Abstract
Background and Purpose
Intragastric balloons are used as a treatment for obesity. Much of the data collected on balloons had been in the context of clinical trials in academic medical centers or as a bridge to bariatric surgery in obesity centers. The aim of this study was to investigate the efficacy and safety of balloon treatment in private practice.
Study Design
This is an interventional study.
Subjects
The study included 1600 patients.
Place
The study was conducted at the ElKatib Hospital.
Method
This was a retrospective analysis of 6-month weight loss data and balloon-related complications of patients referred to a private center for obesity treatment.
Assessment
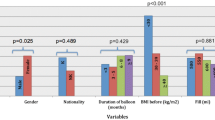
The assessment was carried out by obtaining full patients’ history (personal history, present illness, and previous drug history and operations). Laboratory work was done in the form of CBC, blood sugar, and viral markers. Bioenterics Intragastric Balloon (BIB) silicone balloon was used, filled with saline plus methylene blue dye with a volume ranging from 400 to 700 ml. The gained measures were analyzed by using SPSS program, and paired t test and chi-square test were used to compare between groups.
Results
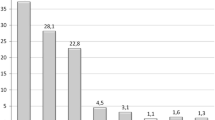
A total of 1600 patients were included (368 male (23%) and 1232 female (77%)) with mean age 34.1 ± 10.354, mean body weight 112.45 ± 26.24, and mean body mass index (BMI) 40.32 ± 8.17. There were 46 patients younger than 18 years and 12 patients older than 60 years. There were 109 patients with a BMI ranging from 25 to < 35 and 737 patients with a BMI ≥ 40 kg/m2. A total of 1567 patients who attended weight consultation had a mean weight loss 17.35 ± 11.07 from intragastric balloon implantation. Thirty-three patients from the total sample were not weighted after the removal of the balloon (dropped out). Percentage excess weight loss (% EWL) = 100% × (baseline absolute weight (AW)−last weight)/(baseline AW−initial body weight (IBW)) was found, and weight loss of more than 10% was considered significant. About 49.3% of patients showed significant weight loss > 10%, 24.7% of patients showed weight loss > 20%, while 26% of patients showed no significant weight loss < 10%.
Conclusion
Intragastric balloons on their own, with an intensive lifestyle program and supportive consultations, resulted in safe and short-term substantial weight loss, and may fill the therapeutic gap between pharmacotherapy and surgery.
Similar content being viewed by others
References
World Health Organization. Obesity: preventing and managing the global epidemic. Report of a WHO consultation on obesity, Geneva, Report no.: WHO/NUT/NCD/98.1 Geneva: WHO; 1998.
Isidro L, Cordido F. Approved and off-label use of obesity medications, and potential new pharmacologic treatment options. Pharmaceuticals. 2010;3:125–45.
Swidnicka-Siergiejko A, Wróblewski E, Dabrowski A. Endoscopic treatment of obesity. Can J Gastroenterol. 2011;25(11):627–33.
Imaz I, Martinez-Cervell C, Garcia-Alvarez EE, et al. Safety and effectiveness of the intragastric balloon for obesity. A meta-analysis. Obes Surg. 2008;18:841–6.
de Moura EG, Orso IR, Martins BC, et al. Improvement of insulin resistance and reduction of cardiovascular risk among obese patients with type 2 diabetes with the duodenojejunal bypass liner. Obes Surg. 2011;21:941–7.
Melissas J, Mouzas J, Filis D, et al. The intragastric balloon – smoothing the path to bariatric surgery. Obes Surg. 2006;16:897–902.
Mathus-Vliegen Elisabeth MH, Alders PRH, Chuttani R, et al. Intragastric balloons in a private practice setting. Gastrointest Endosc. 2015;47:302–7.
Elia PP, Freire A, Silva GC, Teixeira N, Teixeira JM, Feldman G, Moraes CE, Wrobel D and Carvalho G. Efficacy and safety of intragastric balloon for obesity and pre- obese patients: a Brazilian experience gastrointestinal endoscopy. 2010;71(5).
Negrin Dastis S, François E, Deviere J, et al. Intragastric balloon for weight loss: results in 100 individuals followed for at least 2.5 years. Gastrointest Endosc. 2009;41:575–80.
Almeida LS. Results of 700 cases of intragastric balloon. Gastrointest Endosc. 2015;81(5S):AB459.
Uyak D, Galle V. Endoscopic treatment of obesity using a gastric balloon (B.I.B) study data of 101 patients with a BMI of 27 or more with gastric balloon implantations. Gastrointest Endosc. 2010;71(5)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
A Statement of Informed Consent
Informed consent was obtained from all individual participants included in the study.
A Statement of Human Rights
The study has been approved by the ministry of health and the hospital ethics committee and has been performed in accordance with the ethical standards.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Abeid, M., Kaddah, T., Zaitoun, N.A. et al. Efficacy and Safety of Intragastric Balloon Placements in 1600 Case, an Experience from the Middle East. OBES SURG 29, 2087–2091 (2019). https://doi.org/10.1007/s11695-019-03848-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-019-03848-x