnetic resonance elastography (MRE), and acoustic radiation force impulse imaging (ARFI).

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Aggarwal A, Puri K, Thangada S, Zein N, Alkhouri N. Nonalcoholic fatty liver disease in children: recent practice guidelines, where do they take us? Curr Pediatr Rev. 2014;10(2):151–61.
Schwimmer JB, Deutsch R, Kahen T, Lavine JE, Stanley C, Behling C. Prevalence of fatty liver in children and adolescents. Pediatrics. 2006;118(4):1388–93. This was a landmark study which determined the true prevalence of fatty liver disease in pediatric population for the first time. The authors used a cohort of 742 children aged 2–19 years and determined that fatty liver disease is the most common liver disease in children.
Fraser A, Longnecker MP, Lawlor DA. Prevalence of elevated alanine aminotransferase among US adolescents and associated factors: NHANES 1999-2004. Gastroenterology. 2007;133(6):1814–20.
Burgert TS, Taksali SE, Dziura J, et al. Alanine aminotransferase levels and fatty liver in childhood obesity: associations with insulin resistance, adiponectin, and visceral fat. J Clin Endocrinol Metab. 2006;91(11):4287–94.
Nadeau KJ, Ehlers LB, Zeitler PS, Love-Osborne K. Treatment of non-alcoholic fatty liver disease with metformin versus lifestyle intervention in insulin-resistant adolescents. Pediatr Diabetes. 2009;10(1):5–13.
Kawasaki T, Hashimoto N, Kikuchi T, Takahashi H, Uchiyama M. The relationship between fatty liver and hyperinsulinemia in obese Japanese children. J Pediatr Gastroenterol Nutr. 1997;24(3):317–21.
Xanthakos S, Miles L, Bucuvalas J, Daniels S, Garcia V, Inge T. Histologic spectrum of nonalcoholic fatty liver disease in morbidly obese adolescents. Clin Gastroenterol Hepatol. 2006;4(2):226–32.
Sartorio A, Del Col A, Agosti F, et al. Predictors of non-alcoholic fatty liver disease in obese children. Eur J Clin Nutr. 2007;61(7):877–83.
Feldstein AE, Charatcharoenwitthaya P, Treeprasertsuk S, Benson JT, Enders FB, Angulo P. The natural history of non-alcoholic fatty liver disease in children: a follow-up study for up to 20 years. Gut. 2009;58(11):1538–44. A landmark study in which authors followed their study cohort for up till as long as 20 years and determined that NAFLD can eventually lead to hepatic fibrosis and cirrhosis which was previously unknown.
Carter-Kent C, Yerian LM, Brunt EM, et al. Nonalcoholic steatohepatitis in children: a multicenter clinicopathological study. Hepatology. 2009;50(4):1113–20.
Schwimmer JB, Behling C, Newbury R, et al. Histopathology of pediatric nonalcoholic fatty liver disease. Hepatology. 2005;42(3):641–9. The authors determined that type 1 and type 2 NASH are distinct subtypes of pediatric NAFLD, making them very different entities from adult fatty liver disease.
Angulo P. Long-term mortality in nonalcoholic fatty liver disease: is liver histology of any prognostic significance? Hepatology. 2010;51(2):373–5.
Molleston JP, White F, Teckman J, Fitzgerald JF. Obese children with steatohepatitis can develop cirrhosis in childhood. Am J Gastroenterol. 2002;97(9):2460–2.
Alkhouri N, McCullough AJ. Noninvasive diagnosis of NASH and liver fibrosis within the spectrum of NAFLD. Gastroenterol Hepatol (N Y). 2012;8(10):661–8.
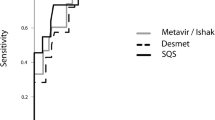
Mansoor S, Yerian L, Kohli R et al. The evaluation of hepatic fibrosis scores in children with nonalcoholic fatty liver disease. Dig Dis Sci. 2014. One of the most recent study published looking at some non-invasive markers of liver fibrosis used in adults and assessing their utilization in pediatrics population with NAFLD.
Yang HR, Kim HR, Kim MJ, Ko JS, Seo JK. Noninvasive parameters and hepatic fibrosis scores in children with nonalcoholic fatty liver disease. World J Gastroenterol. 2012;18(13):1525–30.
Nobili V, Alisi A, Vania A, Tiribelli C, Pietrobattista A, Bedogni G. The pediatric NAFLD fibrosis index: a predictor of liver fibrosis in children with non-alcoholic fatty liver disease. BMC Med 2009;7:21-7015-7-21. The authors of this study proposed PNFI (pediatric NAFLD fibrosis index), which is the first non-invasive marker of hepatic fibrosis to be designed exclusively for pediatric population.
Alkhouri N, Mansoor S, Giammaria P, Liccardo D, Lopez R, Nobili V. The development of the pediatric NAFLD fibrosis score (PNFS) to predict the presence of advanced fibrosis in children with nonalcoholic fatty liver disease. PLoS One. 2014;9(8), e104558.
Feldstein AE, Alkhouri N, De Vito R, Alisi A, Lopez R, Nobili V. Serum cytokeratin-18 fragment levels are useful biomarkers for nonalcoholic steatohepatitis in children. Am J Gastroenterol. 2013;108(9):1526–31.
Lebensztejn DM, Wierzbicka A, Socha P, et al. Cytokeratin-18 and hyaluronic acid levels predict liver fibrosis in children with non-alcoholic fatty liver disease. Acta Biochim Pol. 2011;58(4):563–6.
Nobili V, Alisi A, Torre G, et al. Hyaluronic acid predicts hepatic fibrosis in children with nonalcoholic fatty liver disease. Transl Res. 2010;156(4):229–34.
Guha IN, Parkes J, Roderick P, et al. Noninvasive markers of fibrosis in nonalcoholic fatty liver disease: validating the European liver fibrosis panel and exploring simple markers. Hepatology. 2008;47(2):455–60.
Rosenberg WM, Voelker M, Thiel R, et al. Serum markers detect the presence of liver fibrosis: a cohort study. Gastroenterology. 2004;127(6):1704–13.
Nobili V, Parkes J, Bottazzo G, et al. Performance of ELF serum markers in predicting fibrosis stage in pediatric non-alcoholic fatty liver disease. Gastroenterology. 2009;136(1):160–7. The authors designed this study to validate the use of ELF as a diagnostic marker of liver fibrosis in children and adolescent. Before this study, several studies in adults had shown ELF to be an accurate indicator of liver fibrosis. The group’s findings were promising and called for more pediatric studies for external validation of their results.
Afdhal NH. FibroScan (transient elastography) for the measurement of liver fibrosis. Gastroenterol Hepatol (N Y). 2012;8(9):605–7.
de Ledinghen V, Le Bail B, Rebouissoux L, et al. Liver stiffness measurement in children using FibroScan: feasibility study and comparison with fibrotest, aspartate transaminase to platelets ratio index, and liver biopsy. J Pediatr Gastroenterol Nutr. 2007;45(4):443–50.
Nobili V, Vizzutti F, Arena U, et al. Accuracy and reproducibility of transient elastography for the diagnosis of fibrosis in pediatric nonalcoholic steatohepatitis. Hepatology. 2008;48(2):442–8.
Xanthakos SA, Podberesky DJ, Serai SD, et al. Use of magnetic resonance elastography to assess hepatic fibrosis in children with chronic liver disease. J Pediatr. 2014;164(1):186–8.
Yin M, Talwalkar JA, Glaser KJ, et al. Assessment of hepatic fibrosis with magnetic resonance elastography. Clin Gastroenterol Hepatol. 2007;5(10):1207–13. e2.
Huwart L, Sempoux C, Vicaut E, et al. Magnetic resonance elastography for the noninvasive staging of liver fibrosis. Gastroenterology. 2008;135(1):32–40.
Hanquinet S, Courvoisier D, Kanavaki A, Dhouib A, Anooshiravani M. Acoustic radiation force impulse imaging-normal values of liver stiffness in healthy children. Pediatr Radiol. 2013;43(5):539–44.
Noruegas MJ, Matos H, Goncalves I, Cipriano MA, Sanches C. Acoustic radiation force impulse-imaging in the assessment of liver fibrosis in children. Pediatr Radiol. 2012;42(2):201–4.
Alkhouri N, Sedki E, Alisi A, et al. Combined paediatric NAFLD fibrosis index and transient elastography to predict clinically significant fibrosis in children with fatty liver disease. Liver Int. 2013;33(1):79–85.
Alkhouri N, Carter-Kent C, Lopez R, et al. A combination of the pediatric NAFLD fibrosis index and enhanced liver fibrosis test identifies children with fibrosis. Clin Gastroenterol Hepatol. 2011;9(2):150–5. This study was one of the first studies to assess the combined accuracy of two markers of liver fibrosis in a pediatric cohort, which in their case were PNFI and ELF. Their findings suggested that combination of PNFI and ELF gave the highest accuracy of liver fibrosis on liver biopsy. They also provided a simple clinical algorithm that can be used by clinicians to select patients for biopsy.
Pinto J, Matos H, Nobre S, et al. Comparison of acoustic radiation force impulse/serum noninvasive markers for fibrosis prediction in liver transplant. J Pediatr Gastroenterol Nutr. 2014;58(3):382–6.
Tutar O, Beser OF, Adaletli I, et al. Shear wave elastography in the evaluation of liver fibrosis in children. J Pediatr Gastroenterol Nutr. 2014;58(6):750–5.
Compliance with Ethics Guidelines
Conflict of Interest
Sana Mansoor, Elizabeth Collyer, and Naim Alkhouri declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Pediatric Gastroenterology
Rights and permissions
About this article
Cite this article
Mansoor, S., Collyer, E. & Alkhouri, N. A Comprehensive Review of Noninvasive Liver Fibrosis Tests in Pediatric Nonalcoholic Fatty Liver Disease. Curr Gastroenterol Rep 17, 23 (2015). https://doi.org/10.1007/s11894-015-0447-z
Published:
DOI: https://doi.org/10.1007/s11894-015-0447-z