Abstract
Background
Sleeve gastrectomy (SG) can be performed either as isolated (ISG), or with the malabsorptive procedure of duodenal switch (SG/DS). Among the postoperative complications, stenosis of the SG is relatively rare and only scarcely mentioned in literature. We report our experience in nine patients presenting a long stenosis, not eligible for endoscopic balloon dilation, and treated by laparoscopic seromyotomy after ISG or SG/DS.
Methods
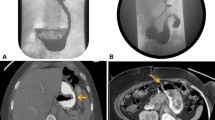
From March 2006 to January 2008, four patients after ISG (0.7%) and five patients after SG/DS (0.8%) were consecutively submitted to laparoscopic seromyotomy for long stenosis, not eligible for endoscopic balloon dilation. Dysphagia appeared after a mean time of 9.2 ± 2.6 months (ISG) and of 18.6 ± 13.2 months (SG/DS). Preoperative mean dysphagia frequency was 4 ± 0 (ISG) and 4 ± 0 (SG/DS). Gastroesophageal reflux disease (GERD) symptoms appeared as de novo in two patients of both groups. Barium swallow showed a stenosis at the upper part of the SG (2) and at the level of the incisura angularis (7). Gastroscopy evidenced a mean length of the stricture of 4.7 ± 0.9 cm (ISG) and of 5.2 ± 1.3 cm (SG/DS). The primary outcomes measure was stricture healing rate. Secondary outcomes measures included procedure time, peroperative, and postoperative complications, performance of barium swallow check, and GERD symptoms improvement.
Results
There were no conversions to open surgery and no mortality. There was no peroperative gastric perforation, but one patient was converted into Roux-en-Y gastric bypass (ISG). Mean operative time was 153.7 ± 39.4 min (ISG) and 110 ± 6.1 min (SG/DS). One gastric leak was recorded postoperatively (ISG). Mean hospital stay was 7.6 ± 5.8 days (ISG) and 3.4 ± 0.8 days (SG/DS). Barium swallow check after 1 month was satisfied in all patients, and they were able to tolerate a regular diet. After a mean follow-up of 21 ± 5.6 months (ISG), the mean dysphagia score was reduced to 0.6 ± 0.9, and after a mean follow-up of 17.6 ± 10.5 months (SG/DS) to 0.8 ± 0.8. De novo GERD symptoms improved in two patients of both groups.
Conclusion
Laparoscopic seromyotomy after SG for long stenosis is feasible, and efficient for the treatment of symptomatic dysphagia. It has a beneficiary influence on de novo GERD symptoms improvement. There is, however, the risk of postoperative leak.



Similar content being viewed by others
References
Deitel M, Crosby RD, Gagner M. The First International Consensus Summit for Sleeve Gastrectomy (SG), New York City, October 25–27, 2007. Obes Surg 2008;18:487–96.
Johnston D, Dachtler J, Sue-Ling HM, et al. The Magenstrasse and Mill operation for morbid obesity. Obes Surg 2003;13:10–6.
Hess DS, Hess DW. Biliopancreatic diversion with duodenal switch. Obes Surg 1998;8:267–82.
Marceau P, Biron S, Bourque RA, et al. Biliopancreatic diversion with a new type of gastrectomy. Obes Surg 1993;3:29–35.
Cottam D, Qureshi FG, Mattar SG, et al. Laparoscopic sleeve gastrectomy as an initial weight loss procedure for high-risk patients with morbid obesity. Surg Endosc 2006;20:859–63.
Hamoui N, Anthone GJ, Kaufman HS, et al. Sleeve gastrectomy in the high-risk patient. Obes Surg 2006;16:1445–9.
Almogy G, Crookes PF, Anthone GJ. Longitudinal gastrectomy as a treatment for the high-risk super-obese patient. Obes Surg 2004;14:492–7.
Silecchia G, Boru C, Pecchia A, et al. Effectiveness of laparoscopic sleeve gastrectomy (first stage of biliopancreatic diversion with duodenal switch) on co-morbidities in super-obese high-risk patients. Obes Surg 2006;16:1138–44.
Milone L, Strong V, Gagner M. Laparoscopic sleeve gastrectomy is superior to endoscopic intragastric balloon as a first stage procedure for super-obese patients (BMI≥50). Obes Surg 2005;15:612–7.
Silecchia G. Rizzello M, Casella G, et al. Two-stage laparoscopic biliopancreatic diversion with duodenal switch as treatment of high-risk super-obese patients: analysis of complications. Surg Endosc. 2008;Sep24 (Epub ahead of print).
Regan JP, Inabnet WB, Gagner M, et al. Early experience with two-stage laparoscopic Roux-en-Y gastric bypass as an alternative the super super-obese patient. Obes Surg 2003;13:861–4.
Serra C, Baltasar A, Andreo L, et al. Treatment of gastric leaks with coated-self-expanding stents after sleeve gastrectomy. Obes Surg 2007;17:866–72.
Eisendrath P, Cremer M, Himpens J, et al. Endotherapy including temporary stenting of fistulas of the upper gastrointestinal tract after laparoscopic bariatric surgery. Endoscopy 2007;39:6225–30.
Baltasar A, Bou R, Bengochea M, et al. Use of a Roux limb to correct esophagogastric junction fistulas after sleeve gastrectomy. Obes Surg 2007;17:1408–10.
Serra C, Baltasar A, Pérez N, et al. Total gastrectomy for complications of the duodenal switch, with reversal. Obes Surg 2006;16:1082–6.
Gagner M, Rogula T. Laparoscopic reoperative sleeve gastrectomy for poor weight loss after biliopancreatic diversion with duodenal switch. Obes Surg 2003;21:1810–6.
Baltasar A, Serra C, Pérez N, et al. Re-sleeve gastrectomy. Obes Surg 2006;16:1535–8.
Gumbs AA, Pomp A, Ganger M. Revisional bariatric surgery for inadequate weight loss. Obes Surg 2007;17:1137–45.
Langer FB, Bohdjalian A, Felberbauer FX, et al. Does gastric dilatation limit the success if sleeve gastrectomy as a sole operation for morbid obesity? Obes Surg 2006;16:166–71.
Parikh M, Gagner M. Laparoscopic hernia repair and repeat sleeve gastrectomy for gastroesophageal reflux disease after duodenal switch. Surg Obes Relat Dis 2008;4:73–5.
Lalor PF, Tucker ON, Szomstein S, et al. Complications after laparoscopic sleeve gastrectomy. Surg Obes Relat Dis 2008;4:33–8.
Mui WL, Ng EK, Tsung BY, et al. Laparoscopic sleeve gastrectomy in ethnic obese chinese. Obes Surg 2008;18(12):1571–4.
Merrell N, McCray RS. Balloon catheter dilation of a severe esophageal stricture. Gastrointest Endosc 1982;28:254–5.
Heller E. Extramukose kardioplastic beim chronischen kardiospasmus mit dilatation des oesophagus. Mitt Grenzeb Med Chir 1913;27:141–9.
Weiner RA, Weiner S, Pomhoff I, et al. Laparoscopic sleeve gastrectomy-influence of sleeve size and resected gastric volume. Obes Surg 2007;17:1297–305.
Tucker ON, Szomstein S, Rosenthal RS. Indications for sleeve gastrectomy as a primary procedure for weight loss in the morbidly obese. J Gastrointest Surg 2008;12:662–7.
Baker RS, Foote J, Kemmeter P, et al. The science of stapling and leaks. Obes Surg 2004;14:1290–8.
Barba CA, Butensky MS, Loenzo M, et al. Endoscopic dilation of gastroesophageal anastomossi stricture after gastric bypass. Surg Endosc 2003;17:416–20.
Ahmad J, Martin J, Ikramuddin S, et al. Endoscopic balloon dilation of gastroenteric anastomotic stricture after laparoscopic gastric bypass. Endoscopy 2003;35:725–8.
Roller JE, de la Fuente SG, Demaria EJ, et al. Laparoscopic Heller myotomy using hook electrocautery: a safe, simple, and inexpensive alternative. Surg Endosc. 2008;Jul 12 (Epub ahead of print).
Eubanks S, Edwards CA, Fearing NM, et al. Use of endoscopic stents to treat anastomotic complications after bariatric surgery. J Am Coll Surg 2008;206:935–8.
Tatum RP, Pellegrini CA. How I do it: laparoscopic Heller myotomy with Toupet fundoplication for achalasia. J Gastrointest Surg. 2008;Jul 12 (Epub ahead of print).
Author information
Authors and Affiliations
Corresponding author
Additional information
This paper has been presented at the XIII World Congress of International Federation for the Surgery of Obesity and Metabolic Disorders, Buenos Aires, September 24–27, 2008.
Rights and permissions
About this article
Cite this article
Dapri, G., Cadière, G.B. & Himpens, J. Laparoscopic Seromyotomy for Long Stenosis After Sleeve Gastrectomy with or Without Duodenal Switch. OBES SURG 19, 495–499 (2009). https://doi.org/10.1007/s11695-009-9803-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-009-9803-0